Save the Date


Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals
You are here
- Volume 14, Issue 5
- How to manage alcohol-related liver disease: A case-based review
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-1530-5328 James B Maurice 1 ,
- http://orcid.org/0000-0001-5140-517X Samuel Tribich 2 ,
- Ava Zamani 3 ,
- Jennifer Ryan 4
- 1 Department of Gastroenterology and Hepatology, Southmead Hospital , North Bristol NHS Trust , Bristol , UK
- 2 Department of Hepatology, Royal London Hospital , Barts Health NHS Trust , London , UK
- 3 Hammersmith Hospital , Imperial College Healthcare NHS Trust , London , UK
- 4 Department of Hepatology and Liver Transplantation, Royal Free Hospital , Royal Free London NHS Foundation Trust , London , UK
- Correspondence to Dr James B Maurice, Department of Gastroenterology and Hepatology, Southmead Hospital, North Bristol NHS Trust, Bristol BS10 5NB, UK; james.maurice{at}nbt.nhs.uk
https://doi.org/10.1136/flgastro-2022-102270
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
- alcoholic liver disease
- chronic liver disease
What is already known on this topic
Alcohol-related liver disease (ArLD) is a major cause of morbidity and mortality.
What this study adds
We present a typical case to illustrate current evidence-based investigation and management of a patient with ArLD.
This case-based review aims to concisely support the day-to-day decision making of clinicians looking after patients with ArLD, from risk stratification and fibrosis assessment in the community through to managing decompensated disease, escalation care to critical care and assessment for liver transplantation.
How this study might affect research, practice or policy
We summarise the evolving evidence for the benefit of liver transplantation in alcoholic hepatitis, and ongoing controversies shaping future research in this area.
ArLD is fundamentally a public health problem, and further efforts are required to implement effective policies to reduce consumption and prevent disease.
Introduction
Alcohol is the leading risk factor for premature death in young adults, of which alcohol-related liver disease (ArLD) is a major contributor. 1 The management of ArLD often requires complex decision-making, raising challenges for the clinician and wider multidisciplinary team. This case-based review follows the typical journey of a patient through the progressive stages of the disease process, from early diagnosis and risk stratification in the outpatient clinic through to alcoholic hepatitis and referral for liver transplantation. At each stage, we discuss a practical approach to clinical management and summarise the underlying evidence base.
Case part 1
A 47-year-old man is referred to the general hepatology clinic from his General Practitioner with abnormal liver function tests, ordered in the community following several episodes of non-specific abdominal pain which subsequently resolved. He is now asymptomatic. The referral states that he drinks one bottle of wine each weekday night and more at the weekends. He is on no regular medication, has no other significant medical history and works in construction. On clinical examination, there are a few …
Twitter @jamesbmaurice
Contributors JBM conceptualised the original article and the case. JBM, ST and AZ drafted the initial version of the manuscript. JBM and ST contributed further editing of various sections. JR provided senior critical review and edited the manuscript. All authors agreed upon the final version.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Linked Articles
- Highlights from this issue UpFront R Mark Beattie Frontline Gastroenterology 2023; 14 357-358 Published Online First: 07 Aug 2023. doi: 10.1136/flgastro-2023-102519
Read the full text or download the PDF:

