Antonella: ‘A Stranger in the Family’—A Case Study of Eating Disorders Across Cultures
- Open Access
- First Online: 12 December 2020

Cite this chapter
You have full access to this open access chapter

- Vincenzo Di Nicola 6 , 7
8373 Accesses
2 Citations
7 Altmetric
The story of Antonella illustrates the way in which cultural and other values impact on the presentation and treatment of eating disorders. Displaced from her European home culture to live in Canada, Antonella presents with an eating disorder and a fluctuating tableau of anxiety and mood symptoms linked to her lack of a sense of identity. These arose against a background of her adoption as a foundling child in Italy and her attachment problems with her adoptive family generating chronically unfixed and unstable identities, resulting in her cross-cultural marriage as both flight and refuge followed by intense conflicts. Her predicament is resolved only when after an extended period in cultural family therapy she establishes a deep cross-species identification by becoming a breeder of husky dogs. The wider implications of Antonella’s story for understanding the relationship between cultural values and mental health are briefly considered.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others

Overlaps and Disjunctures: A Cultural Case Study of a British Indian Young Woman’s Experiences of Bulimia Nervosa
René girard and the mimetic nature of eating disorders, the rise of eating disorders in asia: a review.
- Eating disorders
- Anorexia multiforme
- Cultural values
- Uniqueness of the individual
- Role of animals
- Cross-species identification
- Cultural family therapy
1 Introduction
Eating disorders are a potentially fruitful area of study for understanding the links between values—in particular cultural values—and mental distress and disorder. Eating disorders show widely different prevalence rates across cultures, and much attention has been given to theories linking these differences with variations in cultural values. In particular, the cultural value placed on ‘fashionable slimness’ in the industrialised world has for some time been identified with the greater prevalence of eating disorders among women in Western societies [ 1 ]. Consistently with this view, the growing prevalence of eating disorders in other parts of the world does seem to be correlated with increasing industrialisation [ 2 , 3 ]. In my review of cultural distribution and historical evolution of eating disorders , I was so struck by its protean nature and its variability of clinical presentations of anorexia nervosa that I renamed this predicament ‘anorexia multiforme’ [ 4 , 5 ].
The story of Antonella that follows illustrates the potential importance of contemporary theories linking cultural values with eating disorders though also some of their limitations.
2 Case Narrative: Antonella’s Story
Ottawa in the early 1990s. Antonella Trevisan, a 24-year-old woman, was referred to me by an Italian psychiatrist and family therapist, Dr. Claudio Angelo, who had treated her in Italy [ 6 ] . When Antonella came to Canada to live with a man she had met through her work, Dr. Angelo referred her to me. Antonella’s presenting problems concerned two areas of her life: her eating problems, which emerged after her emigration from Italy, and her relationship with her partner in Canada.
2.1 Antonella’s Predicament
My initial psychiatric consultation (conducted in Italian) revealed the complexities of Antonella’s life. This was reflected in the difficulty of making an accurate diagnosis. Her food-related problems had some features of eating disorders , such as restriction of intake, the resulting weight loss, and a history of weight gain and being teased for it. What was missing was the ‘psychological engine’ of an eating disorder: a drive for thinness or a morbid fear of fatness. Her problem was perhaps better understood as a food-related anxiety arising from a ‘globus’ sensation (lump in the throat) and a learned avoidance response that generalized from one specific situation to eating in any context.
Although it was clear that her weight gain in late adolescence and the teasing and insults from her mother had sensitized her, other factors had to be considered. Antonella showed an exquisite rejection sensitivity that both arose from and was a metaphor for the circumstances of her birth and adoption. Her migration to Canada also seemed to generate anxieties and uncertainties, and there were hints of conflicts with her partner. Was she also re-enacting another, earlier trauma? In the first journey of her life, she was given up by her birth mother (or taken away?) and left on the steps of a foundry. In the first year of her life, Antonella had shown failure to thrive and developmental delays. And she had, at best, an insecure attachment to her adoptive family, predisposing her to lifelong insecurities.
2.2 A Therapeutic Buffet
After my assessment, we faced a choice: whether to treat the eating problem concretely, in purely behavioral terms, or more metaphorically, with some form of psychotherapy. Given the stabilization of her eating pattern and her weight and the larger context of her predicament, we negotiated to do psychotherapy. There were several components to her therapy. Starting with a psychiatric consultation, three types of therapy were negotiated, with Antonella sampling a kind of ‘therapeutic buffet’ over a period of some 2 years: individual therapy for Antonella, couple therapy for Antonella and Rick, and brief family therapy with Antonella’s adoptive family visiting from Italy.
The individual work with Antonella was at first exploratory, getting to know the complex bicultural world of the Italian Alps, how she experienced the move to Canada, examining her choices to move here and live with Rick. Sessions were conducted in a mix of Italian and English. At first, the Italian language was like a ‘transitional object’ in her acculturation process; slowly, as she gained confidence in her daily life, English began to dominate her sessions. Under stress, however, she would revert to Italian. I could follow her progress just by noting the balance of Italian and English in each session. This does not imply any superiority of English or language preferences; rather, it acknowledges the social realities of culture making its demands felt even in private encounters. This is the territory of sociolinguistics [ 7 , 8 ] . Like Italian, these individual sessions were a secure home base to which Antonella returned during times of stress or between other attempts to find solutions.
After some months in Canada and the stabilization of her eating problems, Antonella became more invested in examining her relationship to Rick. They had met through work while she was still in Italy. After communicating on the telephone, she daringly took him up on an offer to visit. During her holiday in Canada, a romance developed. After her return to Italy, Antonella made the extraordinary decision to emigrate, giving up an excellent position in industry, leaving her family for a country she did not know well. Rick is 22 years her senior and was only recently separated from his first wife.
In therapy she not only expressed ambivalence about her situation with Rick but enacted it. She asked for couple sessions to discuss some difficulties in their relationship. Beyond collecting basic information, couple sessions were unproductive. While Rick was frank about his physical attraction to her and his desire to have children, Antonella talked about their relationship in an oddly detached way. She could not quite articulate her concerns. As we got closer to examining the problems of their relationship, Antonella abruptly announced that they were planning their wedding. The conjoint sessions were put on hold as they dealt with the wedding arrangements.
Her parents did not approve of the marriage and boycotted the wedding. Her paternal aunt, however, agreed to come to Canada for the wedding. Since I was regarded by Antonella as part of her extended family support system, she brought her aunt to meet me. It gave me another view of Antonella’s family. Her aunt was warm and supportive of Antonella, trying to smooth over the family differences. A few months later, at Christmas time, her parents and sister visited, and Antonella brought them to meet me. To understand these family meetings, however, it is necessary to know Antonella’s early history.
2.3 A Foundling Child
Antonella was a foundling child. Abandoned on the steps of a foundry in Turin as a newborn, she was the subject of an investigation into the private medical clinics of Turin. This revealed that the staff of the clinic where she was born was ‘paid off to hide the circumstances of my birth.’ As a result, her date of birth could only be presumed because the clinic staff destroyed her birth records. She was taken into care by the state and, as her origins could not be established, she was put up for adoption.
Antonella has always tried to fill in this void of information with meaning that she draws from her own body. She questions me closely: ‘Just look at me. Don’t you think I look like a Japanese?’ She feels that her skin tone is different from other Italians, that her facial features and eyes have an ‘Asian’ cast. With a few, limited facts, and some speculation, she has constructed a personal myth: that she is the daughter of an Italian mother from a wealthy family (hence her hidden birth in a private clinic) and a Japanese father (hence her ‘Asian’ features). It is oddly reassuring to her, but also perhaps a source of her alienation from her family.
At about 6 months of age, Antonella was adopted into a family in the Italian Alps, near the border with Austria. This is a bicultural region where both Italian and German are spoken and services are available in both languages (much like Ottawa, which is bilingually English and French). Her father, Aldo, who is Italian, is a retired FIAT factory worker. Annalise, her mother, who is a homemaker, had an Italian father and an Austrian mother. About her family she said, ‘I had a wonderful childhood compared to what came afterwards.’ Years after her adoption, her parents had a natural child, Oriana, who is 15.
She describes her mother as the disciplinarian at home. Her mother, she said, was ‘tough, German.’ When she visited her Austrian grandmother, no playing was allowed in that strict home. Her own mother allowed her ‘no friends in the house,’ but her father ‘was my pal when I was a kid.’ Although she had a good relationship with her father, he became ‘colder’ when she turned 13. Her parents’ relationship is remembered as cordial, but she later learned that they had many marital problems. Mother told her that she married to get away from home, but in fact she was in love with someone else. Overall, the feeling is of a rigid family organization. Her father is clearly presented by Antonella as warmer and more sociable. She experiences her mother as being ‘tough’. But she is crying all the time, feeling betrayed by everybody.
2.4 A Family Visit from the Italian Alps
When her family finally came to visit, Antonella brought them to see me. At first, the session had the quality of a student introducing out-of-town parents to her college teacher. They were pleased that I spoke Italian and knew Dr. Angelo, who they trusted. I soon found that the Trevisans were hungry to tell their story. Instead of a social exchange of pleasantries, this meeting turned into the first session of an impromptu course of brief family therapy.
Present were Antonella’s parents, Aldo and Annalise, and her sister, Oriana. Annalise led the conversation. Relegating Aldo to a support role. Oriana alternated between disdain and agitation, punctuated by bored indifference. Annalise had much to complain about: her own troubled childhood, her sense of betrayal and abandonment, heightened by Antonella’s departure from the family and from Italy. I was struck by the parallel themes of abandonment in mother and daughter. Mother clearly needed to tell this story, so I tried to set the stage for the family to hear her, what narrative therapists call ‘recruiting an audience’ [ 9 ] . I used Antonella, who I knew best, as a barometer of the progress of the session, and by that indicator, believed it had gone well.
When I saw them again some 10 days later, I was stunned by the turn of events. Oriana had assaulted her parents. The father had bandages over his face and the mother had covered her bruises with heavy make-up and dark glasses. Annalise was very upset about Oriana, who was defiant and aggressive at home. For her part, Oriana defended herself by saying she had been provoked and hit by her mother. Worried by this dangerous escalation, I tried to open some space for a healthy standoff and renegotiation.