ANDREW SMITH, MD, KATRINA BAUMGARTNER, MD, AND CHRISTOPHER BOSITIS, MD
Am Fam Physician. 2019;100(12):759-770
Author disclosure: No relevant financial affiliations.
Cirrhosis is the 12th leading cause of death in the United States. Newer research has established that liver fibrosis is a dynamic process and that early cirrhosis may be reversible. Only one in three people with cirrhosis knows they have it. Most patients with cirrhosis remain asymptomatic until the onset of decompensation. When clinical signs, symptoms, or abnormal liver function tests are discovered, further evaluation should be pursued promptly. The most common causes of cirrhosis are viral hepatitis, alcoholic liver disease, and nonalcoholic steatohepatitis. Initial workup includes viral hepatitis serologies, ferritin, transferrin saturation, and abdominal ultrasonography as well as complete blood count, liver function tests, and prothrombin time/international normalized ratio, if not already ordered. Additional testing is based on demographics and risk factors. Common serum and ultrasound-based screening tests to assess fibrosis include the aspartate transaminase to platelet ratio index score, Fibrosis 4 score, FibroTest/FibroSure, nonalcoholic fatty liver fibrosis score, standard ultrasonography, and transient elastography. Generally, noninvasive tests are most useful in identifying patients with no to minimal fibrosis or advanced fibrosis. Chronic liver disease management includes directed counseling, laboratory testing, and ultrasound monitoring. Treatment goals are preventing cirrhosis, decompensation, and death. Varices are monitored with endoscopy and often require prophylaxis with nonselective beta blockers. Ascites treatment includes diuresis, salt restriction, and antibiotic prophylaxis for spontaneous bacterial peritonitis, when indicated. Hepatic encephalopathy is managed with lifestyle and nutritional modifications and, as needed, with lactulose and rifaximin. Hepatocellular carcinoma screening includes ultrasound screening every six months for patients with cirrhosis.
Cirrhosis is a diffuse process of liver damage considered irreversible in its advanced stages. In 2016, more than 40,000 Americans died because of complications related to cirrhosis, making it the 12th leading cause of death in the United States. 1 Recent projections suggest that this number is likely to grow. 2 An estimated 630,000 Americans have cirrhosis, yet less than one in three knows it. 3 Important racial and socioeconomic disparities exist, with prevalence highest among non-Hispanic blacks, Mexican Americans, and those living below the poverty level. 3 Cirrhosis and advanced liver disease cost the United States between $12 billion and $23 billion dollars in health care expenses annually. 4 , 5
WHAT'S NEW ON THIS TOPIC
Estimates suggest that nonalcoholic steatohepatitis will become the leading cause of cirrhosis in U.S. patients awaiting liver transplantation sometime between 2025 and 2035.
Liver biopsy remains the reference standard; however, transient elastography has become more widely available and is rapidly replacing biopsy as the preferred method for liver fibrosis staging.
Newer guidelines suggest targeted screening for esophageal varices in patients with clinically significant portal hypertension rather than screening all patients with cirrhosis.
| , | Expert opinion and consensus guidelines in the absence of clinical trials | |
| Expert opinion and consensus guidelines with low-quality trials | ||
| Randomized controlled trials demonstrate acceptable survival benefits based on clinical criteria and Model for End-Stage Liver Disease results with some variability | ||
| Data from multiple randomized controlled trials demonstrate more benefit than harm regarding patient comfort and reduced hospitalization times | ||
| , , , | Randomized controlled trials and meta-analyses comparing nonselective beta blockers, endoscopic band ligation, and placebo or no therapy, which generally show a reduction in variceal hemorrhage | |
| Low-quality randomized controlled trials that demonstrate less recurrence of hepatic encephalopathy using lactulose and/or rifaximin | ||
| , , , | Multiple randomized controlled trials demonstrate a reduction in bacterial infections as well as mortality | |
| should be screened for gastroesophageal varices with endoscopy. Repeat endoscopy should be performed every one to two years if small varices are found and every two to three years if no varices are found. | Expert opinion, consensus guidelines, and unpublished studies in progress |
The most common causes of cirrhosis in the United States are viral hepatitis (primarily hepatitis C virus [HCV] and hepatitis B virus [HBV]), alcoholic liver disease, and non-alcoholic steatohepatitis. HCV remains the leading cause of cirrhosis in patients awaiting liver transplant. With an increasing prevalence of nonalcoholic fatty liver disease (NAFLD) in the United States, estimates suggest that non-alcoholic steatohepatitis, a severe progression of NAFLD characterized by inflammatory steatohepatitis, will become the leading cause of cirrhosis in patients awaiting liver transplant sometime between 2025 and 2035. 6 , 7 Table 1 lists common etiologies of cirrhosis. 8
| Viral hepatitis (hepatitis B, hepatitis C) |
| Alcoholic liver disease |
| Nonalcoholic fatty liver disease/nonalcoholic steatohepatitis |
| Storage diseases |
| Hemochromatosis |
| Wilson disease |
| Alpha -antitrypsin deficiency |
| Immune mediated |
| Autoimmune hepatitis (types 1, 2, and 3) |
| Primary biliary cholangitis |
| Primary sclerosing cholangitis |
| Immunoglobulin G4 cholangiopathy |
| Cardiovascular |
| Veno-occlusive disease (Budd-Chiari syndrome) |
| Congestive heart failure |
| Hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease) |
| Chronic biliary disease |
| Recurrent bacterial cholangitis |
| Bile duct stenosis |
| Other |
| Medications (e.g., methotrexate, amiodarone) |
| Erythropoietic protoporphyria |
| Sarcoidosis |
| Schistosomiasis |
Pathophysiology and Natural History of Cirrhosis
Chronic liver injury causes inflammation and hepatic fibrosis. Regardless of the cause, this can lead to the formation of fibrous septae and nodules, collapse of liver structures, and distortion of hepatic parenchyma and vascular architecture. Progressive fibrosis and cirrhosis subsequently result in decreased metabolic and synthetic hepatic function, causing a rise in bilirubin and decreased production of clotting factors and thrombopoietin, as well as splenic platelet sequestration, increased portal pressure, and the development of ascites and esophageal varices.
Cirrhosis can result from chronic liver damage of any cause. In patients with the three most common causes of liver disease, 10% to 20% will develop cirrhosis within 10 to 20 years. 9 Factors associated with an increased risk of progression to cirrhosis include increased age, medical comorbidities (particularly patients coinfected with HIV and HCV), and male sex (except in alcoholic liver disease, where females progress more rapidly). 10 The point at which this process becomes irreversible, however, is not clear. Newer research has established that liver fibrosis is a dynamic process and that even early cirrhosis is reversible. 11 Studies have demonstrated biopsy-proven fibrosis improvement rates as high as 88% after antiviral treatment in patients with HBV and HCV and as high as 85% after bariatric surgery in patients with nonalcoholic steatohepatitis. 12 , 13
After cirrhosis is established, a patient may remain clinically stable, or compensated, for years. Patients with compensated cirrhosis caused by HBV, HCV, and alcoholic liver disease develop clinical signs of decompensation, which include ascites, hepatic encephalopathy, jaundice, or bleeding, at a rate of 4% to 10% per year. 14 Variability of disease progression is influenced by the underlying cause and the presence or absence of treatment and ongoing liver injury. The median survival for those with compensated cirrhosis is 12 years, compared with two years once decompensation occurs. 15
Clinical Presentation
Most patients with compensated cirrhosis remain asymptomatic. When symptoms occur, they include fatigue, weakness, loss of appetite, right upper quadrant discomfort, and unexplained weight loss. With the onset of decompensation, patients may report symptoms of impaired liver function such as jaundice, portal hypertension (including ascites and peripheral edema), and hepatic encephalopathy (such as confusion and disordered sleep).
PHYSICAL EXAMINATION
Physical examination findings that may be present in patients with advanced liver disease (cirrhosis) are summarized in Table 2 . 16 , 17 The Stanford Medicine 25 website is a good resource for photos and instructional videos that demonstrate findings associated with cirrhosis ( http://stanfordmedicine25.stanford.edu/the25/liverdisease.html ). 16 , 17
| General | Muscle wasting |
| Central nervous system | Asterixis (tremor of the hand with wrist extension) |
| Drowsiness, confusion | |
| Head | Fetor hepaticus: sweet odor of the breath attributable to increased concentrations of dimethyl sulfide |
| Jaundice: may see yellowing of mucous membranes beneath the tongue | |
| Parotid enlargement | |
| Scleral icterus | |
| Spider nevi | |
| Chest | Gynecomastia |
| Spider nevi | |
| Thinning axillary hair | |
| Abdomen | Ascites |
| Caput medusae (engorged superficial epigastric veins radiating from the umbilicus) | |
| Contracted or enlarged liver | |
| Hemorrhoids | |
| Splenomegaly | |
| Hands and nails | Clubbing |
| Dupuytren contracture (progressive fibrosis of palmar fascia, resulting in limited extension of the fingers) | |
| Palmar erythema | |
| Terry nails (whiteness of proximal half of nail plate) | |
| Genitourinary (male) | Testicular atrophy |
| Lower extremities | Distal erythema |
| Edema | |
| Petechiae |
INITIAL LABORATORY FINDINGS
In early compensated disease, laboratory findings may be normal. Incidentally elevated liver enzymes or evidence of hepatic disease on imaging may prompt the initial suspicion of chronic liver injury. Findings suggestive of cirrhosis include low albumin (less than 3.5 g per dL [35 g per L]), thrombocytopenia (platelet count less than 160 × 10 3 per μL [160 × 10 9 per L]), aspartate transaminase (AST):alanine transaminase (ALT) ratio greater than 1, elevated bilirubin, and a prolonged prothrombin time (PT)/elevated international normalized ratio (INR). 18
Evaluation of Chronic Liver Disease
When chronic liver disease is suspected, a history should be conducted, reviewing any potentially hepatotoxic medications, alcohol consumption, and family history of liver disease. Basic laboratory tests, including complete blood count, ALT, AST, albumin, alkaline phosphatase, gamma-glutamyl transferase, total bilirubin, and PT/INR, should be ordered.
For those with clinical signs or symptoms of liver disease or abnormal liver function test results, regardless of duration, further evaluation to determine the potential etiology should be pursued promptly. 19 , 20 Viral hepatitis serologies, ferritin, transferrin saturation, and abdominal ultrasonography should be performed; complete blood count, liver function tests, and PT/INR should be completed, if not already ordered. If risk factors for NAFLD exist, testing of fasting lipid levels and A1C should be done. For patients with risk factors or demographics with concern for autoimmune hepatitis, antinuclear antibodies and smooth muscle antibodies should be tested. Table 3 lists additional suggested tests based on risk factors and clinical findings. 19 , 21 , 22
| Alcoholic liver disease | Positive screening tests for alcohol use disorder | Aspartate transaminase ≥ 2 times alanine transaminase level in 70% of patients, especially if 3 times |
| History of excessive alcohol intake | Elevated glucose tolerance test and/or mean corpuscular volume [corrected] | |
| Ultrasonography may show fatty change | ||
| Alpha -antitrypsin deficiency | Autosomal recessive trait | Alpha -antitrypsin phenotype |
| European ancestry | ||
| All other evaluations unrevealing | ||
| Autoimmune hepatitis | Young and middle-aged women (in type 1, the most common) | Antinuclear antibody and/or antismooth muscle antibody positive in titers ≥ 1:80 |
| Total serum immunoglobulin G (polyclonal hypergammaglobulinemia > 1.5 times the upper limit of normal supports diagnosis) | ||
| Hemochromatosis | Autosomal recessive trait | Ferritin ≥ 250 to 300 ng per mL in men, ≥ 200 ng per mL in women |
| Northern European ancestry | Transferrin saturation (serum iron × 100/total iron-binding capacity) ≥ 45% | |
| If ferritin or transferrin saturation is abnormal, order human hemochromatosis protein gene mutation analysis | ||
| Nonalcoholic fatty liver disease/nonalcoholic steatohepatitis | Obesity, diabetes mellitus | Lipids, A1C (not needed for diagnosis) |
| Improvement with weight loss | Ultrasonography may show fatty change | |
| May need biopsy to diagnose nonalcoholic steatohepatitis | ||
| Primary biliary cholangitis (primary biliary cirrhosis) | Associated with other autoimmune disorders (80% with Sjögren syndrome; 5% to 10% with autoimmune hepatitis) Middle-aged women | Cholestasis (elevated alkaline phosphatase and glucose tolerance test) Antimitochondrial antibody positive |
| Primary sclerosing cholangitis | Middle-aged men | Cholestasis (elevated alkaline phosphatase and glucose tolerance test) |
| Associated with inflammatory bowel disease (70%) | Perinuclear antineutrophil cytoplasmic antibodies positive in 70% of patients Frequently positive antinuclear antibodies, antismooth muscle antibodies, other antibodies Magnetic resonance cholangiography | |
| Viral hepatitis B (chronic) | Born in endemic country | Hepatitis B surface antigen |
| Hepatitis B core antibody | ||
| If either is positive, order hepatitis B virus DNA | ||
| Viral hepatitis C (chronic) | Born 1945 to 1965 | Anti–hepatitis C virus antibody |
| Specific risk factors for hepatitis C virus | If positive, order hepatitis C virus RNA | |
| Wilson disease | Autosomal recessive trait | Low serum ceruloplasmin |
| Age younger than 40 years with chronic liver disease or fatty liver and negative workup for the above | If abnormal, serum copper, urinary copper excretion, liver biopsy, hepatic tissue copper measurement, and genetic marker testing can be considered | |
| Kayser-Fleischer rings |
Staging Fibrosis and Diagnosing Cirrhosis
Liver fibrosis is scored on a scale from F0 to F4 ( Table 4 ) . 23 Differentiating between significant (F2 or greater) and advanced (F3 or greater) fibrosis and cirrhosis (F4) is difficult even with complete clinical, laboratory, and imaging data because findings are often nonspecific or insensitive. 24 Liver biopsy remains the reference standard for assessing liver fibrosis; however, use of noninvasive methods has become increasingly common in clinical practice. 18
| No fibrosis | F0 |
| Minimal scarring | F1 |
| Positive scarring with extension beyond area containing blood vessels | F2 |
| Bridging fibrosis with connection to other areas of fibrosis | F3 |
| Cirrhosis or advanced liver scarring | F4 |
Noninvasive testing includes serum-based and imaging modalities ( Table 5 25 – 37 ) . Generally, noninvasive tests are most useful in identifying patients with no to minimal fibrosis (F0) or advanced fibrosis (F3 to F4) and are less accurate at distinguishing early or intermediate stages of liver disease (F1 to F2). 24 , 38 They are most beneficial when combined with all available data, accounting for the pretest probability of fibrosis. 24 , 38
| AST to platelet ratio index score | AST, platelets | < 0.5: good NPV (80% in HCV) for significant fibrosis |
| > 2.0: high specificity for cirrhosis in HCV (46% sensitivity, 91% specificity) ; the World Health Organization recommended cutoff for HBV-related cirrhosis in low-resource settings (28% sensitivity, 87% specificity) , | ||
| Fibrosis 4 score | Age, platelets, AST, ALT | < 1.45: good NPV (95% in HCV) for advanced fibrosis |
| > 3.25 (range: 2.67 to 3.60): good PPV for advanced fibrosis/cirrhosis in HCV, HBV, and NAFLD , , | ||
| In HCV with ≥ 3.25, PPV for advanced fibrosis = 82% | ||
| In NAFLD with ≥ 2.67, PPV for advanced fibrosis = 80% | ||
| FibroTest/FibroSure | Alpha -macroglobulin, gamma-glutamyl transferase, haptoglobin, apolipoprotein A-I, bilirubin | < 0.30: good NPV (90%) for advanced fibrosis in NAFLD |
| > 0.48: high specificity for significant fibrosis in HCV (specificity = 85%) and HBV (specificity = 80%) | ||
| > 0.70: high specificity for advanced fibrosis or cirrhosis | ||
| In NAFLD with > 0.70, PPV for advanced fibrosis = 73% | ||
| In HBV with > 0.74, specificity for cirrhosis = 91% | ||
| NAFLD fibrosis score | Age, body mass index, AST, ALT, glucose, platelets, albumin | < −1.455: good NPV (88%) for advanced fibrosis in NAFLD |
| > 0.676: good PPV (82%) for advanced fibrosis in NAFLD | ||
| Transient elastography | Liver stiffness measured in kPa | HCV (> 12.5 kPa): high sensitivity (87%) and specificity (91%) for cirrhosis; very accurate for F2 to F4 when combined with FibroTest |
| HBV (> 9.0 to 12.0 kPa): good sensitivity (83%) and specificity (87%) but may be falsely elevated during flare-up | ||
| NAFLD (> 10.3 kPa): good NPV (98.5%) but lower PPV (56%) | ||
| Ultrasonography | Standard ultrasonography | Hepatic nodularity specific for severe fibrosis or cirrhosis in all forms of liver disease (sensitivity = 54%, specificity = 95%) |
| Evidence of portal hypertension (splenomegaly, portosystemic collaterals) |
Most serum tests show indirect markers of liver damage, except hyaluronic acid (found in the liver's extracellular matrix), which is included in biomarker panels such as FibroMeter or Hepascore. 24 The AST to platelet ratio index (APRI; https://www.mdcalc.com/ast-platelet-ratio-index-apri ), Fibrosis 4 score ( http://gihep.com/calculators/hepatology/fibrosis-4-score/ ), and NAFLD fibrosis score ( http://nafldscore.com/ ) are accessible, serum-based, nonproprietary calculations. 18 , 39 FibroTest (FibroSure in the United States), FibroMeter, and Hepascore are patented calculations using several serum biomarkers, with FibroTest being the most validated. 24
Biomarkers are most validated in chronic HCV, 40 with the exception of the NAFLD fibrosis score for non-alcoholic steatohepatitis. 33 For other etiologies of liver disease, including alcoholic liver disease, few studies of noninvasive methods exist.
STANDARD ULTRASONOGRAPHY
Given its relatively low cost, accessibility, and lack of radiation, ultrasonography is useful for diagnosing cirrhosis, cirrhosis complications (e.g., splenomegaly, portal hypertension, ascites, hepatocellular carcinoma), and comorbid liver diseases (e.g., extrahepatic cholestasis). 24 Ultrasonography is good at detecting steatosis (94% sensitivity, 84% specificity), but it may frequently miss fibrosis or cirrhosis (for which it is 40% to 57% sensitive). 41 , 42 Characteristics of cirrhosis include hepatic nodularity, coarseness, and echogenicity, 24 with hepatic nodularity being the most specific. 36 Additionally, features consistent with portal hypertension, such as splenomegaly and portosystemic collaterals, are suggestive of cirrhosis. 37 Patients with cirrhosis and some with chronic HBV should undergo right upper quadrant ultrasonography every six months to screen for hepatocellular carcinoma. 43
TRANSIENT ELASTOGRAPHY
Transient elastography, which has become more widely available, is rapidly replacing biopsy as the preferred method for fibrosis staging. Transient elastography, an ultrasound technique performed with a specialized machine (Fibro-Scan), determines liver stiffness in kilopascals (kPa) by measuring the velocity of low-frequency elastic shear waves propagating through the liver. It is a five-minute procedure performed in an outpatient setting and provides point-of-care results. In a meta-analysis of more than 10,000 patients spanning multiple etiologies of liver disease, transient elastography was sensitive (81%) and specific (88%) for detecting liver fibrosis and cirrhosis 40 (see Table 5 25 – 37 for cutoff values). Transient elastography performs better than the biomarker-based tools in detecting cirrhosis and is accurate at excluding cirrhosis (negative predictive value greater than 90%). 38 Similar to serum tests, however, transient elastography is less accurate at distinguishing between intermediate stages of liver disease, and cutoff values vary depending on the etiology of liver disease and population studied. 24 , 38
LIMITATIONS
Abnormal serum results may be seen from non–liver-related causes, including bone marrow disease, hemolysis, and medications. Transient elastography is less reliable in patients with obesity (though an extra-large probe has been developed), ascites, excessive alcohol intake, and extrahepatic cholestasis. If performed during an episode of acute hepatic inflammation, these tests can also lead to falsely elevated results. 38
LIVER BIOPSY
Liver biopsy remains the reference standard in diagnosing cirrhosis; however, a 20% error rate still occurs in fibrosis staging. 44 Pathologic changes may be heterogeneous; therefore, sampling error is common, and interpretation should be made by an experienced pathologist using validated scoring systems. 38 Liver biopsy is recommended when concern for fibrosis remains after indeterminate or conflicting clinical, laboratory, and imaging results; in those for whom transient elastography is not suitable; or to clarify etiology of disease after inconclusive noninvasive evaluation. 9 Liver biopsy may be indicated to diagnose necroinflammation (in HBV) and steatohepatitis (nonalcoholic steatohepatitis) because they are not easily distinguished by noninvasive methods.
Staging Cirrhosis
After the diagnosis of cirrhosis is established, Child-Pugh ( https://www.mdcalc.com/child-pugh-score-cirrhosis-mortality ) and Model for End-Stage Liver Disease ( https://www.mdcalc.com/meld-score-model-end-stage-liver-disease-12-older ) scores should be used to identify the stage of cirrhosis and mortality risk, respectively. 9 , 45 A Child-Pugh grade B classification (seven to nine points) is consistent with early hepatic decompensation, 46 whereas a Model for End-Stage Liver Disease score of 12 or more is predictive of increased risk for cirrhosis complications. 9
Cirrhosis Management
The primary goals of liver disease management are to prevent cirrhosis complications, liver decompensation, and death. These goals are accomplished with rigorous prevention counseling, monitoring, and management by primary care physicians, in consultation with subspecialists as needed.
PREVENTION COUNSELING
For all patients with liver disease, counseling points should be discussed, including avoidance of alcohol; maintenance of a healthy weight; nutrition; medication and supplement review; prevention of infections (including receiving vaccinations); screening and treatment of causative factors; and avoidance of unnecessary surgical procedures. Table 6 provides more details on counseling for patients with chronic liver disease. 7 , 9 , 18 , 21 , 45 , 47 – 52
| Alcohol use | Brief physician counseling, behavioral counseling, and group support |
| Complete alcohol abstinence in cirrhosis | |
| Medication-assisted treatment for alcohol use disorder | |
| Avoid naltrexone and acamprosate in patients with Child-Pugh grade C cirrhosis , | |
| Baclofen (Lioresal), 5 mg three times daily for three days, then 10 mg three times daily can be used, even with ascites , | |
| Avoidance of unnecessary surgical procedures | Cirrhosis, especially if decompensated or with Model for End-Stage Liver Disease score ≥ 14, increases perioperative mortality risk ; an online calculator has been developed to help guide decision-making ( ) |
| Coffee consumption | Three to four cups of coffee per day may reduce the risk of hepatocellular carcinoma and fibrosis progression in patients with nonalcoholic fatty liver disease and hepatitis C virus infection |
| Infection prevention: bacterial exposures | Avoid exposure to brackish/salt water and consumption of raw seafood ( can be fatal in patients with cirrhosis, iron overload, or immunocompromise) |
| Avoid unpasteurized dairy (risk of serious infections in patients with cirrhosis) | |
| Infection prevention: vaccinations | All patients with liver disease should receive yearly influenza vaccinations and hepatitis A and B vaccinations if not known to be immune |
| In patients with cirrhosis and chronic hepatitis B virus infection, 23-valent pneumococcal polysaccharide vaccine (Pneumovax 23) is recommended | |
| Medication and supplement review | For patients with cirrhosis |
| Analgesics: acetaminophen preferred, limit to 2 g per day 7; nonsteroidal anti-inflammatory drugs contraindicated , ; low-dose tramadol may be used for severe symptoms of pain | |
| Antihypertensives: discontinue if patient has hypotension or ascites (linked to hepatorenal syndrome and mortality) | |
| Aspirin: low-dose aspirin may be continued if cardiovascular disease severity exceeds the severity of cirrhosis | |
| Metformin: should be continued for patients with diabetes mellitus | |
| Proton pump inhibitors: avoid unnecessary use (linked to increased risk of spontaneous bacterial peritonitis) | |
| Sedating medications: avoid benzodiazepines and opiates, especially in hepatic encephalopathy; hydroxyzine or trazodone may be considered for severe insomnia | |
| Statins: may be safely used | |
| Supplements: avoid daily dosage of vitamin A > 5,000 IU (may increase fibrosis production); avoid multivitamins with iron | |
| Obesity and diabetes management | Maximize obesity and diabetes management because they increase the risk of cirrhosis , |
| Weight loss of 10% improves histopathologic features of nonalcoholic steatohepatitis, including fibrosis | |
| Screening for and treatment of underlying causative factors of liver disease | Treatment of alcohol use disorder, chronic hepatitis B or C virus infection, and nonalcoholic fatty liver disease can prevent progression and complications of liver disease and can improve fibrosis levels, even in patients with cirrhosis |
MONITORING OF PATIENTS WITH CIRRHOSIS
For patients with cirrhosis, a basic metabolic panel, liver function tests, complete blood count, and PT/INR should be completed every six months to recalculate Child-Pugh and Model for End-Stage Liver Disease scores. Patients with a Model for End-Stage Liver Disease score of 15 or higher should be referred for liver transplantation evaluation 37 , 45 ; patients with ascites, hepatic encephalopathy, or variceal hemorrhage should also be referred. 37 , 53
Screening and Management for Specific Complications
Patients with cirrhosis are at risk of multiple complications, including hepatic decompensation, hepatocellular carcinoma, and other more common conditions (e.g., malnutrition, leg cramps, umbilical hernias). Table 7 includes specific recommendations for the screening and management of select complications of cirrhosis. 7 , 9 , 43 , 45 , 46 , 49 , 53 – 55
| Abdominal hernia | Clinical | Defer surgery until medically optimized and ascites controlled | High perioperative risk and hernia recurrence in presence of ascites |
| Increased risk with ascites | Consult with multidisciplinary team | ||
| Surgeon with experience in the care of patients with cirrhosis is best | |||
| Ascites | Clinical Paracentesis if new-onset moderate to severe ascites or if concern for spontaneous bacterial peritonitis | Moderate (grade 2) and severe (grade 3) ascites: Diuresis with mineralocorticoids for treatment and prophylaxis Salt restriction < 2 g per day 7; no added salt; avoid preprepared meals , Fluid restriction usually not helpful Large (grade 3) ascites: Paracentesis: large-volume paracentesis with albumin infusion | Spironolactone, 100 mg per day Titrate every three days to maximum of 400 mg daily Goal of no more than 1.1 to 2.2 lb (0.5 to 1 kg) daily of weight loss Add furosemide (Lasix; or torsemide [Demadex]) if not responsive to spironolactone alone or if limiting adverse effects occur (e.g., hyperkalemia , ) Decrease to lowest effective dosage |
| Esophageal varices | EGD at diagnosis of cirrhosis May defer EGD if compensated, transient elastography with liver stiffness < 20 kPa, and platelets > 150,000 per mm (< 5% probability of high-risk varices) Repeat EGD if decompensation develops; if no varices (every two to three years ); if small varices (every one to two years ); or if medium or large varices or high-risk timing of repeat EGD varies | Medium, large, or high-risk varices (red wale markings): Endoscopic band ligation or nonselective beta blocker for prophylaxis , , , Prophylaxis with nonselective beta blocker should be indefinite | Propranolol, 20 to 40 mg twice daily; maximum: 160 to 320 mg per day Nadolol (Corgard), 20 to 40 mg daily; maximum: 80 to 160 mg per day Carvedilol (Coreg), 6.25 mg daily; maximum: 12.5 mg per day Titrate every two to three days; goal 25% heart rate reduction, keep heart rate > 55 beats per minute , , Discontinue if hemodynamic instability: sepsis, spontaneous bacterial peritonitis, acute gastrointestinal bleeding, refractory ascites, systolic blood pressure < 90 mm Hg, sodium concentration < 120 to 130 mEq per L (120 to 130 mmol per L), or acute kidney injury , |
| Hepatic encephalopathy | Clinical | Reverse precipitants | Lactulose syrup, 25 mL every one to two hours until two soft bowel movements per day Titrate to two to three soft bowel movements per day Rifaximin, 550 mg orally twice per day , |
| Exclude other causes | Nutritional support | ||
| Ammonia levels should not be used for diagnosis or monitoring , | Medications First episode: lactulose for treatment and prophylaxis Second episode: add rifaximin (Xifaxan) for prophylaxis | ||
| Hepatocellular carcinoma | Right upper quadrant ultrasonography every six months for all patients with cirrhosis and in certain patients with chronic hepatitis B virus infection without cirrhosis , | Treat obesity, nonalcoholic steatohepatitis, nonalcoholic fatty liver disease, diabetes mellitus, and hepatitis B virus infection | Refer to hepatologist for suspicious findings |
| Leg cramps | Clinical | Manage electrolytes | Baclofen, 10 mg per day, titrate weekly up to 30 mg per day |
| Especially if taking diuretics | Baclofen (Lioresal) as needed and tolerated | ||
| Malnutrition | Clinical | Multivitamin | Avoid protein restriction, even during hepatic encephalopathy Because of the increased risk of osteoporosis in chronic cholestasis and cirrhosis, performing a bone mineral density scan at the time of liver disease diagnosis or liver transplantation evaluation should be considered |
| Especially if new hepatic encephalopathy | Small frequent meals and late-night snack | ||
| Protein intake of 1 to 1.5 g per kg per day, with supplementation as needed , | |||
| Consider bone mineral density scan | |||
| Spontaneous bacterial peritonitis | Clinical Paracentesis if suspicion of disease (new or worsening ascites, gastrointestinal bleeding, hemodynamic instability, fever or signs of systemic inflammation, gastrointestinal symptoms, worsening liver or kidney function, new or worsening hepatic encephalopathy) Diagnosis Ascitic fluid neutrophil count > 250 per mm | Treatment (empiric, IV antibiotics): Community-acquired bacterial peritonitis: third-generation cephalosporin or piperacillin/tazobactam (Zosyn) Prophylaxis per criteria: Ceftriaxone IV if acute gastrointestinal bleeding and Child-Pugh grade B/C Trimethoprim/sulfamethoxazole or ciprofloxacin oral if acute gastrointestinal bleeding and Child-Pugh grade A [corrected] History of spontaneous bacterial peritonitis, ascitic protein < 1.5 g per dL and advanced liver disease (Child-Pugh score ≥ 9 or bilirubin ≥ 3 mg per dL) or kidney disease (creatinine ≥ 1.2 mg per dL, sodium ≤ 130 mmol per L) , , , | Treatment dosing: Cefotaxime, 2 g IV every eight to 12 hours Ceftriaxone, 2 g IV every 24 hours Piperacillin/tazobactam, 3.375 g IV every six hours Prophylactic dosing: Ceftriaxone, 1 g IV per day for seven days Trimethoprim/sulfamethoxazole, one 800-mg/160-mg tablet per day Ciprofloxacin, 500 mg per day Norfloxacin, 400 mg per day (not available in United States) Routine use of antibiotic prophylaxis in ascites without spontaneous bacterial peritonitis or acute gastrointestinal bleeding is not recommended |
COMMON COMPLICATIONS IN DECOMPENSATED CIRRHOSIS
Ascites, which develops in 5% to 10% of patients with cirrhosis per year, leads to decreased quality of life, frequent hospitalizations, and directly increases risk of further complications such as spontaneous bacterial peritonitis, umbilical hernias, and respiratory compromise. It also portends a poor prognosis, with a 30% five-year survival. 53 Hepatic encephalopathy, which occurs in 5% to 25% of patients within five years of a cirrhosis diagnosis, is likewise associated with increased medical cost and mortality, with a reported 15% inpatient mortality rate. 54
SCREENING FOR VARICES
Portal hypertension predisposes patients with cirrhosis to develop esophageal varices. Patients with varices have a one in three chance of developing a variceal bleed in the two years after diagnosis, with a 20% to 40% mortality rate per episode. 45 Endoscopy is the preferred screening method for esophageal varices. Many experts and guidelines recommend screening all patients with cirrhosis 9 ; however, newer recommendations suggest targeted screening of patients with clinically significant portal hypertension. 46 A liver stiffness greater than 20 kPa, alone or combined with a low platelet count (less than 150,000 per mm 3 ) and increased spleen size, and/or the presence of portosystemic collaterals on imaging may be sufficient to diagnose clinically significant portal hypertension and warrant endoscopic screening for varices. Repeat endoscopy should be performed every one to two years if small varices are found and every two to three years if no varices are found. 46
Consultation
Varices, hepatic encephalopathy, and ascites herald hepatic decompensation; these conditions warrant referral for subspecialist evaluation. The management of acute or refractory complications of cirrhosis (e.g., spontaneous bacterial peritonitis, acute gastrointestinal bleeding, hepatorenal syndrome, unresponsive portal hypertension, hepatic encephalopathy, ascites) is best addressed in the inpatient or referral setting.
This article updates previous articles on this topic by Starr and Raines , 56 Heidelbaugh and Bruderly , 57 and Riley and Bhatti . 58
Data Sources: A literature search was completed in Medline via Ovid, EBSCOhost, DynaMed, and the Cochrane Database of Systematic Reviews using the keywords cirrhosis, end stage liver disease, management of liver disease, and liver fibrosis staging. Additionally, the EE+Evidence Summary literature search sent by the AFP medical editors was reviewed. Search dates: November 26, 2018; December 27, 2018; and August 7, 2019.
Kochanek KD, Murphy S, Xu J, et al. Mortality in the United States, 2016. NCHS Data Brief. 2017(293):1-8.
Best AF, Haozous EA, Berrington de Gonzalez A, et al. Premature mortality projections in the USA through 2030: a modelling study [published correction appears in Lancet Public Health . 2018;3(8):e364]. Lancet Public Health. 2018;3(8):e374-e384.
Scaglione S, Kliethermes S, Cao G, et al. The epidemiology of cirrhosis in the United States: a population-based study. J Clin Gastroenterol. 2015;49(8):690-696.
Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018 [published correction appears in Gastroenterology . 2019;156(6):1936]. Gastroenterology. 2019;156(1):254-272.e11.
National Institute of Diabetes and Digestive and Kidney Diseases. The burden of digestive diseases in the United States. January 2008. Accessed January 4, 2019. https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/burden-of-digestive-diseases-in-united-states
Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547-555.
Ge PS, Runyon BA. Treatment of patients with cirrhosis. N Engl J Med. 2016;375(8):767-777.
Wiegand J, Berg T. The etiology, diagnosis and prevention of liver cirrhosis: part 1 of a series on liver cirrhosis. Dtsch Arztebl Int. 2013;110(6):85-91.
National Institute for Health and Care Excellence. Cirrhosis in over 16s: assessment and management. NICE guideline [NG50]. July 2016. Accessed May 28, 2019. https://www.nice.org.uk/guidance/ng50
Poynard T, Mathurin P, Lai CL, et al.; PANFIBROSIS Group. A comparison of fibrosis progression in chronic liver diseases. J Hepatol. 2003;38(3):257-265.
Bonis PA, Friedman SL, Kaplan MM. Is liver fibrosis reversible?. N Engl JMed. 2001;344(6):452-454.
Jung YK, Yim HJ. Reversal of liver cirrhosis: current evidence and expectations. Korean J Intern Med. 2017;32(2):213-228.
Lassailly G, Caiazzo R, Buob D, et al. Bariatric surgery reduces features of nonalcoholic steatohepatitis in morbidly obese patients. Gastroenterology. 2015;149(2):379-388.
Asrani SK, Kamath PS. Natural history of cirrhosis. Curr Gastroenterol Rep. 2013;15(2):308.
D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44(1):217-231.
Stanford Medicine. Liver disease, head to foot. Accessed January 4, 2019. http://stanfordmedicine25.stanford.edu/the25/liverdisease.html
Reuben A. The liver has a body—a Cook's tour. Hepatology. 2005;41(2):408-415.
Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis?. JAMA. 2012;307(8):832-842.
Oh RC, Hustead TR, Ali SM, et al. Mildly elevated liver transaminase levels: causes and evaluation. Am Fam Physician. 2017;96(11):709-715. Accessed August 28, 2019. https://www.aafp.org/afp/2017/1201/p709.html
Newsome PN, Cramb R, Davison SM, et al. Guidelines on the management of abnormal liver blood tests. Gut. 2018;67(1):6-19.
O'Shea RS, Dasarathy S, McCullough AJ Practice Guideline Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Alcoholic liver disease. Hepatology. 2010;51(1):307-328.
Bacon BR, Adams PC, Kowdley KV, et al.; American Association for the Study of Liver Diseases. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54(1):328-343.
Wilkins T, Akhtar M, Gititu E, et al. Diagnosis and management of hepatitis C. Am Fam Physician. 2015;91(12):835-842. Accessed August 28, 2019. https://www.aafp.org/afp/2015/0615/p835.html
Lurie Y, Webb M, Cytter-Kuint R, et al. Non-invasive diagnosis of liver fibrosis and cirrhosis. World J Gastroenterol. 2015;21(41):11567-11583.
Lin ZH, Xin YN, Dong QJ, et al. Performance of the aspartate aminotransferase-to-platelet ratio index for the staging of hepatitis C-related fibrosis: an updated meta-analysis. Hepatology. 2011;53(3):726-736.
Parikh P, Ryan JD, Tsochatzis EA. Fibrosis assessment in patients with chronic hepatitis B virus (HBV) infection. Ann Transl Med. 2017;5(3):40.
World Health Organization. Guidelines for the prevention, care and treatment of persons with chronic hepatitis B infection. March 2015. Accessed January 4, 2019. https://www.who.int/hiv/pub/hepatitis/hepatitis-b-guidelines/en/
Vallet-Pichard A, Mallet V, Nalpas B, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. Comparison with liver biopsy and Fibrotest. Hepatology. 2007;46(1):32-36.
Shah AG, Lydecker A, Murray K, et al.; Nash Clinical Research Network. Comparison of noninvasive markers of fibrosis in patients with non-alcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7(10):1104-1112.
Ratziu V, Massard J, Charlotte F, et al.; LIDO Study Group; CYTOL Study Group. Diagnostic value of biochemical markers (FibroTest-FibroSURE) for the prediction of liver fibrosis in patients with non-alcoholic fatty liver disease. BMC Gastroenterol. 2006;6:6.
Imbert-Bismut F, Ratziu V, Pieroni L, et al.; MULTIVIRC Group. Biochemical markers of liver fibrosis in patients with hepatitis C virus infection: a prospective study. Lancet. 2001;357(9262):1069-1075.
Salkic NN, Jovanovic P, Hauser G, et al. FibroTest/Fibrosure for significant liver fibrosis and cirrhosis in chronic hepatitis B: a meta-analysis. Am J Gastroenterol. 2014;109(6):796-809.
Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45(4):846-854.
Castéra L, Vergniol J, Foucher J, et al. Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology. 2005;128(2):343-350.
Hashemi SA, Alavian SM, Gholami-Fesharaki M. Assessment of transient elastography (FibroScan) for diagnosis of fibrosis in non-alcoholic fatty liver disease: a systematic review and meta-analysis. Caspian J Intern Med. 2016;7(4):242-252.
Colli A, Fraquelli M, Andreoletti M, et al. Severe liver fibrosis or cirrhosis: accuracy of US for detection—analysis of 300 cases. Radiology. 2003;227(1):89-94.
Martin P, DiMartini A, Feng S, et al. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59(3):1144-1165.
European Association for Study of Liver; Asociacion Latinoamericana para el Estudio del Higado. EASL-ALEH Clinical Practice Guidelines: non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol. 2015;63(1):237-264.
Noureddin M, Loomba R. Nonalcoholic fatty liver disease: indications for liver biopsy and noninvasive biomarkers. Clin Liver Dis (Hoboken). 2012;1(4):104-107.
Geng XX, Huang RG, Lin JM, et al. Transient elastography in clinical detection of liver cirrhosis: a systematic review and meta-analysis. Saudi J Gastroenterol. 2016;22(4):294-303.
Bonekamp S, Kamel I, Solga S, et al. Can imaging modalities diagnose and stage hepatic fibrosis and cirrhosis accurately?. J Hepatol. 2009;50(1):17-35.
Saverymuttu SH, Joseph AE, Maxwell JD. Ultrasound scanning in the detection of hepatic fibrosis and steatosis. Br Med J (Clin Res Ed). 1986;292(6512):13-15.
Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68(2):723-750.
Afdhal NH. Diagnosing fibrosis in hepatitis C: is the pendulum swinging from biopsy to blood tests?. Hepatology. 2003;37(5):972-974.
Herrera JL, Rodríguez R. Medical care of the patient with compensated cirrhosis. Gastroenterol Hepatol (N Y). 2006;2(2):124-133.
Garcia-Tsao G, Abraldes JG, Berzigotti A, et al. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the Study of Liver Diseases [published correction appears in Hepatology . 2017;66(1):304]. Hepatology. 2017;65(1):310-335.
Addolorato G, Mirijello A, Leggio L, et al. Management of alcohol dependence in patients with liver disease. CNS Drugs. 2013;27(4):287-299.
Addolorato G, Leggio L, Ferrulli A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet. 2007;370(9603):1915-1922.
Runyon BA. Management of adult patients with ascites due to cirrhosis: update 2012. Accessed August 20, 2019. https://www.aasld.org/sites/default/files/2019-06/141020_Guideline_Ascites_4UFb_2015.pdf
Wadhawan M, Anand AC. Coffee and liver disease. J Clin Exp Hepatol. 2016;6(1):40-46.
Zhang X, Harmsen WS, Mettler TA, et al. Continuation of metformin use after a diagnosis of cirrhosis significantly improves survival of patients with diabetes. Hepatology. 2014;60(6):2008-2016.
Glass LM, Dickson RC, Anderson JC, et al. Total body weight loss of ≥ 10% is associated with improved hepatic fibrosis in patients with non-alcoholic steatohepatitis. Dig Dis Sci. 2015;60(4):1024-1030.
European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis [published correction appears in J Hepatol . 2018;69(5):1207]. J Hepatol. 2018;69(2):406-460.
Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60(2):715-735.
Terrault NA, Lok AS, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67(4):1560-1599.
Starr SP, Raines D. Cirrhosis: diagnosis, management, and prevention. Am Fam Physician. 2011;84(12):1353-1359. Accessed August 28, 2019. https://www.aafp.org/afp/2011/1215/p1353.html
Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: part I. Diagnosis and evaluation. Am Fam Physician. 2006;74(5):756-762. Accessed August 28, 2019. https://www.aafp.org/afp/2006/0901/p756.html
Riley TR, Bhatti AM. Preventive strategies in chronic liver disease: part II. Cirrhosis. Am Fam Physician. 2001;64(10):1735-1740. Accessed August 28, 2019. https://www.aafp.org/afp/2001/1115/p1735.html
Continue Reading
More in AFP
More in pubmed.
Copyright © 2019 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
Cirrhosis of the Liver Ch. 44 Case Study
Published by Elfreda Cunningham Modified over 9 years ago
Similar presentations
Presentation on theme: "Cirrhosis of the Liver Ch. 44 Case Study"— Presentation transcript:

Hepatocirrhosis Liver cirrhosis.

Gallbladder Disease Candice W. Laney Spring 2014.
HEPATIC FAILURE TITO A. GALLA. HEALTHY LIVER LIVER FUNCTION METABOLISM DETOXIFICATION PROCESS PROTEIN SYNTHESIS MANUFACTURE OF CLOTTING FACTOR.

Pancreatitis Acute pancreatitis. Definition Is an inflamation of the pancreas ranging from mild edema to extensive hemorrhage the structure and function.

: foul mouth odor, bad breath Etiology: poor dental hygiene, lung or intestinal disorder S/S: bad breath TX: proper dental hygiene,
Cirrhosis of the Liver. Hepatic Cirrhosis It is a chronic progressive disease characterized by: - replacement of normal liver tissue with diffuse fibrosis.
Hepatic Working knowledge of physiological changes during disease process & effects on nutrition care.
Cirrhosis Biol E-163 TA session 1/8/06. Cirrhosis Fibrosis (accumulation of connective tissue) that progresses to cirrhosis Replacement of liver tissue.
CDI Education Cirrhosis 4/17/2017.
Gastrointestinal Pathophysiology II Pancreas and Liver Nancy Long Sieber Ph.D. December 13, 2010.
Cirrhosis of the Liver Kayla Shoaf.
Cirrhosis of the Liver (relates to Chapter 42, “Nursing Management: Liver, Biliary Tract, and Pancreas Problems,” in the textbook)
Liver pathology: CIRRHOSIS
Liver Cirrhosis S. Diana Garcia
HEPATIC DISORDERS NUR – 224. LEARNING OUTCOMES Explain liver function tests. Relate jaundice, portal hypertension, ascites, varices, nutritional deficiencies.
Hepatic Encephalopathy in End-Stage Liver Disease Megan Dudley End of Life Care for Adults and Families The University of Iowa College of Nursing 1.
Liver, Gall Bladder, and Pancreatic Disease. Manifestations of Liver Disease Inflammation - Hepatitis –Elevated AST, ALT –Steatosis –Enlarged Liver Portal.
Pre and Post Operative Nursing Management
By: Michelle Russell Case Study Presentation NUR 4216L
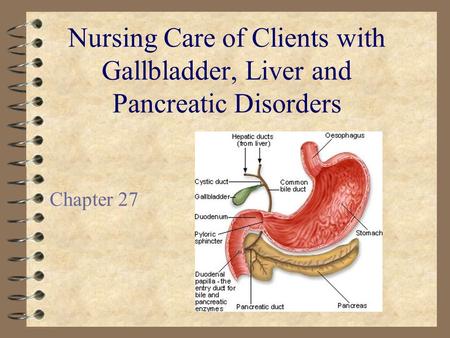
Nursing Care of Clients with Gallbladder, Liver and Pancreatic Disorders Chapter 27.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.

Understanding Liver Cirrhosis: Causes, Symptoms, and Treatment Options
Apr 11, 2023
120 likes | 201 Views
Liver cirrhosis is a chronic liver disease that results in scarring and damage to liver tissue, affecting liver function and overall health. Learn about the causes, symptoms, and treatment options available to manage this condition.<br><br>TO know more check here : https://www.livertransplantinternational.com/liver-cirrhosis/
Share Presentation