Somehow, the concern had shifted away from Antonella to Oriana. Antonella was off the hook, but I waited for an opening to deal with this. I first tried to explore the cultural attitudes to adolescence in Italy by asking how the Italian and the German subcultures in their area understood teenagers differently. What were Oriana’s concerns? Had they seen this outburst coming? The whole family participated in a kind of sociological overview of Italian adolescence, with me as their grateful audience. The parents demonstrated keen insight and empathy. Concerned about Oriana’s experience of the session, I made a concerted effort to draw her into it. Eventually, the tone of the session lightened. Knowing they would return to Italy soon, I explored whether they had considered family work. Since they had met a few times with Dr. Angelo over Antonella’s eating problems, they were comfortable seeing Dr. Angelo as a family to find ways to understand Oriana and her concerns and for Oriana to explore other, nonviolent ways to be heard in the family. I agreed to meet them again before their departure and to communicate with Dr. Angelo about their wishes. On their way out, I wondered aloud about the apparent switch in their focus from Antonella to Oriana. The parents reassured me that they were ready to let Antonella live her own life now.
When they returned to say goodbye, we had a brief session. Oriana and Antonella were oddly buoyant and at ease. The parents were relieved. Antonella had offered the possibility of Oriana returning to spend the summer in Canada with her. I tried to connect this back to the previous session, wondering how much the two sisters supported each other. I was delighted, I said emphatically, by the family’s apparent approval of Antonella’s marriage to Rick. It was striking that, even from a distance of thousands of miles away, Antonella was still a part of the Trevisan family. And Rick was still not in the room.
3 Discussion
In this section, I will consider the impact of cultural and other values on Antonella and those around her and then look briefly at the wider implications of her story for our understanding not only of eating disorders but of mental distress and disorders in general.
3.1 Antonella: Life Before Man
The key to understanding Antonella’s attachments was her passion for her Siberian huskies. In the language of values-based practice , it was above all her huskies that mattered or were important to her. And it is not hard to see why. From the beginning of her relationship with Rick, she used her interest in dogs as a way for them to be more socially active as a couple, getting them out of the house to go to dog shows, for example. As her interests expanded, she wanted to buy bitches for breeding and to set up a kennel. Rick was only reluctantly supportive in this. Nonetheless, they ended up buying a home in the country where she could establish a kennel. Her haggling with Rick over the dogs was quite instrumental on her part, representing her own choices and interests and a test of the extent to which Rick would support her.
Yet the importance to Antonella of her huskies rests I believe on deeper cultural factors, both negative and positive. As to negative factors , these are evident in the fact that from the first days of her life, Antonella was rejected by her birth parents, literally abandoned and exposed, and later adopted by what she experienced as a non-nurturing family. Positive cultural factors , on the other hand, are evident in the way that having thrown her net wider afield, she looked initially to Canada, and to Rick, for nurturance and for identity. Then, finding herself only partly satisfied, she turned to the nonhuman world for the constancy of affection she could not find with people. Her huskies gave her pleasure, a task, and an identity. She spent many sessions discussing their progress, showing me pictures of her dogs and their awards. As it happened, my secretary at the time was also a dog lover who raised Samoyed dogs (related to huskies) and the two of them exchanged stories of dog lore.
As to positive factors , again, is there something, too, in the mythology of Canada that helps us understand Antonella? Does Canada still hold a place in the European imagination as a ‘New World’ for radical departures and identity makeovers? Or does Canada specifically represent the ‘malevolent North,’ as Margaret Atwood [ 10 ] calls it in her exploration of Canadian fiction? Huskies are a Northern animal, close to the wolf in their origins and habits. Bypassing the human world, Antonella finds her identity within a new world through its animals. If people have failed her, then she will leave not only her own tribe (Italy), but skip the identification with Canada’s Native peoples, responding to the ‘call of the wild’ to identify with a ‘life before man’ (to use another of Atwood’s evocative phrases, [ 11 ]), finding companionship and solace with her dogs.
3.2 Wider Implications of Antonella’s Story
Antonella may seem on first inspection something of an outlier to the human tribe. Orphaned from her culture of origin, she finds her place not in another country but by identification with another and altogether wilder species, her husky dogs. Yet, understood through the lens of values-based practice Antonella’s story has, I believe, wider significance at a number of levels.
First, Antonella’s story is significant for our understanding of the role of values – of what is important or matters to the individual concerned – in the presentation and treatment of eating disorders , and, by extension, of perhaps many other forms of mental distress and disorder. Specifically, her story provides at least one clear ‘proof of principle’ example supporting the role of cultural values.
As noted in my introduction, much attention has been given in the literature to the correlations between the uneven geographical distribution of eating disorders and cultural values. Correlations are of course no proof of causation. But in Antonella’s story at least the role of cultural values seems clearly evident. They were key to understanding her presenting problems. And this understanding in turn proved to be key to the cultural family therapy [ 12 ] through which these problems were, at least to the extent of her presenting eating disorder, resolved.
The cultural values involved, it is true, were not those of fashionable slimness so widely discussed in the literature. But this takes us to a second level at which Antonella’s story has wider significance. For it shows that to the extent that cultural values are important in eating disorders , their importance plays out at the level of individually unique persons. In this sense, social stresses and cultural values are played out in the body of the individual suffering with an eating disorder, making her body the ‘final frontier’ of psychiatric phenomenology [ 13 ]. Yes, there are no doubt valid cultural generalisations to be made about eating disorders and mental disorders of other kinds. And yes, these generalisations no doubt include generalisations about cultural values—about things that matter or are important to this or that group of people as a whole. Yet, this does not mean that we can ignore the values of the particular individual concerned. It has been truly said in values-based practice that as to their values, everyone is an ‘ n of 1’ [ 14 ]. Antonella, then, in the very idiosyncrasies of her story, reminds us of the idiosyncrasies of the stories of each and every one of us, whatever the culture or cultures to which we belong.
Antonella’s identification with animals , furthermore, to come to yet another level at which her story has wider significance, was a strongly positive factor in her recovery. As with other areas of mental health, it is with the negative impact of cultural values that the literature has been largely concerned: the pathogenetic influences of cultural values of slimness being a case in point in respect of eating disorders . Antonella’s story illustrates what has been clear for some time in the ‘recovery movement’, that positive values are often the very key to recovery. Not only that, but as Antonella’s passion for her husky dogs illustrates, the particular positive values concerned may, and importantly often are, individually unique.
Not, it is worth adding finally, that Antonella’s values were in this respect entirely unprecedented. Animals , after all, are widely valued, positively and negatively, and for many different reasons, in many cultures [ 11 ]. Their healing powers are indeed acknowledged. Just how far these powers depend on the kind of cross-species identification shown by Antonella, remains a matter for speculation. But, again, her story even in this respect is far from unique. Elsewhere, I have described the story of a white boy with what has become known as the ‘Grey Owl Syndrome’ , wishing to be native [ 12 , chapter 5 ]. Similarly, in Bear , Canadian novelist Marion Engel [ 15 ] portrays Lou, a woman who lives in the wilderness and befriends a bear. Lou seeks her identity from him: ‘Bear, make me comfortable in the world at last. Give me your skin’ [ 15 , p. 106]. After some time with the bear, the woman changes: ‘What had passed to her from him she did not know…. She felt not that she was at last human, but that she was at last clean’ [ 15 , p. 137]. It was perhaps to some similarly partial resolution that Antonella came.
4 Conclusions
Antonella’s story as set out above goes to the heart of the importance of cultural values in mental health. Her presenting eating disorder develops when, displaced from her culture of origin in Italy, and in effect rejected by her birth family, she finds healing only through cross-species identification with the wildness of husky dogs in her adoptive country of Canada. Although somewhat unusual in its specifics, her story illustrates the importance of cultural values at a number of levels in the presentation and management of eating and other forms of mental distress disorder.
And Antonella? I met her again in a gallery in Ottawa, rummaging through old prints. She was asking about prints of dogs; I was looking for old prints of Brazil where my father had made a second life. How was she, I asked? ‘Well …,’ she said hesitantly. Was that a healthy ‘well’ or the start of an explanation? ‘Me and Rick are splitting up,’ she said without ceremony, ‘but I still have the huskies.’ For each of us, the prints represented another world of connections.
Makino M, Tsuboi K, Denerson L. Prevalence of eating disorders: a comparison of Western and non-Western countries. MedGenMed. 2004;6(3):49. Published online 2004 Sep 27 at: https://www.ncbi.nlm.nih.gov/pubmed .
PubMed PubMed Central Google Scholar
Erskine HE, Whiteford HA, Pike KM. The global burden of eating disorders. Curr Opin Psychiatry. 2016;29(6):346–53.
Article Google Scholar
Selvini Palazzoli M. Anorexia nervosa: a syndrome of the affluent society. Transcult Psychiatr Res Rev. 1985;22( 3 ):199–205.
Google Scholar
Di Nicola VF. Overview: anorexia multiforme: self-starvation in historical and cultural context. I: self-starvation as a historical chameleon. Transcult Psychiatr Res Rev. 1990;27(3):165–96.
Di Nicola VF. Overview: anorexia multiforme: self-starvation in historical and cultural context. II: anorexia nervosa as a culture-reactive syndrome. Transcult Psychiatr Res Rev. 1990;27(4):245–86.
Andolfi M, Angelo C, de Nichilo M. The myth of atlas: families and the therapeutic story. Edited & translated by Di Nicola VF. New York: Brunner-Routledge; 1989.
Douglas M. Humans speak. Ch 11. In: Implicit meanings: essays in anthropology. London: Routledge & Kegan Paul; 1975. p. 173–80.
Crystal D. The Cambridge encyclopedia of language. Cambridge: Cambridge University Press; 1987.
Parry A, Doan RE. Story re-visions: narrative therapy in the postmodern world. New York: Guilford Press; 1995.
Atwood M. Strange things: the malevolent north in Canadian literature. Oxford: Oxford University Press; 1995.
Atwood M. Life before man: a novel. New York: Anchor Books; 1998.
Di Nicola VF. A stranger in the family: culture, families, and therapy. New York: W.W. Norton & Co.; 1997.
Nasser M, Di Nicola V. Changing bodies, changing cultures: an intercultural dialogue on the body as the final frontier. Ch 9. In: Nasser M, Katzman MA, Gordon RA, editors. Eating disorders and cultures in transition. East Sussex: Brunner-Routledge; 2001. p. 171–93.