Presentation Transcript
Understanding Liver Cirrhosis
Introduction • Definition of liver cirrhosis • Causes of liver cirrhosis • Symptoms of liver cirrhosis • Importance of early detection and treatment
What is Liver Cirrhosis? • A chronic liver disease that results in scarring and damage to liver tissue • Scar tissue replaces healthy liver tissue, making it difficult for the liver to function properly • Liver function is critical to overall health and well-being
Causes of Liver Cirrhosis • Alcohol abuse • Hepatitis B and C • Non-alcoholic fatty liver disease • Autoimmune disorders • Inherited diseases
Symptoms of Liver Cirrhosis • Fatigue and weakness • Loss of appetite • Nausea and vomiting • Weight loss • Jaundice (yellowing of the skin and eyes) • Abdominal pain and swelling • Itchy skin • Dark urine and pale stools
Diagnosis of Liver Cirrhosis • Blood tests to check liver function • Imaging tests, such as ultrasound or CT scan • Liver biopsy to confirm diagnosis and determine severity of liver damage
Treatment of Liver Cirrhosis • Treating the underlying cause, such as stopping alcohol abuse or treating viral hepatitis • Medications to manage symptoms and complications, such as diuretics to reduce fluid buildup • Liver transplant for severe cases
Complications of Liver Cirrhosis • Portal hypertension, which can lead to varices and bleeding • Ascites, which is fluid buildup in the abdomen • Hepatic encephalopathy, which is a brain disorder caused by liver failure • Liver cancer
Prevention of Liver Cirrhosis • Limit alcohol intake • Practice safe sex and get vaccinated for hepatitis B • Maintain a healthy weight and diet • Avoid exposure to harmful chemicals
Conclusion • Liver cirrhosis is a serious condition that can have severe complications • Early detection and treatment can help manage symptoms and prevent further damage • Prevention is key to reducing the risk of liver cirrhosis
- More by User
Cirrhosis liver
Cirrhosis liver. Dr. Arun R Nair Assistant Professor, dept. of PM. Definition. Cirrhosis, which can be the final stage of any chronic liver disease, is a diffuse process characterized by fibrosis and conversion of normal architecture to structurally abnormal nodules.
1.52k views • 17 slides
Liver Cirrhosis
Liver Cirrhosis. K. Dionne Posey, MD, MPH Internal Medicine & Pediatrics December 9, 2004. Introduction. The two most common causes in the United States are alcoholic liver disease and hepatitis C, which together account for almost one-half of those undergoing transplantation . Introduction.
3.84k views • 60 slides
Liver Cirrhosis. Lamya Alnaim, PharmD. Background. Cirrhosis → the end stage of any chronic liver disease. Hepatitis C and alcohol are the main causes Two major syndromes result Portal hypertension Hepatic insufficiency.
2.44k views • 87 slides
LIVER CIRRHOSIS – AYURVEDIC TREATMENT
LIVER CIRRHOSIS – AYURVEDIC TREATMENT. Dr. Vikram Chauhan is One of the most Promising Ayurvedic doctors in the world and a senior consultant physician from India. He has 12 years of international exposure & treated patients of all ages and all races and
1.09k views • 25 slides
LIVER CIRRHOSIS – AYURVEDIC TREATMENT . Dr. Vikram Chauhan is One of the most Promising Ayurvedic doctors in the world and a senior consultant physician from India. He has 12 years of international exposure & treated patients of all ages and all races and
1.32k views • 25 slides
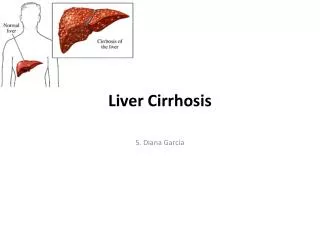
Liver Cirrhosis . S. Diana Garcia . What is Liver Cirrhosis?. Cirrhosis (pronounced sih-ROW-sis) is a consequence of chronic liver disease characterized by replacement of liver tissue by fibrosis, scar tissue, and regenerative nodules leading to loss of liver function. .
1.37k views • 11 slides
Liver Cirrhosis. S. Diana Garcia. What is Liver Cirrhosis?. Cirrhosis (pronounced sih-ROW-sis) is a consequence of chronic liver disease characterized by replacement of liver tissue by fibrosis, scar tissue, and regenerative nodules leading to loss of liver function.
924 views • 11 slides
LIVER CIRRHOSIS
LIVER CIRRHOSIS. DEFINITION : pathological condition with the development of fibrosis to the point that there is architectural distorsion with formation of regenerative nodules. CAUSES : Alcoholism Chronic viral hepatitis (Hepatitis B, Hepatitis C) Autoimmune hepatitis
1.34k views • 27 slides
Liver Cirrhosis and Its Treatment
Cirrhosis is scarring of the liver that occurs as a result of chronic liver disease. Scarring causes disruptions to the flow of blood and bile through the liver and keeps the liver from working properly.
649 views • 4 slides
Liver Disease: Symptoms, causes, treatment, prevention and more
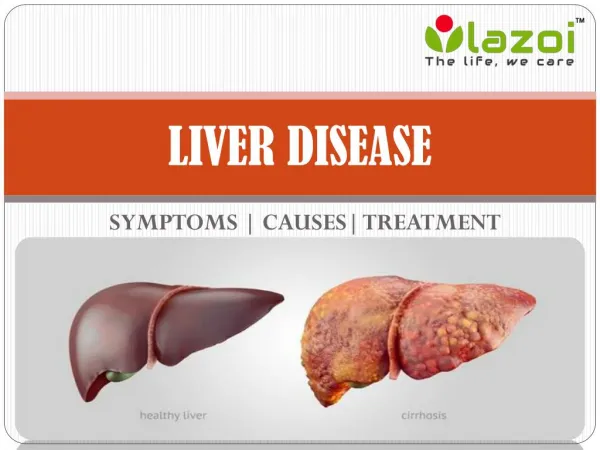
The liver is the largest internal organ in the body located under your rib cage on the right side of your abdomen. It is necessary for digesting food, absorbing nutrients, and eliminating toxic substances. Other than these, liver is vital for storing nutrients and producing proteins.
705 views • 8 slides
Cirrhosis of Liver: Causes and Symptoms
Highest Success Rate of Liver Transplants in India! With 17 years of experience, Dr. Vivek Vij has a track record of 95% patients and 100% donor success rate.
81 views • 1 slides
Symptoms of Male Menopause- Causes and Treatment Options
Women aren’t the only ones that can experience menopause symptoms. Men can suffer from age-related hormonal upheaval as well. Symptoms and treatment options for male menopause are the subject of this article.
108 views • 8 slides
Tinnitus – Symptoms, Causes and Treatment Options
The sensation of noise or resonant in the ears is known as Tinnitus.At the Audiology clinic all the treatments are performed by the Doctor of Audiology, Dr. Deepak Kumar. Firstly, we take a complete diagnostic audiology test of the patients and on the basis of their report, suitable hearing aids recommend to the patients.
56 views • 3 slides
Acid Reflux - Symptoms, Causes and Treatment Options
1.tAcid Reflux - Symptoms, Causes and Treatment Options 2.tAcid Reflux - Acid reflux is a fairly common disease, and more than 10 million cases are reported each year in India. It is technically known as GERD or u2018gastroesophageal reflux diseaseu2019. Acid reflux results in the backing up of stomach acids and bile into the food pipe in a reverse upward direction. An abnormal functioning of the LES (lower oesophageal sphincter), which connects the food pipe with the stomach results in acid reflux disease. It causes a burning pain in the chest, and irritation in the lining of the oesophagus (food pipe). 3.tAs it is a common disease, diagnosing acidic refluxes do not require a medical professional at all times. One can discern the presence of refluxes, based on symptoms experienced by oneself. Also laboratory testing is generally not required to diagnose acid refluxes. Let us study the symptoms, causes and various options for treatment of acid reflux in detail. 10.tIf you are struggling with Acid Reflux or GERD, take an appointment with GERD Specialist - Dr. Chirag Thakkar at Adroit Centre for Digestive and Obesity Surgery. 11.t Consult us for GERD Treatment - For Appointment Call - 079-29703438 Or Visit:- www.drchiragthakkar.com
125 views • 11 slides
Liver Transplant Symptoms and Causes
A liver transplant is a process by which failing liver is surgically replaced with the normal and healthy liver. For liver failures, only cure is to go for liver transplant. When an originally healthy live suffers major injury, acute liver failure occurs.
38 views • 2 slides
Tonsillitis – Symptoms, Causes & Treatment Options
Tonsils are the two lymph nodes located on each side of the back of your throat. They function as a defense mechanism and help prevent your body from getting an infection. When tonsils become infected, the condition is called tonsillitis. View this presentation to know more.
130 views • 6 slides
Liver Cirrhosis - Symptoms, Prevention, Diagnosis Tests
Liver Cirrhosis is the last stage of scarring (Fibrosis) of the liver that involves loss of liver cells. The main cause of cirrhosis are alcohol, hepatitis, and other liver diseases. Know about the symptoms, causes, prevention and diagnosis tests for liver cirrhosis.
144 views • 10 slides
1.19k views • 87 slides
Liver CIRRHOSIS
Liver CIRRHOSIS. Doç.Dr .Atakan Yeşil Yeditepe Unıversıty Department of Gastroenterology. Consequence of chronic liver disease characterized by replacement of liver tissue by fibrosis, scar tissue and regenerative nodules leading to progressive loss of liver function.
1.09k views • 73 slides
Liver Cirrhosis. K. Dionne Posey, MD, MPH Internal Medicine & Pediatrics December 9, 2004. Introduction. The two most common causes in the United States are alcoholic liver disease and hepatitis C, which together account for almost one-half of those undergoing transplantation. Introduction.
875 views • 60 slides
Neurological Problems: Causes, Symptoms & Treatment Options
The symptoms may seem like that of the other health conditions, so it is essential to consult the best neurologist in Dubai and get a diagnosis before the condition gets worse. Coming to the available treatment options, the most popular treatments among the masses. Read more info: https://bit.ly/2FJf68g
89 views • 8 slides


Adolescent Idiopathic Scoliosis Causes Symptoms and Treatment Options
Adolescent Idiopathic Scoliosis is the most common type of Scoliosis suffered by children between the ages of 10 and 18. As the onset of the curve coincides with the growth spurt of the children, the possibility of curve progression increases, severely impacting the body anatomy over time.
120 views • 9 slides
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Hepatic cirrhosis.
Bashar Sharma ; Savio John .
Affiliations
Last Update: October 31, 2022 .
- Continuing Education Activity
Cirrhosis is characterized by fibrosis and nodule formation of the liver secondary to chronic injury, leading to alteration of the normal lobular organization of the liver. Various insults can injure the liver, including viral infections, toxins, hereditary conditions, or autoimmune processes. With each injury, the liver initially forms scar tissue (fibrosis) without losing its function. After a chronic injury, most of the liver tissue becomes fibrotic, leading to loss of function and the development of cirrhosis. This activity reviews the causes, evaluation, and management of hepatic cirrhosis and highlights the interprofessional team's role in managing patients with this condition.
- Identify the pathophysiology of cirrhosis.
- Assess the etiology of cirrhosis.
- Evaluate the presentation of a patient with cirrhosis.
- Communicate the importance of improving care coordination amongst interprofessional team members to improve outcomes for cirrhotic patients.
- Introduction
Cirrhosis is characterized by fibrosis and nodule formation of the liver, secondary to a chronic injury, which leads to alteration of the normal lobular organization of the liver. Various insults can injure the liver, including viral infections, toxins, hereditary conditions, or autoimmune processes. The liver initially forms scar tissue (fibrosis) with each injury without losing its function. After a long-standing injury, most of the liver tissue gets fibrosed, leading to loss of function and the development of cirrhosis. See image. Cirrhosis, Liver.
Chronic liver diseases usually progress to cirrhosis. In the developed world, the most common causes of cirrhosis are hepatitis C virus (HCV), alcoholic liver disease, and nonalcoholic steatohepatitis (NASH). In contrast, hepatitis B virus (HBV) and HCV are the most common causes in the developing world. [1] Other causes of cirrhosis include autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis, hemochromatosis, Wilson disease, alpha-1 antitrypsin deficiency, Budd-Chiari syndrome, drug-induced liver cirrhosis, and chronic right-sided heart failure. Cryptogenic cirrhosis is defined as cirrhosis of unclear etiology.
- Epidemiology
The worldwide prevalence of cirrhosis is unknown; however, it has been estimated to be between 0.15% and 0.27% in the United States. [2] [3]
- Pathophysiology
Multiple cells play a role in liver cirrhosis, including hepatocytes and sinusoidal lining cells such as hepatic stellate cells (HSCs), sinusoidal endothelial cells (SECs), and Kupffer cells (KCs). HSCs form a part of the wall of the liver sinusoids, and their function is to store vitamin A. When these cells are exposed to inflammatory cytokines, they get activated, transform into myofibroblasts, and start depositing collagen, which results in fibrosis. SECs form the endothelial lining and are characterized by the fenestrations they make in the wall that allow the exchange of fluid and nutrients between the sinusoids and the hepatocytes. [4] Defenestration of the sinusoidal wall can happen secondary to chronic alcohol use and promote perisinusoidal fibrosis. [5] KCs are satellite macrophages that line the wall of the sinusoids as well. Studies from animal models have shown that they play a role in liver fibrosis by releasing harmful mediators when exposed to injurious agents and acting as antigen-presenting cells for viruses. [6] Hepatocytes are also involved in cirrhosis's pathogenesis, as damaged hepatocytes release reactive oxygen species and inflammatory mediators that can promote activating HSCs and liver fibrosis. [7]
The major cause of morbidity and mortality in cirrhotic patients is the development of portal hypertension and hyperdynamic circulation. Portal hypertension develops secondary to fibrosis and vasoregulatory changes intrahepatically and systematically, leading to collateral circulation formation and hyperdynamic circulation. [8] Intrahepatically, SECs synthesize nitric oxide (NO) and endothelin-1 (ET-1), which act on HSCs, causing relaxation or contraction of the sinusoids, respectively, and controlling sinusoidal blood flow. In patients with cirrhosis, there is an increase in ET-1 production and the sensitivity of its receptors with a decrease in NO production. This leads to increased intrahepatic vasoconstriction and resistance, initiating portal hypertension. Vascular remodeling mediated by the contractile effects of HSCs in the sinusoids augments the increase in vascular resistance. To compensate for this increase in intrahepatic pressure, collateral circulation is formed. [8] In systemic and splanchnic circulation, the opposite effect happens, with an increase in NO production, leading to systemic and splanchnic vasodilation and decreased systemic vascular resistance. This activates the renin-angiotensin-aldosterone system, leading to sodium and water retention and hyperdynamic circulation. Thus, in cirrhosis with portal hypertension, there is a depletion of vasodilators (predominantly NO) intrahepatic-ally but a renin-excess of NO extrahepatically in the splanchnic and systemic circulation, leading to sinusoidal vasoconstriction and splanchnic (systemic) vasodilation. The collaterals also contribute to the hyperdynamic circulation by increasing the venous return to the heart. [8] [9]
- Histopathology
Cirrhosis is classified based on morphology or etiology.
- Viral - hepatitis B, C, and D
- Toxins - alcohol, drugs
- Autoimmune - autoimmune hepatitis
- Cholestatic - primary biliary cholangitis, primary sclerosing cholangitis
- Vascular - Budd-Chiari syndrome, sinusoidal obstruction syndrome, cardiac cirrhosis
- History and Physical
Patients with cirrhosis can be asymptomatic or symptomatic, depending on whether their cirrhosis is clinically compensated or decompensated. In compensated cirrhosis, patients are usually asymptomatic, and their disease is detected incidentally by labs, physical exams, or imaging. One of the common findings is mild to moderate elevation in aminotransferases or gamma-glutamyl transpeptidase with possible enlarged liver or spleen on the exam. On the other hand, patients with decompensated cirrhosis usually present with a wide range of signs and symptoms arising from a combination of liver dysfunction and portal hypertension. The diagnosis of ascites, jaundice, hepatic encephalopathy, variceal bleeding, or hepatocellular carcinoma in a patient with cirrhosis signifies the transition from a compensated to a decompensated phase of cirrhosis. Other cirrhosis complications include spontaneous bacterial peritonitis and hepatorenal syndrome, which occur in patients who have ascites.
Multiple Organs Affected
Gastrointestinal
Portal hypertension can cause ascites, hepatosplenomegaly, and prominence of the periumbilical abdominal veins, resulting in caput medusa. Esophageal varices are another complication of cirrhosis secondary to increased blood flow in the collateral circulation, with a mortality rate of at least 20% at 6 weeks after a bleeding episode. [10] Patients with alcoholic cirrhosis are at increased risk of small bowel bacterial overgrowth and chronic pancreatitis, and patients with chronic liver disease have a higher rate of gallstone formation. [11] [12]
Hematologic
Anemia can occur due to folate deficiency, hemolytic anemia (spur cell anemia in severe alcoholic liver disease), and hypersplenism. There can be pancytopenia due to hypersplenism in portal hypertension, impaired coagulation, disseminated intravascular coagulation, and hemosiderosis in cirrhosis patients due to different causes.
Patients with cirrhosis are prone to develop hepatorenal syndrome secondary to systemic hypotension and renal vasoconstriction, causing the underfilling phenomenon. Splanchnic vasodilation in cirrhosis leads to decreased effective blood flow to the kidneys, activating the renin-angiotensin-aldosterone system, leading to sodium and water retention and renal vascular constriction. [13] However, this effect is not enough to overcome the systemic vasodilation caused by cirrhosis, leading to renal hypoperfusion and worsened by renal vasoconstriction with the endpoint of renal failure. [14]
Manifestations of cirrhosis include hepatopulmonary syndrome, portopulmonary hypertension, hepatic hydrothorax, decreased oxygen saturation, ventilation-perfusion mismatch, reduced pulmonary diffusion capacity, and hyperventilation.
Spider nevi, central arterioles surrounded by multiple smaller vessels resembling a spider, are seen in cirrhosis patients secondary to hyperestrogenemia. Liver dysfunction leads to a sex hormone imbalance, causing an increased estrogen-to-free testosterone ratio and the formation of spider nevi. [15] Palmar erythema is another skin finding that is seen in cirrhosis and is also secondary to hyperestrogenemia. Jaundice is a yellowish discoloration of the skin and mucous membranes seen when the serum bilirubin is greater than 3 mg/dL and in decompensated cirrhosis.
Patients with alcoholic liver cirrhosis can develop hypogonadism and gynecomastia. The pathophysiology is multifactorial, mainly due to the hypersensitivity of estrogen and androgen receptors seen in cirrhotic patients. Hypothalamic pituitary dysfunction has also been implicated in the development of these conditions. [16] Hypogonadism can lead to decreased libido and impotence in males with loss of secondary sexual characteristics and feminization. Women can develop amenorrhea and irregular menstrual bleeding, as well as infertility.
Nail Changes
Clubbing, hypertrophic osteoarthropathy, and the Dupuytren contracture are seen. Other nail changes include azure lunules (Wilson disease), Terry nails, and Muehrcke nails.
Fetor hepaticus (sweet, musty breath smell due to high levels of dimethyl sulfide and ketones in the blood) and asterixis (flapping tremor when the arms are extended and the hands are dorsiflexed) are both features of hepatic encephalopathy that can be seen in cirrhosis. [17] Cirrhosis can lead to hyperdynamic circulation, reduced lean muscle mass, muscle cramps, and umbilical herniation. Physical examination in patients with cirrhosis may reveal stigmata of chronic liver disease (spider telangiectasias, palmar erythema, Dupuytren contractures, gynecomastia, testicular atrophy), signs of portal hypertension (ascites, splenomegaly, caput medusae, Cruveilhier-Baumgarten murmur- epigastric venous hum), signs of hepatic encephalopathy (confusion, asterixis, and fetor hepaticus), and other features such as jaundice, bilateral parotid enlargement, and scant chest/axillary hair.
Lab Findings
Aminotransferases are usually mildly to moderately elevated, with aspartate aminotransferase (AST) greater than alanine aminotransferase (ALT); however, normal levels do not exclude cirrhosis. [18] In most forms of chronic hepatitis (except alcoholic hepatitis), the AST/ALT ratio is less than 1. As chronic hepatitis progresses to cirrhosis, there is a reversal of this AST/ALT ratio. Alkaline phosphatase (ALP), 5'- nucleotidase, and gamma-glutamyl transferase (GGT) are elevated in cholestatic disorders. Prothrombin time (PT) is elevated due to coagulation factor defects and bilirubin, while albumin is low as the liver synthesizes it, and its functional capacity decreases. Thus, serum albumin and PT are true indicators of synthetic hepatic function. Normochromic anemia is seen; however, macrocytic anemia can be seen in alcoholic liver cirrhosis. Leukopenia and thrombocytopenia are also seen secondary to sequestration by the enlarged spleen and alcohol suppression effect on the bone marrow. [19] Immunoglobulins, especially the gamma fraction, are usually elevated due to impaired clearance by the liver. [20]
Specific Labs to Investigate Newly Diagnosed Cirrhosis
Serology and PCR techniques for viral hepatitis and autoimmune antibodies (anti-nuclear antibodies [ANA], anti-smooth muscle antibodies (ASMA), anti-liver-kidney microsomal antibodies type 1 (ALKM-1) and serum IgG immunoglobulins) for autoimmune hepatitis and anti-mitochondrial antibody for primary biliary cholangitis may be ordered. Ferritin and transferrin saturation for hemochromatosis, ceruloplasmin, and urinary copper for Wilson disease, Alpha 1-antitrypsin level, and protease inhibitor phenotype for alpha 1-antitrypsin deficiency, and serum alpha-fetoprotein for hepatocellular carcinoma (HCC) are other useful tests.
Imaging and Liver Biopsy
Several imaging modalities are used alongside labs to help diagnose cirrhosis. These include ultrasound, CT, MRI, and transient elastography (fibroscan). Ultrasonography is a cheap, noninvasive, and available modality for evaluating cirrhosis. It can detect nodularity and increased echogenicity of the liver, which are seen in cirrhosis; however, it is nonspecific as these findings can also be seen in fatty liver. [21] It can also determine the ratio of the caudate lobe width to the right lobe width, which usually increases in cirrhosis. [22] Moreover, it is a useful screening tool for HCC in cirrhotic patients. Duplex Doppler ultrasonography helps to assess the patency of hepatic, portal, and mesenteric veins. CT and MRI, in contrast, can detect HCC and vascular lesions, with MRI being superior to CT. [23] MRI can also be used to detect the level of iron and fat deposition in the liver for hemochromatosis, steatosis, and biliary obstruction if an MRC (magnetic resonance cholangiography) is obtained.[24] [25] MRI, however, is expensive and not readily available. Transient elastography (fibroscan) is a noninvasive method that uses high-velocity ultrasound waves to measure liver stiffness, which correlates with fibrosis. In cirrhosis, a colloid liver spleen scan using technetium-99m sulfur colloid may show increased colloid uptake in the bone marrow and spleen compared to the liver. The presence of varices in the esophagus or stomach on esophagogastroduodenoscopy (EGD) suggests portal hypertension. A liver biopsy is the gold standard for diagnosing cirrhosis and assessing the disease's degree of inflammation (grade) and fibrosis (stage). See Image . Cirrhosis, Portal Space in Fibrous Septa. Reticulin stain 4×.
Nevertheless, it can miss the diagnosis at times due to sampling errors. [24] The diagnosis of cirrhosis by biopsy requires the presence of fibrosis and nodules. The nodular pattern can be micronodular, macronodular, or mixed with the micronodular pattern, representing an independent risk factor for elevated hepatic venous pressure gradient (HVPG) and more severe disease. [24] Noninvasive tests using direct and indirect serum markers detect patients with significant fibrosis/cirrhosis from patients with no/mild fibrosis. [25] [26] [27]
- Treatment / Management
Damage to the liver is permanent. Nevertheless, further injury to the liver should be avoided to halt the progression of the disease. General management to prevent chronic liver disease includes avoidance of alcohol, vaccination for HBV and HCV, good nutrition with a balanced diet, weight reduction, and early treatment of precipitating factors like dehydration, hypotension, and infections (see Image. Schistosomiasis Infection). This is achieved by routine monitoring of volume status, kidney function, varices development, and progression to HCC. Specific therapy usually targets the etiology, including antiviral medications in viral hepatitis, steroids and immunosuppressant agents in autoimmune hepatitis, ursodeoxycholic acid and obeticholic acid in primary biliary cholangitis, copper chelation in Wilson disease, and iron chelation and phlebotomy in hemochromatosis. Weight loss of at least 7% is beneficial in NASH, and alcohol abstinence is crucial in alcoholic cirrhosis. [28]
- Differential Diagnosis
The differential diagnosis for hepatic cirrhosis includes the following:
- Acute fatty liver of pregnancy
- Amanita phalloides mushroom poisoning
- Acetaminophen poisoning
- Bacillus cereus toxin
- Fructose intolerance
- Galactosemia
- HELLP(hemolysis, elevated liver enzymes, low platelets) syndrome of pregnancy
- Hemorrhage viruses (Ebola virus, Lassa virus, Marburg virus)
- Idiopathic drug reaction
- Neonatal iron storage diseases
- Tyrosinemia
Predictive models for the prognosis of cirrhosis estimate the 10-year survival in patients with compensated cirrhosis at 47%, but this drops to 16% once a decompensating event occurs. The Child-Turcotte-Pugh (CTP) scoring or classification uses serum albumin, bilirubin, PT, ascites, and hepatic encephalopathy to classify patients with cirrhosis into classes A, B, and C. 1 and 2-year survival rates for these classes are 100% and 85% (A), 80% and 60% (B), and 45% and 35% (C). The model for end-stage liver disease (MELD) score is another model used to predict the short-term mortality of patients with cirrhosis. It uses serum bilirubin, creatinine, and INR to predict mortality within the next 3 months. [29] Based on the MELD score (more recently, the MELDNa score), the priority of organ allocation for liver transplantation for patients with cirrhosis is adjudicated in the US. [29] Liver transplantation is indicated in decompensated cirrhosis that does not respond to medical treatment. The 1-year and 5-year survival rates after liver transplantation are approximately 85% and 72%, respectively. Recurrence of the underlying liver disease can occur after a transplant. [30] Long-term side effects of immunosuppressant drugs are another cause of morbidity in transplant patients.
- Complications
Complications accompanying hepatic cirrhosis can include:
- Portal hypertension
- Edema in the abdomen and lower extremities
- Splenomegaly
- Hepatic encephalopathy [31]
- Deterrence and Patient Education
While patient lifestyle changes cannot cure cirrhosis, these behavioral modifications can prevent or at least delay disease progression and provide symptomatic relief. Modifiable lifestyle factors include:
- Eliminating ethanol consumption
- Avoid raw seafood and shellfish
- possible low-sodium diet to reduce water retention
- Vaccinations for pneumonia, influenza, and hepatitis
- Regulate protein intake according to their doctor's directions
- Some doctors will recommend a vitamin and mineral supplement
- Pearls and Other Issues
Hepatocellular Carcinoma
HCC is the most common primary cancer in the liver, and its incidence is increasing. [32] Cirrhosis secondary to HBV and HCV is the most common risk factor. [32] Routine monitoring of cirrhotic patients for the development of HCC is recommended, with at least 6 monthly screenings using abdominal ultrasonography. [2]
- Enhancing Healthcare Team Outcomes
An interprofessional team that includes a hepatologist, gastroenterologist, liver surgeon, pathologist, infectious disease specialist, primary care provider, and internist is best for treating and preventing liver cirrhosis. All healthcare workers should follow patients with liver dysfunction from any cause because it can quickly become irreversible. Liver cirrhosis is associated with many systemic complications that can cause death. A liver transplant is not always an option because of the shortage of donors.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Schistosomiasis Infection. Under a magnification of 500X, this photomicrograph of a liver tissue specimen revealed signs of a schistosomiasis infection. This included a histopathologic finding known as pipe stem cirrhosis, which occurs when schistosomes (more...)
Cirrhosis, Liver. Reticulin stain enhances the fibrous septa dividing the hepatic nodules, ×4 magnification. Contributed by F Farci, MD
Liver Cirrhosis, Reticulin Stain 4× Contributed by F Farci, MD
Cirrhosis, Portal Space in Fibrous Septa. Reticulin stain 4×. Contributed by F Farci, MD
Liver Cirrhosis, Trichrome Stain, 4× Contributed by F Farci, MD
Disclosure: Bashar Sharma declares no relevant financial relationships with ineligible companies.
Disclosure: Savio John declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Sharma B, John S. Hepatic Cirrhosis. [Updated 2022 Oct 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Metabolism of N-nitrosodimethylamine, methylation of macromolecules, and development of hepatic fibrosis in rodent models. [J Mol Med (Berl). 2020] Review Metabolism of N-nitrosodimethylamine, methylation of macromolecules, and development of hepatic fibrosis in rodent models. George J, Tsuchishima M, Tsutsumi M. J Mol Med (Berl). 2020 Sep; 98(9):1203-1213. Epub 2020 Jul 14.
- Non-hepatic insults are common acute precipitants in patients with acute on chronic liver failure (ACLF). [Dig Dis Sci. 2010] Non-hepatic insults are common acute precipitants in patients with acute on chronic liver failure (ACLF). Duseja A, Chawla YK, Dhiman RK, Kumar A, Choudhary N, Taneja S. Dig Dis Sci. 2010 Nov; 55(11):3188-92. Epub 2010 Aug 19.
- Review Cirrhosis and autoimmune liver disease: Current understanding. [World J Hepatol. 2016] Review Cirrhosis and autoimmune liver disease: Current understanding. Liberal R, Grant CR. World J Hepatol. 2016 Oct 8; 8(28):1157-1168.
- Overlap syndrome of autoimmune hepatitis and primary biliary cholangitis complicated with atypical hepatocellular carcinoma: a case report. [J Med Case Rep. 2023] Overlap syndrome of autoimmune hepatitis and primary biliary cholangitis complicated with atypical hepatocellular carcinoma: a case report. Surdea-Blaga T, Cărăguț RL, Caraiani C, Spârchez Z, Al Hajjar N, Dumitrașcu DL. J Med Case Rep. 2023 Jul 25; 17(1):328. Epub 2023 Jul 25.
- Review Molecular mechanisms in the pathogenesis of N-nitrosodimethylamine induced hepatic fibrosis. [Cell Death Dis. 2019] Review Molecular mechanisms in the pathogenesis of N-nitrosodimethylamine induced hepatic fibrosis. George J, Tsuchishima M, Tsutsumi M. Cell Death Dis. 2019 Jan 8; 10(1):18. Epub 2019 Jan 8.
Recent Activity
- Hepatic Cirrhosis - StatPearls Hepatic Cirrhosis - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