Fulford KWM, Peile E, Carroll H. A smoking enigma: getting and not getting the knowledge. Ch 6. In: Fulford KWM, Peile E, Carroll H, editors. Essential values-based practice: clinical stories linking science with people. Cambridge: Cambridge University Press; 2012. p. 65–82.
Chapter Google Scholar
Engel M. Bear: a novel. Toronto: Emblem (Penguin Random House Books); 2009.
Download references
Acknowledgements
The story of Antonella was first published in reference [ 12 ] (pp. 214–220) and presented at the Advanced Studies Seminar of the Collaborating Centre for Values-based Practice in Health and Social Care at St Catherine’s College, Oxford in October 2019. The names and other details of the case have been altered to maintain confidentiality. Parts of the discussion are adapted from that publication and the Oxford seminar. I am grateful to the publishers for permission to reproduce these materials here and to Professor Fulford and the members of the Advanced Studies Seminar for their stimulating exchanges. The subheading to the discussion of Antonella’s story (‘Life before Man’) was inspired by Margaret Atwood’s novel, Life Before Man [ 11 ].
Author information
Authors and affiliations.
Canadian Association of Social Psychiatry (CASP), World Association of Social Psychiatry (WASP), Department of Psychiatry and Addictions, University of Montreal, Montreal, QC, Canada
Vincenzo Di Nicola
Department of Psychiatry and Behavioral Sciences, The George Washington University, Washington, DC, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Vincenzo Di Nicola .
Editor information
Editors and affiliations.
Medical University Plovdiv, Plovdiv, Bulgaria
Drozdstoy Stoyanov
St Catherine’s College, University of Oxford, Oxford, UK
Bill Fulford
Department of Psychological, Health & Territorial Sciences, “G. D’Annunzio” University, Chieti Scalo, Italy
Giovanni Stanghellini
Centre for Ethics and Philosophy of Health Sciences, University of Pretoria, Pretoria, South Africa
Werdie Van Staden
Department of Psychiatry, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China
Michael TH Wong
Guide to Further Sources
For a more extended treatment of the role of culture in eating disorders and family therapy see:
Di Nicola VF (1990a) Overview: Anorexia multiforme: Self-starvation in historical and cultural context. I: Self-starvation as a historical chameleon. Transcultural Psychiatric Research Review, 27(3): 165–196.
Di Nicola VF (1990b) Overview: Anorexia multiforme: Self-starvation in historical and cultural context. II: Anorexia nervosa as a culture-reactive syndrome. Transcultural Psychiatric Research Review, 27(4): 245–286.
Di Nicola, V (1997) A Stranger in the Family: Culture, Families, and Therapy . New York & London: W.W. Norton & Co.
Nasser M and Di Nicola, V. (2001) Changing bodies, changing cultures: An intercultural dialogue on the body as the final frontier. In: Nasser M, Katzman M A, and Gordon R A, eds. Eating Disorders and Cultures in Transition . East Sussex, UK: Brunner-Routledge, pp. 171–193.
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions
Copyright information
© 2021 The Author(s)
About this chapter
Di Nicola, V. (2021). Antonella: ‘A Stranger in the Family’—A Case Study of Eating Disorders Across Cultures. In: Stoyanov, D., Fulford, B., Stanghellini, G., Van Staden, W., Wong, M.T. (eds) International Perspectives in Values-Based Mental Health Practice. Springer, Cham. https://doi.org/10.1007/978-3-030-47852-0_3
Download citation
DOI : https://doi.org/10.1007/978-3-030-47852-0_3
Published : 12 December 2020
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-47851-3
Online ISBN : 978-3-030-47852-0
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Eating disorders in adolescent boys and young men: an update
Jason m nagata, kyle t ganson, stuart b murray.
- Author information
- Copyright and License information
Corresponding Author: Jason M. Nagata, 550 16 th Street, 4 th Floor, Box 0110, San Francisco, California 94158, Telephone: +1 (626) 551-1932, [email protected]
Purpose of review
To review the recent literature on eating disorders and disordered eating behaviors among adolescent boys and young men, including epidemiology, assessment, medical complications, treatment outcomes, and special populations.
Recent findings
Body image concerns in males may involve muscularity, and muscle-enhancing goals and behaviors are common among adolescent boys and young men. Recent measures, such as the Muscularity Oriented Eating Test (MOET), have been developed and validated to assess for muscularity-oriented disordered eating. Medical complications of eating disorders can affect all organ systems in males. Eating disorder treatment guidance may lack specificity to males, leading to worse treatment outcomes in this population. Male populations that may have elevated risk of eating disorders and disordered eating behaviors include athletes and racial/ethnic, sexual, and gender minorities.
Eating disorders and disordered eating behaviors in males may present differently than in females, particularly with muscularity-oriented disordered eating. Treatment of eating disorders in males may be adapted to address unique concerns in males.
Keywords: Eating disorders, anorexia nervosa, muscle dysmorphic disorder, boys, male health
INTRODUCTION
Eating disorders (ED) are thought to be among the most gendered of mental health disorders [ 1 ], with strong associations with femininity. Eating disorder diagnoses include, but are not limited to, anorexia nervosa (AN), atypical anorexia nervosa (AAN), bulimia nervosa (BN), binge eating disorder (BED), and avoidant/restrictive food intake disorder (ARFID) according to the Diagnostic and Statistical Manual of Mental Disorders, 5 th Edition (DSM-5) [ 2 ]. Despite decades of research focusing exclusively on female populations, unique body image and disordered eating concerns are increasingly recognized in male populations. Males may have a higher drive for muscularity [ 3 ] which may, in extreme cases, lead to muscle dysmorphic disorder [ 4 ].
The purpose of this article is to review recent literature on eating disorders and disordered eating behaviors among male populations, with special consideration related to adolescent boys and young men. In particular, we review the epidemiology, assessment, medical complications, treatment, and special populations related to male eating disorders.
Epidemiology
Although there has traditionally been a paucity of research on male body image and disordered eating behaviors in community settings [ 5 ], some recent literature has shed light on the epidemiology of these phenomena. A study of Australian adolescents estimated the prevalence rates of DSM-5 eating disorder diagnoses by gender. Among adolescent boys, 12.8% met criteria for any eating disorder diagnosis, including other specified feeding and eating disorder (OSFED, 8.5%), night eating syndrome (4.9%), bulimia nervosa (1.8%), unspecified feeding and eating disorder (UFED, 1.3%), and atypical anorexia nervosa (1.2%) [6]** . Nationally representative surveys in the USA demonstrate that 30% of adolescent boys report trying to gain weight or bulk up, including 40% of boys objectively considered normal weight by body mass index (BMI) [ 7 ]. Nearly 22% of young men report engaging in muscle-enhancing behaviors, including eating more or differently to build muscle (17%), supplement use (7%), and androgenic-anabolic steroid use (3%) [ 8 ]. Among young men, overweight and obesity may be associated with disordered eating behaviors. Overall, 15% of young men with BMI ≥ 25 report engaging in disordered eating behaviors including fasting, skipping meals, vomiting, laxatives, diuretics, or binge-eating [ 9 ]. In comparison, 8% of young men with BMI < 25 report engaging in disordered eating behaviors.
A recent review article provides an overview of assessment measures for men with eating disorders, including body image measures, muscularity-oriented measures, and eating disorder measures [ 4 ]. Examples of assessment tools that can be used in male populations include the Eating Disorders Examination Questionnaire (EDE-Q) and Muscle Dysmorphic Disorder Inventory (MDDI) [ 4 ]. Given the diversity of populations affected by eating disorders, the EDE-Q [ 10 ] and MDDI [ 11 ] have been translated and validated in Spanish for Latin American male populations.
While the under-recognition of EDs among males has been well documented [ 12 ], recent years have seen some important advances. Existing assessment instruments are insensitive towards disordered eating that is oriented towards the pursuit of muscularity. Indeed, with the hyper-muscular body ideals being pervasively portrayed to males, disordered eating symptoms are increasingly muscularity-centric. To this end, the recent development of the muscularity-oriented eating test (MOET) offers important new insights on the measurement of disordered eating attitudes and behaviors that are intended to increase muscular density or leanness [13]* . The MOET is a 15-item measure which dually captures behaviors related to the development of muscularity and the reduction of body adiposity - which enhances the visibility of muscularity ( Table 1 ).
Table 1. The Muscularity Oriented Eating Test (MOET).
Instructions: Please read each statement carefully and circle the number that best indicates how true each statement is of you. Please answer all the questions as honestly as you can, as they apply to you in the last 4 weeks. (0 = never true, 1 = rarely true, 2 = sometimes true, 3 = usually true, 4 = always true)
Global MOET scores are formed by calculating the mean score of all items. Murray SB, Brown TA, Blashill AJ, et al. The development and validation of the muscularity-oriented eating test: A novel measure of muscularity-oriented disordered eating. Int J Eat Disord 2019, 52:1389–1398.
Medical Complications
Medical complications of eating disorders, particularly related to malnutrition, can affect every organ system in the body [ 14 ]. In one clinical sample of adolescent boys with EDs, over half (52%) had vital sign instability that met Society for Adolescent Health and Medicine hospital admission criteria [ 15 ]. Bradycardia was present in 39% and orthostatic heart rate changes were present in 12% of the sample. Bradycardia requiring hospital admission criteria has also been reported among adolescent boys with muscularity-oriented disordered eating [ 16 ], and hours of exercise per week is associated with bradycardia among adolescents with eating disorders [ 17 ]. Forty percent of adolescent boys with eating disorders had abnormal total cholesterol levels [ 15 ], and binge eating has been shown to be associated with hyperlipidemia in young men [ 18 ].
Electrolyte abnormalities are common in adolescent boys with eating disorders; one fourth had low potassium, 5% had low phosphorus, and 10% had low calcium [ 15 ]. In terms of hematologic abnormalities, one third were anemic, 24% leukopenic, 19% thrombocytopenic, and 10% neutropenic [ 15 ]. Gastrointestinal complications in males with eating disorders include elevated liver enzymes [ 19 ], impaired gastric emptying [ 20 ], and superior mesenteric artery syndrome [ 21 ].