- Nutrition counsellor
- Food Allergy
- gastroenterology
- Heptologist In Delhi
- Liver transplant
- Alcoholic Liver Cirrhosis
Alcoholic liver cirrhosis is a late stage of fibrosis of the liver caused by many forms of liver diseases and conditions, such as chronic alcoholism. A person diagnosed with an alcoholic liver case may start from having fatty liver disease, then alcoholic hepatitis, and ultimately develop alcoholic cirrhosis. Hence, alcoholic liver cirrhosis stages in three levels. The diagnosed liver cirrhosis can be of two types :
- Compensated cirrhosis – when symptoms are not noticeable
- Uncompensated cirrhosis- when the symptoms can be noticed
The most common alcoholic liver causes are:
- Chronic alcohol consumption
- Chronic hepatitis
- Fatty liver disease
- Iron buildup in the body or hemochromatosis
- Copper accumulated in the liver (Wilson’s disease)
- Cystic fibrosis
- Biliary Atresia
- Inherited sugar metabolism or digestive disorders
- Infection like syphilis
Many other factors like the destruction of bile ducts(Primary Biliary Cirrhosis) or leaky gut also called, increased intestinal permeability are cofactors for the development of alcoholic liver cirrhosis.
Now, let us have a look at alcoholic liver cirrhosis symptoms:
- Food pipe problems
- Portal hypertension
- Swelling in legs (oedema) and abdomen (ascites)
- Bleeding in mouth
- Confusion, poor memory, loss of appetite
- Patchy red skin on palms (erythema)
Food pipe problem is also known as esophageal varices. Kidney failure and hypersplenism are other complications that happen due to this medical condition. If the symptoms are not taken seriously, then this deficient liver may arise a life-threatening situation. Hence, a person needs to keep a track of these indicators as if these signs are caught early and treated, it may slow down the progression of the disease.
How to treat alcoholic liver cirrhosis:
The first and foremost step in treatments is to help the patient to cease alcohol consumption. Medications like corticosteroids, calcium channel blockers, insulin can also be prescribed by the doctor as per the alcoholic liver care plan. Hepatologists may advise the patient to follow an alcoholic liver disease diet inclusive of fiber and protein. If the condition of the patient gets worsened, then the hepatologist may have to suggest a liver transplant surgery.
Dr. Nivedita Pandey is one of the best liver specialist doctors in Patna, Bihar. She is a well-renowned liver specialist doctor in Delhi, the best stomach doctor in Patna, the best gastroenterologist in Jammu, and a notable stomach doctor in Faridabad. Now, you can sway off all your gastroenterological worries online by booking an online gastroenterologist consultation with one of the best hepatologists in India. She is a liver specialist in Delhi NCR, one of the finest gastroenterologists in Jhansi and Jammu, and an acidity specialist doctor in Patna. Dr. Pandey’s gastroenterologist live chat has also helped people in several ways.
Case Review
This alcoholic liver case study presents a patient with liver cirrhosis. A 43-year-old man was brought into the hospital with a complaints of loss of appetite, abdominal distention, and arrhythmia. He also experienced itchy skin and blood in the stool. The patient’s family rushed him into the hospital, and he was in a half-conscious state. The patient was taken to the emergency room for evaluation. As told by the family, he had a past medical history and was a heavy alcohol consumer. This alcoholic liver case history consisted of various medical ailments like fatty liver, asthma, tuberculosis, malnutrition, hypertension, and hepatitis C. The patient had a heart attack three years back and stented for the same. Due to his health conditions, he was on several medications. In the emergency room, when the patient was under observation by a stomach specialist doctor in Patna and her team, they were able to diagnose from his symptoms that it was alcoholic liver cirrhosis. The patient went for a few scans including, a liver function test, liver ultrasound, and endoscopy along with CT, blood test, and urine tests.
Case Discussion
Though most of the liver cirrhosis causes remain unknown, with the help of her team, the best liver doctor and specialist in Patna was able to find out the reason for this one. The liver cirrhosis caused in this case was due to the medical history of the patient. His scans came out to be reasonably sound, and a liver biopsy was conducted to confirm the severity and type of liver disease. There were problems in his blood and urine culture, and they were taken care of by the team. His liver appeared swollen in the reports. There were certain other problems seen in his ultrasound and endoscopy. The crew decided to start with the treatment while keeping him under observation for the next 72 hours.
Clinical Symptoms
He was initially confused and was not able to respond or hear properly. According to the condition reported by his family i.e.- appetite loss, memory loss, and confusion were some other clinical symptoms of alcoholic liver cirrhosis. When the doctor talked to the family of the patient, she was able to get a clearer picture. The patient complained about acute abdominal pain. When Dr. Pandey, one of the best doctors in Patna for the stomach, observed the patient and talked to him, she noticed bleeding in his mouth. This further helped doctors to eliminate all doubts, and after looking at the lab results, they made out it was alcoholic liver cirrhosis.
The first and foremost management required when treating the alcoholic liver cirrhosis case is calming the patient down. The liver specialist with the help of her fellow doctors was able to counsel the patient and explain his medical condition to the family. After a complete diagnosis, the patient was taken to the ICU as he was under observation. The doctor prescribed him antioxidant drugs and insulin to control any future problems while treating the present one. The doctor is the best gastroenterologist in Faridabad, Delhi, and Patna, and she handled the situation well before any further complications. The patient got his discharge in due time and was sent back home in a healthy and sound condition.
1. Which Group of People are More Likely to get diagnosed with alcoholic liver cirrhosis?
A person who has drunk heavily for a long time is more prone to acquire this disease. Women are also at risk for this medical disease due to the absence of many enzymes which break down alcohol particles.
Consider consulting the best gastroenterologist in India , Dr. Nivedita Pandey who is also well known for her nutritional counselling services and teleconsultation services. She is also famous for her care from afar service. You can also find her as the best liver specialist doctor in Patna, Bihar or hepatologist in Patna or the best doctor for hepatitis b in Patna , a gastroenterologist in Faridabad , the best gastro doctor in Delhi, NCR , a gastroenterologist In Uttarakhand , a liver specialist in Jhansi , best gastroenterologist in Jammu take advantage of the online gastroenterology consultation to gastroenterologist live chat and receive the best treatment that your body deserves!
2. Is liver cirrhosis cancer?
No, liver cirrhosis is not a type of cancer. If a person has alcoholic liver cirrhosis, he/she has an increased risk of liver cancer.
3. Is liver cirrhosis a hereditary disease?
Negative, alcoholic liver cirrhosis is not a hereditary disease, rather it is a type of an acquired disease.
Privacy Preference Center
Privacy preferences.
- Case Report
- Open access
- Published: 09 September 2024
Robot-assisted laparoscopic hepatectomy for hepatocellular carcinoma with Fontan-associated liver disease: a world-first case report
- Takuma Ishikawa 1 ,
- Shinji Itoh ORCID: orcid.org/0000-0003-0382-2520 1 ,
- Takeo Toshima 1 ,
- Shohei Yoshiya 1 ,
- Yuki Bekki 1 ,
- Norifumi Iseda 1 ,
- Yuriko Tsutsui 1 ,
- Ichiro Sakamoto 2 ,
- Kotaro Abe 2 &
- Tomoharu Yoshizumi 1
Surgical Case Reports volume 10 , Article number: 210 ( 2024 ) Cite this article
Metrics details
Fontan-associated liver disease (FALD) encompasses hepatic complications following the Fontan procedure, ranging from fibrosis to hepatocellular carcinoma (HCC). Despite advancements in surgical techniques and perioperative care, robot-assisted laparoscopic hepatectomy (RALH) for HCC in patients with FALD has not been previously reported owing to concerns about the Fontan circulation.
Case presentation
We present the first case of RALH for recurrent HCC in a 45-year-old man after the Fontan procedure. The preoperative evaluation confirmed good cardiac function. The procedure involved meticulous monitoring and management of central venous pressure and was successfully completed with minimal blood loss. Postoperative recovery was uneventful. With thorough preoperative cardiac assessment and close collaboration between cardiologists and anesthesiologists, RALH can be safely performed in selected patients with FALD.
Conclusions
Even if a patient has a history of FALD, RALH can be safely performed in selected patients under appropriate conditions.
Liver complications after undergoing the Fontan procedure (FP) are classified as Fontan-associated liver disease (FALD) [ 1 ]. The first report of FALD was by Stanton et al. in 1981 when cirrhosis was found in an autopsy case who died of a fatal arrhythmia 21 months after the FP [ 2 ]. FALD is a severe complication, particularly in adult patients who have undergone the FP [ 3 ]. FALD encompasses a range of hepatic abnormalities, from mild fibrosis to cirrhosis and hepatocellular carcinoma (HCC), and is associated with benign and malignant liver lesions [ 4 ]. The pathophysiology of FALD is complex, involving hemodynamic and inflammatory factors [ 3 ]. Recently, the long-term prognosis after the FP has been improving owing to advances in procedures and postoperative management [ 5 ]. As a result, the number of patients diagnosed with FALD, a late complication of liver fibrosis and cirrhosis leading to HCC, is increasing.
Robot-assisted surgery is rapidly gaining popularity in many surgical fields, because it is precise, minimally invasive surgery with enhanced stereoscopic magnification enabling full dexterity [ 6 ]. The first report of robot-assisted laparoscopic hepatectomy (RALH) in the world was made by Giulianotti in 2003 [ 7 ]. Several limitations and drawbacks to conventional laparoscopy exist, including limited movement, the inability to perform high-precision sutures, unnatural positions for the surgeon, and flat vision. Robotic surgery can overcome the limitations of conventional laparoscopy. The goal is for this type of minimally invasive surgery to be available to more patients [ 7 ].
Despite the known benefits of RALH, its results have never been reported after the FP. The limitations of RALH in FALD are related primarily to the adverse effects of pneumoperitoneum on the Fontan circulation due to increasing intra-abdominal and intrathoracic pressure, rising pulmonary and systemic resistance, and cardiac preload and output reduction, which can be fatal [ 8 ]. Moreover, severe portal hypertension may cause a high risk of bleeding during liver resection [ 9 ]. To the best of our knowledge, this report is the first case of RALH for HCC after the FP.
We present the case of a 45-year-old man with HCC recurrence. The patient had a history of tricuspid atresia and underwent a Blalock–Taussig–Thomas shunt procedure at the age of 3, an FP at the age of 6, and total cavopulmonary bypass conversion, atrial septal defect creation, right atrium maze procedure, and implantation of a permanent pacemaker lead at the age of 26. At age 42, the patient had elevated alpha-fetoprotein levels, and a detailed examination revealed HCC. Lap-assisted partial resection of segment 3 of the liver was performed. Pathological findings indicated a moderate to poorly differentiated HCC with trabecular and pseudoglandular patterns of 2.5 × 1.9 cm. This was classified as vp1, vv1, va0, b0, im0, and the peritumoral liver tissue showed stage F3 cirrhosis according to the new Inuyama classification [ 10 ]. No malignant cells were found in the surgical margins (R0 resection).
During follow-up, HCC recurrence was suspected in segment 5 of the liver on computed tomography (CT) 25 months postoperatively. CT hepatic arteriography/CT arterial portography revealed a reticular pattern of decreased enhancement in the hepatic parenchyma, indicative of changes due to congestive liver. An 8 mm arterially enhanced nodule was observed with corona-like enhancement in segment 5 of the liver ( Fig. 1 a ) and a lack of portal blood flow, consistent with findings of HCC ( Fig. 1 b ). The tumor was located on the edge of segment 5, and the nearest branch of the Glisson 5 was not within the planned resection margin ( Fig. 1 c, d ).