Skeletal and bone complications have been documented in males with eating disorders. Significant deficits in bone mineral density [ 22 ], lean mass, and fat mass index [ 23 ] have been documented in adolescent boys with anorexia nervosa. Adolescent samples including boys have demonstrated that bone mineral density is higher in atypical anorexia nervosa versus anorexia nervosa [ 24 ], and that weight bearing exercise and participation in team sports may be protective of bone mineral density at the hip and whole body bone mineral content [ 25 ]. In adult men, low bone mineral density Z scores (<−2 at ≥1 site) have been documented in men with anorexia nervosa (65%), atypical anorexia nervosa, (33%), and ARFID (18%) [ 26 ]. Men with anorexia nervosa over age 40 have greater fracture risk compared to healthy controls over age 40 [ 27 ].
Medical guidelines specific to male populations are lacking, and are mostly based on research and clinical experience with females [ 28 ]. Some clinical guidance still use criterion, such as amenorrhea, which are not applicable to males [ 28 ]. For instance, the Society for Adolescent Health and Medicine medical update for restrictive eating disorders indicates that dual-energy X-ray absorptiometry (DXA) scans should be conducted to monitor bone health when there has been a loss of menses for six or more months [ 29 ]. While this does not provide specific guidance on how to monitor bone health among adolescent boys, clinical practice guidelines produced by the National Institute for Health and Care Excellence [ 30 ] and the Royal Australian and New Zealand College of Psychiatrists [ 31 ] indicate that duration of illness may be a more effective measure of when to obtain a DXA scan. Additional areas where clinical guidance is lacking for adolescent boys and young men include using BMI and weight loss as a measure of malnutrition and severity of illness, refeeding protocols, and the assessment and treatment of performance-enhancing substances (PES) use [ 28 ].
In documenting treatment outcomes among males with EDs, few randomized controlled trials exist. In fact, most randomized controlled trials have actively excluded male patients on the basis of their purported atypicality [ 12 ]. Qualitative research demonstrates that men with eating disorders report feeling like “the odd one out” or “atypical’ in current female-dominated treatment environments [ 32 ]. Recently, however, a large dataset documenting clinical outcomes among a transdiagnostic sample of 110 males was reported. These data suggest comparable remission rates among males and females with anorexia nervosa by the end of treatment (at approximately 40% remission [ 33 ]), although more males demonstrated clinically significant disordered eating at follow-up. Males with bulimia nervosa demonstrated marginally less favorable remission relative to females with bulimia nervosa (44% remission by end of treatment, versus 50%). Importantly, however, standardized mortality rates were higher in males with anorexia nervosa relative to both females with anorexia nervosa, and males with bulimia nervosa [ 34 ], suggesting that anorexia nervosa in males may be particularly pernicious. In another study, men with eating disorders at 12-month follow-up had partial recovery (19%) or full recovery (14%) [ 35 ].
Special Populations
There are several unique populations that are important to highlight when considering eating disorders among adolescent boys and young men. First, recent research has begun to identify the unique disordered eating and weight gain behaviors that are prevalent among adolescent boys and young men, particularly athletes. Weight gain behaviors among adolescent and young adult males may be driven by body ideals that emphasize muscularity and leanness [ 36 ]. Among collegiate male athletes, baseball, cycling, and wrestling were sports with the most players reporting elevated eating disorder symptoms in a clinical range [ 37 ]. Among competitive collegiate male athletes, nearly half report current supplement use [ 38 ]. Sports supplement use in male athletes is associated with greater eating disorder symptoms [ 38 ]. Use of legal performance-enhancing supplements is associated with future use of anabolic-androgenic steroids [ 39 ]. Little is known about long-term health consequences of performance-enhancing supplements, as the Food and Drug Administration do not review dietary supplements for effectiveness or safety [ 40 ]. Adolescent boys may be more likely to engage in individually driven exercise compared to females. This may be exacerbated by athletic norms associated with sports that emphasize muscularity and strength (i.e. American football) or weight control and loss (i.e. wrestling) [ 17 , 36 ].
A second area of importance to highlight is EDs among racially and ethnically diverse adolescent boys. This area of knowledge remains largely sparse, as there is a dearth of research solely investigating specific racial/ethnic adolescent populations and eating disorders. This is in part due to continued sociocultural narratives that EDs primarily impact White, affluent, adolescent females. Thus, there remains an urgent need to conduct robust and rigorous research on the unique differences among adolescent males with EDs across racial/ethnic identities. However, current research indicates that disordered eating behaviors may be particularly prevalent among non-White adolescent boys. One study among a population of adolescents from Minnesota found that disordered eating behaviors were highest among Asian boys (43%), followed by Black boys (38.5%), Hispanic boys (35%), and lastly, White boys (33%) [ 41 ]. Using the National Youth Risk Behavior Surveillance Survey (YRBS), another recent study found that Black/African American and Hispanic/Latino boys had higher prevalence rates and risk ratios of purging behaviors and fasting behaviors compared to White boys [42]** . This study also found that Hispanic/Latino boys had higher, while Black/African American boys had nearly identical, prevalence rates and risk ratios of diet pill use compared to their White peers [ 42 ]. Given the results from these studies, it is evident that additional research is needed to develop a stronger understanding of the nuances of EDs among racially and ethnically diverse male populations.