Abdominal computed tomography arteriography and arterial portography. a 8 mm arterially enhanced nodule with corona-like enhancement was observed in segment 5 of the liver (yellow arrowhead). b Same nodule exhibited poor portal blood flow (yellow arrowhead). c Position of the tumor is indicated in the 3D images (yellow arrowhead). d 3D images show that the tumor was located on the edge of segment 5 (yellow arrowhead) and branch of the Glisson 5 (orange arrowhead)
Preoperative information included a height of 164 cm and a weight of 57.1 kg (body mass index, 21.1). Blood testing showed the following results: aspartate transaminase, 35 U/L; alanine transaminase, 56 U/L; albumin, 4.2 mg/dL; total bilirubin, 0.9 mg/ dL; prothrombin time-international normalized ratio, 1.08; and platelet count, 12.8 × 104/μL. Alpha-fetoprotein and des-gamma-carboxy prothrombin were elevated to 11.1 ng/mL and 7538 mAU/mL, respectively. Type IV collagen 7S was slightly elevated to 6.0 ng/mL, but other markers of liver fibrosis were normal (hyaluronic acid, 39 ng/mL; mac-2-binding protein glycosylation isomer, 0.34 cutoff index). Negative results were obtained for hepatitis B virus surface antigen and hepatitis C virus antibody, and the patient had no history of heavy alcohol consumption. The indocyanine green (ICG) retention rate at 15 min was 15.9%. The Child–Pugh classification was A. Echocardiography demonstrated good single right ventricular function and no obstruction in the Fontan circulation. Cardiac function tests showed an ejection fraction of 61%, central venous pressure (CVP) of 10–14 mmHg, pulmonary artery pressure of 17 mmHg, and pulmonary capillary wedge pressure of 11 mmHg. Pulmonary and renal functions were normal. Oxygen saturation in room air was 96%. The systolic blood pressure was approximately 90 mmHg.
Robot-assisted laparoscopic partial resection of S5 was planned to address the recurrent HCC after a multidisciplinary discussion with the cardiologist and anesthesiologist. Warfarin 2 mg was discontinued and replaced with heparin. Two days before the surgery, 12.5 mg of ICG was administered intravenously to the patient. After induction of general anesthesia, a central venous catheter was inserted into the right internal jugular vein for intraoperative monitoring of CVP. A transesophageal echocardiogram was also placed. Management was performed by monitoring cardiac output and its variations using a FloTrac sensor ® . The cardiovascular medications used in this case were dobutamine, vasopressin, furosemide, ephedrine, and phenylephrine.
Surgical procedure
The patient was placed in the supine position. A small incision was made in the subumbilical area, and an access port was placed to induce pneumoperitoneum. A pneumoperitoneum was started at a pressure of 8 mmHg while carefully monitoring vital signs. The liver showed a rough surface consistent with cirrhosis, and a small amount of ascites was observed. Adhesions between the abdominal wall and omentum were noted. The lesion in S5 was visibly protruding ( Fig. 2 a ) . The second port was placed 20 cm away from the tumor, and the third port was positioned 7 cm away in the lower right abdomen. An assistant port (12 mm) was placed 7 cm away between the second and third ports. To add additional ports, it was necessary to perform adhesiolysis within the abdominal cavity. Adequate visualization of the tumor had been achieved, and it was deemed feasible to resect the marginal tumor with four ports. We performed intraperitoneal manipulation using four ports and a minimal number of instruments. ( Fig. 2 b ) .

Operative findings. a Surgery was performed by the insertion of four ports: one subumbilical for the camera (8 mm), one working trocar in the right lateral flank (8 mm), one working trocar in the lower right abdomen position (8 mm), and one assistant port between the second and third ports (12 mm). b Lliver showed a rough surface consistent with cirrhosis. The tumor in S5 was visibly protruding (yellow arrowhead). c Tumor in S5 was revealed using indocyanine green fluorescence for confirmation. d Robot-assisted laparoscopic S5 partial hepatectomy resections were performed
The patient cart was rolled in and docked from the right side. The falciform ligament was not divided. Adhesions were dissected to allow for liver resection. Adhesions around the hepatoduodenal ligament were observed. Furthermore, since the lesion was small and located on the surface of segment 5, we refrained from forcibly Pringle maneuver. The resection line was set to ensure adequate margins. Although the gallbladder was located near the tumor, we were able to secure clear resection margins for the tumor, thus preserving the gallbladder. Liver parenchymal transection was performed using the crush-clamp technique with intraoperative ICG fluorescence to confirm the tumor margins (Fig. 2 c). Small, exposed vessels on the transection surface were coagulated and divided as necessary. The specimen was extracted (Fig. 2 d). Intra-abdominal lavage was performed, and hemostasis was confirmed. A 15 Fr drain was placed through the 8 mm port on the right side of the abdomen. The robotic docking was released, and the patient cart was rolled out (console time was 54 min). The specimen was extracted through the umbilical incision. After confirming the tumor was at a sufficient distance from the resection margin, the incision was closed ( Fig. 3 ) . The operation duration was 111 min, with minimal blood loss.

Macroscopic findings of the resected tissue specimen. a Elastic soft nodule was found in liver segment 5. b On the cut surface, there was a yellowish-white tumor measuring 0.8 cm × 0.8 cm
Histological findings
A well to moderately differentiated HCC with compact, trabecular, and pseudoglandular patterns of 0.6 × 0.6 cm was classified as vp1, vv0, va0, b0, im0. The peritumoral liver tissue showed stage F4 cirrhosis according to the new Inuyama classification [ 10 ] No malignant cells were found in the surgical margins (R0 resection).
Postoperative course
Postoperatively, the patient was managed in the intensive care unit. Owing to low blood pressure, norepinephrine was administered. On the first postoperative day, the drain was removed as its condition was unremarkable. Norepinephrine was discontinued, and the patient was transferred to the general ward and began oral intake. On the second postoperative day, heparin therapy was initiated. On the third postoperative day, oral warfarin was resumed. CT on the sixth postoperative day revealed no issues. Heparin therapy was discontinued on the seventh postoperative day. The patient was discharged on the eighth postoperative day. One year after surgery, the patient has not had HCC recurrence.
We presented a case of robotic-assisted laparoscopic liver resection in a patient with FALD where reoperation was necessary due to HCC recurrence. No reports of robotic-assisted laparoscopic liver resection for HCC with FALD exist. Liver dysfunction arising from FALD causes liver fibrosis, cirrhosis, and HCC, even in young patients [ 11 ]FALD is caused by excessive hepatic congestion due to high CVP and results from fibrosis of the sinusoids and portal tracts. The progression of FALD depends on the duration after the FP and hepatic venous pressure [ 12 ]. It has been reported that FALD progresses to cirrhosis 11–15 years after the FP, with cumulative incidence rates of cirrhosis of 56.6% and 97.9% at 20 and 30 year post-FP, respectively [ 13 ]. The annual incidence of HCC in FALD is estimated to be between 1.5% and 5.0% [ 14 ].
Many cases of HCC arising from FALD are treated non-surgically because of poor liver function, making surgical resection unfeasible [ 9 ]]. However, recent advancements in surgical techniques and perioperative management have made safe hepatectomy possible in open and laparoscopic surgery [ 14 , 15 ] Laparoscopic hepatectomy for HCC arising from FALD has often been avoided owing to the difficulty in controlling venous bleeding caused by high CVP and challenges in anesthesia management [ 16 ].
Robot-assisted laparoscopic surgery in patients with Fontan circulation is considered disadvantageous, because the venous return may be compromised by insufflation of carbon dioxide (CO₂) into the abdomen, use of the reverse Trendelenburg position, and positive pressure ventilation [ 14 , 15 , 17 ]. Furthermore, CO₂ absorption from the peritoneum increases the partial pressure of CO₂ in the blood, raising pulmonary vascular resistance. CO₂ in the abdominal cavity might be sucked into the injured hepatic veins, causing pulmonary embolism. The Pringle maneuver does not adversely affect the Fontan circulation during laparoscopic hepatectomy [ 14 ]. On the other hand, inferior vena cava clamping can easily induce hypotension in the Fontan circulation [ 5 ]. In this case, the patient was placed in the reverse Trendelenburg position, and the CVP was controlled at approximately 10 mmHg during the surgery. The preoperative CVP in the previous surgery was 19 mmHg, and the CVP was controlled at approximately 15 mmHg during the surgery. In the current surgery, the patient was managed by the cardiology department preoperatively, with the preoperative CVP ranging from 10 to 14 mmHg and the intraoperative CVP controlled at 10 mmHg. In case of FALD, minimally invasive surgery, particularly RALH, was considered candidate only when the lesion was small, located on the surface of anterolateral segments, and did not involve major blood vessels, and the Fontan circulation was maintained despite a low CVP. Furthermore, this case involved reoperation, and compared to laparoscopic surgery, the advantages of RALH were considered beneficial for performing precise tasks, such as adhesiolysis, in confined spaces. However, a disadvantage of RALH was the time required to convert to open surgery, which was crucial in cases involving FALD. The indication for RALH in patients with FALD must be carefully determined through close communication with cardiologists and anesthesiologists.
RALH has several disadvantages compared with conventional laparoscopic hepatectomy, including prolonged operation time and increased total cost [ 18 , 19 ]. However, RALH offers several advantages over conventional laparoscopic hepatectomy, including enhanced visualization, improved surgical dexterity, ease of dissection and suturing, and stable camera control. [ 20 , 21 ]. Comparisons between robotic and laparoscopic hepatectomies indicate that both methods are equally safe and feasible in terms of blood loss, transfusion rates, and postoperative complications [ 22 ]. Nevertheless, robotic surgery has a higher rate of performing major hepatectomies in a minimally invasive manner [ 22 ]. In addition, during robotic-assisted laparoscopic surgery, the timing of conversion to open surgery must always be considered because of the risk of intraoperative bleeding and the likelihood of vital sign changes in patients with FALD. Therefore, hepatectomy for HCC arising from FALD requires stricter criteria than conventional hepatectomy. Such criteria may include preoperative CVP to predict the likelihood of intraoperative bleeding from hepatic veins. To establish such criteria, data should be accumulated on patients with FALD by creating a large-scale, nationwide database. In this surgery, the tumor was located on the liver surface; therefore, we were able to perform the hepatectomy relatively easily. In the future, reports on hepatectomy for tumors in the deep liver parenchyma will also be necessary.
In conclusion, our report suggests that RALH for patients with HCC and Fontan circulation can be safely performed in selected patients with sufficient cardiac reserves. A long time has passed since the FP was first performed, and the cases of HCC with congested liver cirrhosis are expected to increase in the future. In addition, because of congestive cirrhosis and carcinogenesis at a young age, recurrence of HCC may be unavoidable. RALH is a desirable minimally invasive surgery for reoperation and maintaining postoperative quality of life. More case reports on RALH for patients with HCC and Fontan circulation are warranted.
We successfully performed RALH in a patient with FALD. To safely perform RALH for HCC in patients who have undergone the FP, thorough preoperative cardiac function assessments, careful decision-making, and close communication between cardiologists and anesthesiologists are necessary.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Carbon dioxide
Computed tomography
- Central venous pressure
- Fontan-associated liver disease
- Fontan procedure
- Hepatocellular carcinoma
Indocyanine green
- Robot-assisted laparoscopic hepatectomy
Rychik J, Veldtman G, Rand E, Russo P, Rome JJ, Krok K, et al. The precarious state of the liver after a Fontan operation: summary of a multidisciplinary symposium. Pediatr Cardiol. 2012;33:1001–12.
Article PubMed PubMed Central Google Scholar
Stanton RE, Lurie PR, Lindesmith GG, Meyer BW. The Fontan procedure for tricuspid atresia. Circulation. 1981;64:40–6.
Google Scholar
Heering G, Lebovics N, Agarwal R, Frishman WH, Lebovics E. Fontan-associated liver disease: a review. Cardiol Rev. 2024. https://doi.org/10.1097/CRD.0000000000000684 .
Article PubMed Google Scholar
Jarasvaraparn C, Thoe J, Rodenbarger A, Masuoka H, Payne RM, Markham LW, et al. Biomarkers of fibrosis and portal hypertension in Fontan-associated liver disease in children and adults. Dig Liver Dis. 2024. https://doi.org/10.1016/j.dld.2023.12.017 .
Nemoto S, Ariizumi SI, Kotera Y, Omori A, Yamashita S, Kato TA, et al. A patient with post-Fontan operation underwent left hepatectomy and caudate lobectomy for hepatocellular carcinoma: a case report. Surg Case Rep. 2020;6:104.
Mori M, Hirano S, Hakamada K, Oki E, Urushidani S, Uyama I, et al. Clinical practice guidelines for telesurgery 2022 committee for the promotion of remote surgery implementation Japan surgical society. Surg Today. 2024. https://doi.org/10.1007/s00595-024-02863-5 .
Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, et al. Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003;138:777–84.
McClain CD, McGowan FX, Kovatsis PG. Laparoscopic surgery in a patient with Fontan physiology. Anesth Analg. 2006;103:856–8.
Asrani SK, Warnes CA, Kamath PS. Hepatocellular carcinoma after the Fontan procedure. N Engl J Med. 2013;368:1756–7.
Article CAS PubMed Google Scholar
Grizzi F, Qehajaj D, Yiu D, Bresalier RS, Chiriva-Internati M. PD-L1, fibrosis, and immunotherapy in hepatocellular carcinoma: the importance of a scientific method to explore observations and answer questions. Surg Today. 2020;50:1318–9.
Kuwabara M, Niwa K, Toyoda T, Shirai T, Tateno S, Ohuchi H, et al. Liver cirrhosis and/or hepatocellular carcinoma occurring late after the Fontan procedure–a nationwide survey in Japan. Circ J. 2018;82:1155–60.
Kiesewetter CH, Sheron N, Vettukattill JJ, Hacking N, Stedman B, Millward-Sadler H, et al. Hepatic changes in the failing Fontan circulation. Heart. 2007;93:579–84.
Yoon JS, Lee DH, Cho EJ, Song MK, Choi YH, Kim GB, et al. Risk of liver cirrhosis and hepatocellular carcinoma after Fontan operation: a need for surveillance. Cancers (Basel). 2020;12:1805.
Yokota Y, Noda T, Kobayashi S, Matsumoto K, Sakano Y, Iwagami Y, et al. A case report of Fontan procedure-related hepatocellular carcinoma: pure laparoscopic approach by low and stable pneumoperitoneum. BMC Surg. 2020;20:80.
Angelico R, Lisignoli V, Monti L, Pariante R, Grimaldi C, Saffioti MC, et al. Laparoscopic liver resection for hepatocellular carcinoma in Fontan-associated chronic liver disease the first case report. Int J Surg Case Rep. 2019;59:144–7.
Takuma Y, Fukada Y, Iwadou S, Miyatake H, Uematsu S, Okamoto R, et al. Surgical resection for hepatocellular carcinoma with cardiac cirrhosis after the Fontan procedure. Intern Med. 2016;55:3265–72.
Shiraishi J, Itoh S, Tomino T, Yoshiya S, Nagao Y, Kayashima H, et al. Surgical treatment of hepatocellular carcinoma after Fontan operation: three case reports and review of the literature. Clin J Gastroenterol. 2023;16:559–66.
Zhang L, Yuan Q, Xu Y, Wang W. Comparative clinical outcomes of robot-assisted liver resection versus laparoscopic liver resection: a meta-analysis. PLoS ONE. 2020;15: e0240593.
Article CAS PubMed PubMed Central Google Scholar
Coletta D, Levi Sandri GB, Giuliani G, Guerra F. Robot-assisted versus conventional laparoscopic major hepatectomies: systematic review with meta-analysis. Int J Med Robot. 2021;17: e2218.
Fruscione M, Pickens R, Baker EH, Cochran A, Khan A, Ocuin L, et al. Robotic-assisted versus laparoscopic major liver resection: analysis of outcomes from a single center. HPB (Oxford). 2019;21:906–11.
Zhang L, Hu C, Qin Q, Li R, Zhao J, Zhang Z, et al. Learning process analysis of robotic lateral pelvic lymph node dissection for local advanced rectal cancer: the CUSUM curve of 78 consecutive patients. Surg Today. 2024;54:220–30.
Tsung A, Geller DA, Sukato DC, Sabbaghian S, Tohme S, Steel J, et al. Robotic versus laparoscopic hepatectomy: a matched comparison. Ann Surg. 2014;259:549–55.
Download references
Acknowledgements
We would like to thank Editage ( www.editage.jp ) for English language editing.
This study was not supported by any funding.
Author information
Authors and affiliations.
Department of Surgery and Science, Graduate School of Medical Sciences, Kyushu University, 3-1 Maidashi, Higashi-Ku, Fukuoka-Shi, Fukuoka, 812-0054, Japan
Takuma Ishikawa, Shinji Itoh, Takeo Toshima, Shohei Yoshiya, Yuki Bekki, Norifumi Iseda, Yuriko Tsutsui & Tomoharu Yoshizumi
Department of Cardiovascular Medicine, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan
Ichiro Sakamoto & Kotaro Abe
You can also search for this author in PubMed Google Scholar
Contributions
Study conception: SI. Writing: TI. Final approval of the article: all authors. Accountability for all aspects of the work: all authors.
Corresponding author
Correspondence to Shinji Itoh .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Written informed consent was obtained from the patient to publish this case report and accompanying images.
Competing interests
The authors declare no conflicts of interest in association with the present study.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Ishikawa, T., Itoh, S., Toshima, T. et al. Robot-assisted laparoscopic hepatectomy for hepatocellular carcinoma with Fontan-associated liver disease: a world-first case report. surg case rep 10 , 210 (2024). https://doi.org/10.1186/s40792-024-02014-5
Download citation
Received : 14 July 2024
Accepted : 31 August 2024
Published : 09 September 2024
DOI : https://doi.org/10.1186/s40792-024-02014-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Case report
- Open access
- Published: 07 September 2024
Progressive familial intrahepatic cholestasis type 4: a case report
- Mohamed Abdelmalak Abokandil 1 ,
- Saber Waheeb 1 , 2 ,
- Wessam Zaghloul 1 , 2 ,
- Manal Abdelgawad 1 , 2 ,
- Mona Abdelhady 2 ,
- Mohamed Mansy 1 , 3 &
- Mostafa Kotb ORCID: orcid.org/0000-0002-2558-3551 1 , 2
Journal of Medical Case Reports volume 18 , Article number: 434 ( 2024 ) Cite this article
Metrics details
Progressive familial intrahepatic cholestasis is an autosomal recessive genetic disorder that manifests primarily with jaundice and pruritus and can progresses from persistent cholestasis to cirrhosis and late childhood liver failure. Classically, progressive familial intrahepatic cholestasis is classified into three subtypes: 1, 2, and 3 and results from a defect in a biliary protein responsible for bile formation and circulation in the liver. In the last decade and with the increased use of genetic testing, more types have been known.
Case presentation
A 6-month-old Afrocentric boy presented with progressive jaundice and pruritus that started since the age of 2 months. He was thoroughly investigated to be finally diagnosed as progressive familial intrahepatic cholestasis type 4. A low-fat diet, ursodeoxycholic acid, fat-soluble vitamins, and cholestyramine were started. He showed initial improvement then had refractory pruritus and impaired quality of life. He underwent surgical biliary diversion at the age of 1 year with marked improvement of manifestations.
Owing to the increased technology of genetic testing, more clinical subtypes of progressive familial intrahepatic cholestasis were diagnosed other than the classical three types. Surgical management using biliary diversion could be beneficial and delays or may even obviate the need for liver transplantation.
Peer Review reports
Introduction
Progressive familial intrahepatic cholestasis (PFIC) is a group of rare autosomal recessive genetic disorders involving defects in bile acid secretion or transport. There are a wide spectrum of manifestations ranging from neonatal cholestasis, recurrent cholestasis, refractory pruritus, growth failure, childhood liver failure, and portal hypertension to advanced end-stage liver disease [ 1 , 2 ]. Classically, PFIC is classified into three subtypes: PFIC1, PFIC2, and PFIC3 according to the timing of their discovery. PFIC1 (Byler’s disease) involves FIC1 deficiency due to mutations in the ATPase phospholipid transporting 8B1 (ATP8B1) gene. PFIC2, which is the most common subtype involves a defective or deficient severe bile salt export pump (BSEP) caused by a mutation in the ATP-binding cassette subfamily B member 11 (ABCB11) gene. PFIC3 is due to multidrug resistance protein 3 (MDR3) deficiency resulting from a mutation in the ABCB4 gene [ 3 , 4 , 5 ].
With the advancements in genetic analyses, newer subtypes are being discovered. PFIC4 was first reported in 1991 by Gumbiner et al . [ 6 , 7 ]. In PFIC4, there is deficiency in a protein called tight junction protein 2 (TJP2) or zona occludens 2 due to mutation in the tight junction protein 2 (TJP2) gene. This results in reduced integrity of the canalicular membrane and reflux of bile acids into hepatocytes, with their deleterious effect in potentiating hepatocyte damage and cholestasis [ 7 , 8 ]. TJP2 has a widespread expression, including the respiratory and central nervous systems [ 8 ].
Clinically, cases with PFIC4 can present with mild anicteric pruritus, recurrent cholestasis, or severe progressive liver disease [ 4 , 8 ]. Extrahepatic manifestations in the form of neurological and respiratory symptoms can be present in these cases [ 7 ]. Similar to PFIC2, there is increased risk of progression to hepatocellular carcinoma (HCC) in PFIC4 [ 7 , 9 , 10 ]. Thus, early diagnosis, treatment, and close follow-up is mandatory.
Investigations in PFIC4 typically show elevated total and direct serum bilirubin with low to normal serum gamma glutamyl transferase (GGT). Liver enzymes are elevated in these cases as well as serum bile acids [ 7 ]. Liver histopathology classically reveals canalicular cholestasis along with a variable degree of fibrosis and giant cell transformation. Electron microscopy shows elongated tight junctions and a lack of the densest part of the zona occludens [ 11 ]. Molecular genetic diagnosis is considered the test of choice in diagnosing PFIC type as it is noninvasive unlike liver biopsy. This can be done using next-generation sequencing (NGS) [ 12 ]. Whole-exome (WES) or whole-genome (WGS) sequencing can be done in cases with negative targeted gene analysis.
Genetic counseling for parents is crucial as it is an autosomal recessive disorder. Nutritional management with providing adequate calories [125–140% of the recommended dietary allowances ( RDA)], protein (2–3 g/kg daily), and a low-fat diet is crucial. Supplementation of medium-chain triglycerides (MCT) and fat-soluble vitamins is recommended [ 13 ]. Regular monitoring of growth parameters and nutritional deficiencies is important as those cases are liable for growth failure.
Pruritus is the most devastating manifestation in PFIC. It can affect the quality of life. Local skin emollients, ursodeoxycholic acid (UDCA), cholestyramine, antihistamines, rifampicin, naltrexone, and sertraline are used to control pruritus [ 14 ]. Some cases respond well to these medications. Others can have deterioration in liver status or refractory itching despite drug therapy, necessitating biliary diversion or liver transplantation [ 15 ].
Biliary diversion (BD) procedures aim at the diversion of bile from the intestine, reducing the reabsorption of bile through enterohepatic circulation [ 16 ]. This reduces the accumulation of bile acids. BD has good results in the alleviation of refractory pruritus in PFIC1 and 2 [ 17 ]. Its role in the newer variants of PFIC is not yet well known. We report a case with PFIC4 who had refractory pruritus for which he underwent surgical biliary diversion.
A 6-month-old Afrocentric boy presented to our institute with a 3-month history of progressive generalized jaundice and persistent pruritus. History revealed that the parents were cousins. No family history of cholestasis or hepatic disease was reported. On clinical examination, the patient was markedly icteric and pale. His growth parameters were affected; weight −1.8 standard deviation (SD), length −1.5 SD, and mid upper arm circumference 12 cm, despite being within the normal range at birth (weight 0.7 SD and length 0.9 SD). He had marked hepatomegaly, but no splenomegaly or ascites. He had scratch marks allover his body, especially around in his face. His urine was dark.
His investigations showed direct hyperbilirubinemia along with elevation of liver enzymes and serum bile acids. On the other hand, gamma-glutamyl transpeptidase (GGT), serum albumin, and coagulation profiles were within normal ranges (Table 1 ). At this stage, biliary atresia and other causes of obstructive jaundice in this age group such as PFIC, Alagille syndrome, and inspissated bile syndrome were considered. Percutaneous ultrasound (US)-guided liver biopsy revealed marked pseudoglandular transformation of almost all of the hepatocytes with canalicular cholestasis, florid ductular proliferation, and mild ductopenia (Fig. 1 A and B). Thus, PFIC was the prime consideration.

A , B Prominent pseudoglandular transformation and canalicular cholestasis (arrows). Hematoxylin and eosin stain ( A ×100, B ×200). C Diagrammatic illustration of the operation performed. D , E Marked improvement of jaundice and growth
The patient was on nutritional management with adequate calories and proteins in addition to MCT. He was on high doses of vitamin D (2000 units/day) based on his serum vitamin D level. He also received the recommended daily doses of vitamins A and E. UDCA dose was escalated according to clinical and laboratory findings. Cholestyramine was added in maximum doses with initial control of pruritus, then became nonbeneficial.
Whole-exome sequencing was done to detect the exact genetic mutation. A homozygous pathogenic variant in TJP2 was identified, which was consistent with the diagnosis of progressive familial intrahepatic cholestasis type 4 (OMIM: 615878). The patient continued on his nutritional and medical management till 1 year of age; however, he still had growth failure and worsening of pruritus with evident scarring and impaired quality of life.
The patient was scheduled for partial internal diversion. On exploration, the gallbladder was found to be dilated with thickened wall. A 15-cm-long jejeunal segment was isolated with its blood supply, 40 cm from the duodenojejunal junction, and passed retrocoloic for anastomosis with the gallbladder. The proximal stump was closed and side-to-side jejunocolic anastomosis was done, while the distal end was anastomosed with the transverse colon in an end-to-side fashion. Restoration of the bowel continuity was done by end-to-end jejunojejunal anastomosis (Fig. 1 C).
Postoperatively, the patient was doing well after 18 months of follow-up with marked drop in the level of total and direct bilirubin, improvement in the growth pattern (weight 0.9 SD, length 0.5 SD) and relief of pruritus (Fig. 1 D, E).
PFIC type 4 represents a new entity of PFIC that evolved after the advances in genetic testing. The exact incidence of PFIC4 is not well known due to the limited number of studies, which are mostly case reports or small case series [ 7 ]. PFIC1 and PFIC 2 usually occur in early infancy and are caused by a mutation in the ATP8B1 and ABCB11 genes, respectively. They are characterized by having a normal level of GGT, compared to PFIC3, that occurs in adolescents due to a mutation in the ABCB4 gene and has high GGT levels [ 1 , 2 ]. In PFIC4, there is a mutation in the TJP2 gene, which is a member of the membrane-associated guanylate kinase homolog family, located on the long arm of chromosome 9. It encodes a protein called tight junction protein 2 (TJP2). This encoded protein is an integral component of the tight junction barrier in epithelial and endothelial cells, which are crucial for proper assembly of tight junctions. Deficiency of TJP2 protein results in reduced integrity of the canalicular membrane and reflux of bile acids through the intercellular spaces into the hepatocytes, causing liver damage and progressive cholestasis [ 8 , 18 ]. All homozygous mutations cause deficient TJP2 protein and complete loss of function. Missense and frame deletion lead to milder disease due to residual TJP2 protein expression [ 19 , 20 ].
Medical treatment for PFIC4 using UDCA (10–30 mg/kg/day), fat-soluble vitamins, MCT, and cholestyramine (240–400 mg/kg/day) can be effective in some cases [ 14 , 21 ]. Surgery is indicated if there is intractable pruritus despite optimum treatment. Other indications include failure to thrive and nutritional deficiencies. Sambrotta et al . reported 12 cases with PFIC4; 9 cases (75%) required liver transplantation (LT) while 2 had portal hypertension [ 19 ]. On the other hand, Zhang et al . reported 7 cases and none of them required LT; all of them responded well to medical treatment [ 20 ].
Biliary diversion in PFIC is indicated for children who do not yet have advanced fibrosis or liver cirrhosis. [ 15 ] Regardless of the adopted technique, the main aim is to interfere with enterohepatic recirculation of bile salt leading to bile salt pool depletion; hence, pruritus decreases and the progression to cirrhosis is delayed. This can be achieved either by anastomosis of the biliary tract to the outside skin using a jejunal loop as a conduit as a stoma (external drainage) or to the intestines (internal drainage). The latter has now gained ground and can be performed by anastomosing the gall bladder via a jejunal (cholecystojejunocolic), ileal (cholecystojejunocolic), appendix (cholecystoappendicocolic) conduit to the colon or directly between gall bladder and antireflux loop of colon (cholecystocolocolic anastomosis) [ 22 ].
Concerning biliary diversion surgeries, a meta-analysis yielded a 60% incidence of pruritus relief and only a 27% need for liver transplantation [ 23 ]. They also found that partial internal biliary diversion using a chole-cystojejunocolic approach has lower complications and liver transplantation requirement than partial extrabiliary diversion using appendix or jejunum [ 23 ].
Conclusions
Owing to the advances in genetic testing, more clinical subtypes of PFIC have been diagnosed, other than the classical three types. Surgical management using biliary diversion could be beneficial and could delay or even obviate the need for liver transplantation. The CARE Checklist has been completed by the authors for this case report, attached as supplementary material.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Bull LN, Thompson RJ. Progressive familial intrahepatic cholestasis. Clin Liver Dis. 2018;22(4):657–69.
Article PubMed Google Scholar
Srivastava A. Progressive familial intrahepatic cholestasis. J Clin Exp Hepatol. 2014;4(1):25–36.
Baker A, Kerkar N, Todorova L, Kamath BM, Houwen RHJ. Systematic review of progressive familial intrahepatic cholestasis. Clin Res Hepatol Gastroenterol. 2019;43(1):20–36.
Sharma A, Poddar U, Agnihotry S, Phadke SR, Yachha SK, Aggarwal R. Spectrum of genomic variations in Indian patients with progressive familial intrahepatic cholestasis. BMC Gastroenterol. 2018;18(1):1–10.
Article Google Scholar
Pawlikowska L, Strautnieks S, Jankowska I, Czubkowski P, Emerick K, Antoniou A, et al . Differences in presentation and progression between severe FIC1 and BSEP deficiencies. J Hepatol. 2010;53(1):170–8.
Article PubMed PubMed Central Google Scholar
Gumbiner B, Lowenkopf T, Apatira D. Identification of a 160-kDa polypeptide that binds to the tight junction protein ZO-1. Proc Natl Acad Sci U S A. 1991;88:3460–4.
Article CAS PubMed PubMed Central Google Scholar
Vinayagamoorthy V, Srivastava A, Sarma MS. Newer variants of progressive familial intrahepatic cholestasis. World J Hepatol. 2021;13(12):2024.
Sambrotta M, Thompson RJ. Mutations in TJP2, encoding zona occludens 2, and liver disease. Tissue Barriers. 2015;3: e1026537.
Vij M, Shanmugam NP, Reddy MS, Sankaranarayanan S, Rela M. Paediatric hepatocellular carcinoma in tight junction protein 2 (TJP2) deficiency. Virchows Arch. 2017;471:679–83.
Article CAS PubMed Google Scholar
Wei CS, Becher N, Friis JB, Ott P, Vogel I, Grønbæk H. New tight junction protein 2 variant causing progressive familial intrahepatic cholestasis type 4 in adults: a case report. World J Gastroenterol. 2020;26:550–61.
Gomez-Ospina N, Potter CJ, Xiao R, Manickam K, Kim MS, Kim KH, et al . Mutations in the nuclear bile acid receptor FXR cause progressive familial intrahepatic cholestasis. Nat Commun. 2016;7:10713.
Togawa T, Sugiura T, Ito K, Endo T, Aoyama K, Ohashi K, et al . Molecular genetic dissection and neonatal/infantile intrahepatic cholestasis using targeted next-generation sequencing. J Pediatr. 2016;171:171-7.e1.
Lane E, Murray KF. Neonatal cholestasis. Pediatr Clin N Am. 2017;64:621–39.
Thébaut A, Debray D, Gonzales E. An update on the physiopathology and therapeutic management of cholestatic pruritus in children. Clin Res Hepatol Gastroenterol. 2018;42:103–9.
Wang KS, Tiao G, Bass LM, Hertel PM, Mogul D, Kerkar N, et al . Analysis of surgical interruption of the enterohepatic circulation as a treatment for pediatric cholestasis. Hepatology. 2017;65(5):1645–54.
Lemoine C, Superina R. Surgical diversion of enterohepatic circulation in pediatric cholestasis. Semin Pediatr Surg. 2020;29: 150946.
Verkade HJ, Thompson RJ, Arnell H, Fischler B, Gillberg PG, Mattsson JP, et al . Systematic review and meta-analysis: partial external biliary diversion in progressive familial intrahepatic cholestasis. J Pediatr Gastroenterol Nutr. 2020;71:176–83.
Mirza N, Bharadwaj R, Malhotra S, Sibal A. Progressive familial intrahepatic cholestasis type 4 in an Indian child: presentation, initial course and novel compound heterozygous mutation. BMJ Case Rep. 2020;13: e234193.
Sambrotta M, Strautnieks S, Papouli E, Rushton P, Clark BE, Parry DA, et al . Mutations in TJP2 cause progressive cholestatic liver disease. Nat Genet. 2014;46:326–8.
Zhang J, Liu LL, Gong JY, Hao CZ, Qiu YL, Lu Y, et al . TJP2 hepatobiliary disorders: novel variants and clinical diversity. Hum Mutat. 2020;41:502–11.
Alam S, Lal BB. Recent updates on progressive familial intrahepatic cholestasis types 1, 2 and 3: outcome and therapeutic strategies. World J Hepatol. 2022;14(1):98.
Gunaydin M, Bozkurter Cil AT. Progressive familial intrahepatic cholestasis: diagnosis, management, and treatment. Hepat Med. 2018;10:95–104.
Bolia R, Goel AD, Sharma V, Srivastava A. Biliary diversion in progressive familial intrahepatic cholestasis: a systematic review and meta-analysis. Expert Rev Gastroenterol Hepatol. 2022;16:163–72.
Download references
Acknowledgements
Not applicable.
There was no funding source for this report.
Author information
Authors and affiliations.
Nile of Hope Hospital for Congenital Anomalies, Alexandria, Egypt
Mohamed Abdelmalak Abokandil, Saber Waheeb, Wessam Zaghloul, Manal Abdelgawad, Mohamed Mansy & Mostafa Kotb
Faculty of Medicine, Alexandria University, Alexandria, Egypt
Saber Waheeb, Wessam Zaghloul, Manal Abdelgawad, Mona Abdelhady & Mostafa Kotb
Faculty of Medicine, Port Said University, Port Said, Egypt
Mohamed Mansy
You can also search for this author in PubMed Google Scholar
Contributions
M. Abokandil, M. Abdelgawad, and S. Waheeb made and confirmed the diagnosis, provided the details of the case, and contributed to the design of the report. M. Abdelhady provided the pathological diagnosis. W. Zaghloul, M. Mansy, and M. Kotb drafted the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Mostafa Kotb .
Ethics declarations
Ethics approval and consent to participate.
Written informed consent was obtained from the patient for publication of the details of her medical case and any accompanying images. The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
Consent for publication
Written informed consent was obtained from the patient’s legal guardian for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Abokandil, M.A., Waheeb, S., Zaghloul, W. et al. Progressive familial intrahepatic cholestasis type 4: a case report. J Med Case Reports 18 , 434 (2024). https://doi.org/10.1186/s13256-024-04662-5
Download citation
Received : 29 August 2023
Accepted : 13 May 2024
Published : 07 September 2024
DOI : https://doi.org/10.1186/s13256-024-04662-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Progressive familial intrahepatic cholestasis
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Hev infection in the context of prior hbv-related liver injury: case series.

1. Introduction
2. case series, 3. materials and methods, 4. discussions, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, acknowledgments, conflicts of interest.
- Teshale, E. Hepatitis E. In CDC Yellow Book 2024 ; Oxford University Press: Oxford, UK, 2023. Available online: https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/hepatitis-e (accessed on 30 August 2024).
- Song, Y.-J.; Park, W.-J.; Park, B.-J.; Lee, J.-B.; Park, S.-Y.; Song, C.-S.; Lee, N.-H.; Seo, K.-H.; Kang, Y.-S.; Choi, I.-S. Hepatitis E virus infections in humans and animals. Clin. Exp. Vaccine Res. 2014 , 3 , 29. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Trickey, A.; Bivegete, S.; Duffell, E.; McNaughton, A.L.; Nerlander, L.; Walker, J.G.; Fraser, H.; Hickman, M.; Vickerman, P.; Brooks-Pollock, E.; et al. Estimating hepatitis B virus prevalence among key population groups for European Union and European Economic Area countries and the United Kingdom: A modelling study. BMC Infect. Dis. 2023 , 23 , 457. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Popovici, O. Rezultatele Studiului Sero-Epidemiologic de Prevalenta Pentru Infectia cu Virus Hepatitic B si C, Romania, Anul 2013 ; Institutul National de Sanatate Publica Romania: Bucuresti, Romania, 2013. Available online: https://www.cnscbt.ro/index.php/analiza-date-supraveghere/hepatita-virala-tip-b-si-c/405-rezultatele-studiului-epidemiologic-de-prevalenta-pentru-infectia-cu-virus-hepatitic-b-si-c-romania-anul-2013/file (accessed on 23 July 2024).
- Mrzljak, A.; Dinjar-Kujundzic, P.; Jemersic, L.; Prpic, J.; Barbic, L.; Savic, V.; Stevanovic, V.; Vilibic-Cavlek, T. Epidemiology of hepatitis E in south-East Europe in the “One Health” concept. World J. Gastroenterol. 2019 , 25 , 3168. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6626717/ (accessed on 23 July 2024). [ CrossRef ] [ PubMed ]
- Aspinall, E.J.; Couturier, E.; Faber, M.; Said, B.; Ijaz, S.; Tavoschi, L.; Takkinen, J.; Adlhoch, C., on behalf of the country experts. Hepatitis E virus infection in Europe: Surveillance and descriptive epidemiology of confirmed cases, 2005 to 2015. Eurosurveillamce 2017 , 22 , 35061. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cheng, S.-H.; Mai, L.; Zhu, F.-Q.; Pan, X.-F.; Sun, H.-X.; Cao, H.; Shu, X.; Ke, W.-M.; Li, G.; Xu, Q.-H. Influence of chronic HBV infection on superimposed acute hepatitis E. World J. Gastroenterol. 2013 , 19 , 5904–5909. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3793145/ (accessed on 21 September 2013). [ CrossRef ] [ PubMed ]
- Chen, C.; Zhang, S.-Y.; Zhang, D.-D.; Li, X.-Y.; Zhang, Y.-L.; Li, W.-X.; Yan, J.-J.; Wang, M.; Xun, J.-N.; Lu, C.; et al. Clinical features of Acute Hepatitis E super-infections on chronic hepatitis B. World J. Gastroenterol. 2016 , 22 , 10388. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5175251/ (accessed on 2 July 2024). [ CrossRef ] [ PubMed ]
- Shalimar; Kedia, S.; Mahapatra, S.J.; Nayak, B.; Gunjan, D.; Thakur, B.; Acharya, S.K. Severity and outcome of acute-on-chronic liver failure is dependent on the etiology of acute hepatic insults: Analysis of 368 patients. J. Clin. Gastroenterol. 2017 , 51 , 734–741. Available online: https://pubmed.ncbi.nlm.nih.gov/28296656/ (accessed on 2 July 2024). [ CrossRef ] [ PubMed ]
- Shalimar; Kumar, D.; Vadiraja, P.K.; Nayak, B.; Thakur, B.; Das, P.; Gupta, S.D.; Panda, S.K.; Acharya, S.K. Acute on chronic liver failure because of acute hepatic insults: Etiologies, course, extrahepatic organ failure and predictors of mortality. J. Gastroenterol. Hepatol. 2016 , 31 , 857–864. Available online: https://pubmed.ncbi.nlm.nih.gov/26519215/ (accessed on 4 July 2024).
- Tseng, T.C.; Liu, C.J.; Chang, C.T.; Su, T.H.; Yang, W.T.; Tsai, C.H.; Chen, C.L.; Yang, H.C.; Liu, C.H.; Chen, P.J.; et al. HEV superinfection accelerates disease progression in patients with chronic HBV infection and increases mortality in those with cirrhosis. J. Hepatol. 2020 , 72 , 1105–1111. Available online: https://pubmed.ncbi.nlm.nih.gov/32006586/ (accessed on 3 July 2024). [ CrossRef ] [ PubMed ]
- Chow, C.W.; Tsang, S.W.; Tsang, O.T.; Leung, V.K.; Fung, K.S.; Luk, W.K.; Chau, T.N. Comparison of acute hepatitis E infection outcome in patients with and without chronic hepatitis B infection: A 10 year retrospective study in three regional hospitals in Hong Kong. J. Clin. Virol. 2014 , 60 , 4–10. Available online: https://pubmed.ncbi.nlm.nih.gov/24646686/ (accessed on 3 July 2024). [ CrossRef ] [ PubMed ]
- Zhao, H.; Ye, W.; Yu, X.; Hu, J.; Zhang, X.; Yang, M.; Sheng, J.; Shi, Y. Hepatitis E virus superinfection impairs long-term outcome in hospitalized patients with hepatitis B virus-related decompensated liver cirrhosis. Ann. Hepatol. 2023 , 28 , 100878. Available online: https://pubmed.ncbi.nlm.nih.gov/36417965/ (accessed on 3 July 2024). [ CrossRef ] [ PubMed ]
- Hoan, N.X.; Tong, H.V.; Hecht, N.; Sy, B.T.; Marcinek, P.; Meyer, C.G.; Song, L.H.; Toan, N.L.; Kurreck, J.; Kremsner, P.G.; et al. Hepatitis E virus superinfection and clinical progression in hepatitis B patients. EbioMedicine 2015 , 2 , 2080–2086. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4703726/ (accessed on 4 July 2024). [ CrossRef ] [ PubMed ]
- Zhang, X.; Ke, W.; Xie, J.; Zhao, Z.; Xie, D.; Gao, Z. Comparison of effects of hepatitis E or a viral superinfection in patients with chronic hepatitis B. Hepatol. Int. 2010 , 4 , 615–620. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2940009/ (accessed on 4 July 2024). [ CrossRef ] [ PubMed ]
- Hyams, C.; Mabayoje, D.A.; Copping, R.; Maranao, D.; Patel, M.; Labbett, W.; Haque, T.; Webster, D.P. Serological cross reactivity to CMV and EBV causes problems in the diagnosis of acute hepatitis E virus infection. J. Med. Viral. 2013 , 86 , 478–483. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Huang, Q.; Li, X.; Zhu, C.; Yan, J.; Song, Z.; Zhang, S.; Hu, Y.; Chen, L.; Ling, Y. Acute Viral Hepatitis Presenting as Cytomegalovirus, Hepatitis E and Epstein-Barr virus IgM Antibody Positive. Antivir. Ther. 2015 , 21 , 171–173. [ Google Scholar ] [ CrossRef ] [ PubMed ]
| Case Number | AgHBs | HBcAb IgG | HBeAg | HBeAb | VHEAb IgM | VHBViral Load | VHDAb IgG |
|---|---|---|---|---|---|---|---|
| 1 | + | + | − | + | + | Test not performed | − |
| 2 | + | + | − | + | + | 38,700,000 IU/mL | + |
| 3 | + | + | + | − | + | Test not performed | − |
| 4 | + | + | − | + | + | 20,000,000 IU/mL | − |
| 5 | + | + | − | + | + | Test not performed | − |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Olariu, M.-C.; Filipescu, M.-C.; Pauna, A.M.; Simoiu, M.; Borcan, A.M. HEV Infection in the Context of Prior HBV-Related Liver Injury: Case Series. Infect. Dis. Rep. 2024 , 16 , 888-893. https://doi.org/10.3390/idr16050070
Olariu M-C, Filipescu M-C, Pauna AM, Simoiu M, Borcan AM. HEV Infection in the Context of Prior HBV-Related Liver Injury: Case Series. Infectious Disease Reports . 2024; 16(5):888-893. https://doi.org/10.3390/idr16050070
Olariu, Mihaela-Cristina, Mihai-Cezar Filipescu, Andreea Marilena Pauna, Madalina Simoiu, and Alina Maria Borcan. 2024. "HEV Infection in the Context of Prior HBV-Related Liver Injury: Case Series" Infectious Disease Reports 16, no. 5: 888-893. https://doi.org/10.3390/idr16050070
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

COMMENTS
Educational Case: Evaluating a patient with cirrhosis - PMC
Cirrhosis Case Discussion - Michigan Medicine
Spontaneous bacterial peritonitis (neutrophil count >250) Diuretics are held - given IV albumin (1.5g/kg body weight), ceftriaxone and lactulose. Day 3 - Given IV albumin again (1gm/kg body weight). Remains confused, disoriented. Still with asterixis Rifaximin 550mg bid was added to regimen and lactulose dose adjusted to 30cc po twice daily ...
Alcohol-related liver disease (ArLD) is a major cause of morbidity and mortality. Effective management requires multi-disciplinary input at every stage of the disease trajectory. We present a typical case to illustrate current evidence-based investigation and management of a patient with ArLD. This case-based review aims to concisely support the day-to-day decision making of clinicians looking ...
Cirrhosis: Diagnosis and Management
Evidence-based clinical practice guidelines for Liver ...
Here, we report the case of a patient presenting with cirrhosis of the liver due to autoimmune hepatitis along with systemic sclerosis. Case presentation A 51-year-old non-obese female with no history of alcoholism was admitted with complaints of gradually progressive abdominal distension and swelling over both lower limbs for the last month.
This case presentation discusses a 56-year-old male patient with a history of alcohol use who presented with melena and was diagnosed with liver cirrhosis complicated by hepatic encephalopathy and esophageal varices. The patient's condition has progressively worsened, as evidenced by altered mental status, impaired nutrition, and functional decline. His daughter has taken on the primary ...
Case Presentation Liver Cirrhosis - Free download as PDF File (.pdf), Text File (.txt) or read online for free. This case presentation discusses a 67-year-old man with liver cirrhosis and a history of alcohol abuse who presented with hematemesis. Liver cirrhosis is a progressive condition caused by scar tissue replacing healthy liver tissue as a result of chronic alcohol abuse or other factors.
Download ppt "Cirrhosis of the Liver Ch. 44 Case Study". Learning Objectives Identify 3 possible causes of cirrhosis List the clinical manifestations of cirrhosis Name 2 laboratory tests used to assess liver function List 3 nurisng interventions for a patient with cirrhosis.
If liver cirrhosis is diagnosed early and the cause is treated, further damage can be limited and, rarely, reversed. ... Case Presentation: A male patient of Two and half years from Shiwangaon MO ...
Liver cirrhosis is a chronic liver disease that results in scarring and damage to liver tissue, affecting liver function and overall health. Learn about the causes, symptoms, and treatment options available to manage this condition. ... During download, if you can't get a presentation, the file might be deleted by the publisher. E N D ...
Liver cirrhosis is a disease in which normal tissue of liver replaced with scar tissue, ... Severe conditions leads towards liver transplantation. Case Presentation A 45 years 78-kgs Asian man was presented to sheikh zayed hospital Rahim yar khan Pakistan. He was experiencing generalized body weakness, brownish
Hepatic Cirrhosis - StatPearls
and mixed connective tissue disorders is infrequent [3,4]. Here, we report the case of a patient presenting with cirrhosis of the liver due to autoimmune hepatitis along with systemic sclerosis. Case Presentation A 51-year-old non-obese female with no history of alcoholism was admitted with complaints of gradually
This alcoholic liver case study presents a patient with liver cirrhosis. A 43-year-old man was brought into the hospital with a complaints of loss of appetite, abdominal distention, and arrhythmia. He also experienced itchy skin and blood in the stool. The patient's family rushed him into the hospital, and he was in a half-conscious state.
Case Study on Cirrhosis of Liver - Free download as Word Doc (.doc), PDF File (.pdf), Text File (.txt) or read online for free. This document contains a biodata and medical history of a patient named Mr. Rameshwar who was admitted to the hospital with cirrhosis of the liver. It includes sections on his personal information, medical history, physical examination findings, description of ...
Here, we report the case of a patient presenting with cirrhosis of the liver due to autoimmune hepatitis along with systemic sclerosis. Case Presentation A 51-year-old non-obese female with no history of alcoholism was admitted with complaints of gradually progressive abdominal distension and swelling over both lower limbs for the last month.
Liver complications after undergoing the Fontan procedure (FP) are classified as Fontan-associated liver disease (FALD) [].The first report of FALD was by Stanton et al. in 1981 when cirrhosis was found in an autopsy case who died of a fatal arrhythmia 21 months after the FP [].FALD is a severe complication, particularly in adult patients who have undergone the FP [].
Progressive familial intrahepatic cholestasis is an autosomal recessive genetic disorder that manifests primarily with jaundice and pruritus and can progresses from persistent cholestasis to cirrhosis and late childhood liver failure. Classically, progressive familial intrahepatic cholestasis is classified into three subtypes: 1, 2, and 3 and results from a defect in a biliary protein ...
Hepatitis E virus (HEV) is a common cause of acute hepatitis, with increasing incidence in Europe, including Romania. Concurrently, Romania has a high prevalence of chronic hepatitis B (CHB). There is limited research on the clinical presentation and outcomes of HEV infection in patients with pre-existing chronic hepatitis B (CHB), especially in resource-rich settings. Most literature data ...