EDs have been documented among sexual minority males. In general, research has continued to indicate that sexual minority adolescent boys experience body dissatisfaction, EDs, and disordered weight control behaviors [ 43 ]. Research from the United Kingdom has found that gay or bisexual, as well as mostly heterosexual, boys had significantly greater odds of dieting behaviors compared to their completely heterosexual peers [44]* . Similarly, body dissatisfaction and pressure to increase muscularity was highest among mostly heterosexual and gay or bisexual boys [ 44 ]. Lastly, gay and bisexual boys and mostly heterosexual boys had the greatest odds of any binge-eating behaviors compared to their completely heterosexual peers [ 44 ]. Similarly, among a national sample of adolescent boys in the United States, boys who identify as gay, bisexual, or not sure had greater odds of reporting fasting behaviors. Further, adolescent boys who identify as bisexual or not sure of their sexual orientation had greater odds of using steroids compared to their heterosexual peers [ 45 ]. More specific results from the state of Connecticut [ 46 ] and Massachusetts [ 47 ] found that sexual minority adolescent boys had greater odds of ED and weight control behaviors compared to their heterosexual peers. In terms of adult men, eating disorder attitudes and behaviors have been shown to be elevated among gay men compared to the general population of men [ 48 ]. Despite this evidence, there remains a paucity of research on the epidemiology, treatment, and prevention of EDs among sexual minority adolescent boys and young men.
A final area of importance to highlight is the intersection of gender with EDs. Masculine gender norms are associated with muscle-enhancing behaviors [ 49 ]. Transgender men may therefore desire a masculine-appearing build and engage in muscle-enhancing behaviors such as bodybuilding [ 50 ]. Transgender men may experience dissatisfaction with several body features such as genitalia, body hair, body shape, facial features, and extremities [ 51 ]. Young adult transgender men have also been shown to report high rates of binge eating (35%), fasting (34%), and vomiting (7%) [ 52 ]. A review article has previously summarized body image and eating disorders in sexual and gender minority youth [ 53 ].
Emerging research demonstrates that males with eating disorders have unique concerns with regards to disordered eating and body image. Clinical guidance for eating disorders has not yet become individualized to address these unique concerns [ 28 ], and future research should develop male-specific screening, treatment guidance, and interventions to improve health outcomes in this underserved population.
Key Points.
Body image concerns in males may involve muscularity; muscle-enhancing goals and behaviors are common among adolescent boys and young men.
Recent measures, such as the Muscularity Oriented Eating Test (MOET), have been developed and validated to assess for muscularity-oriented disordered eating.
Medical complications of eating disorders can affect all organ systems in males and there are inadequate medical management guidelines for adolescent boys and young men.
Male populations that may have elevated risk of eating disorders and disordered eating behaviors include athletes and racial/ethnic, sexual, and gender minorities.
Financial support and sponsorship
J.M.N. was a participant in the Pediatric Scientist Development Program (K12HD00085033), funded by the American Academy of Pediatrics and the American Pediatric Society, and a recipient of the American Heart Association Career Development Award (CDA34760281). S.B.M. was supported by the National Institutes of Health (K23 MH115184).
Conflicts of interest
The authors have no conflicts of interest to declare
- 1. Weber AM, Cislaghi B, Meausoone V, et al. How gender norms shape health: insights from global survey data. Lancet 2019, 393:2455–2468. [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th Ed. edition Arlington, VA: American Psychiatric Publishing; 2013. [ Google Scholar ]
- 3. Eik-Nes TT, Austin SB, Blashill AJ, et al. Prospective health associations of drive for muscularity in young adult males. Int J Eat Disord 2018, 51:1185–1193. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Lavender JM, Brown TA, Murray SB. Men, Muscles, and Eating Disorders: an Overview of Traditional and Muscularity-Oriented Disordered Eating. Curr Psychiatry Rep 2017, 19:32. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Murry SB, Griffiths S, Nagata JM. Community-Based Eating Disorder Research in Males: A Call to Action. J Adolesc Health 2018, 62:649–50. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6.**. Mitchison D, Mond J, Bussey K, et al. DSM-5 full syndrome, other specified, and unspecified eating disorders in Australian adolescents: prevalence and clinical significance. Psychol Med 2019:1–10. [ DOI ] [ PubMed ] [ Google Scholar ]; Reports on prevalence of DSM-5 eating disorders in adolescent boys in Australia
- 7. Nagata JM, Bibbins-Domingo K, Garber AK, et al. Boys, Bulk, and Body Ideals: Sex Differences in Weight Gain Attempts Among Adolescents in the United States. J Adolesc Health 2019, 64:450–453. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Nagata JM, Murray SB, Bibbins-Domingo K, et al. Predictors of muscularity-oriented disordered eating in US young adults: a prospective cohort study. Int J Eat Disord 2019, 52:1380–1388. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Nagata JM, Garber AK, Tabler J, et al. Prevalence and Correlates of Disordered Eating Behaviors among Young Adults with Overweight or Obesity. J Gen Intern Med 2018, 33:1337–1343. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Compte EJ, Nagata JM, Sepúlveda AR, et al. Confirmatory factor analysis and measurement invariance of the eating disorders examination-questionnaire across four male samples in Argentina. Int J Eat Disord 2019, 52:740–745. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Compte EJ, Nagata JM, Sepúlveda AR, et al. Assessment and validation of a Spanish version of the Muscle Dysmorphia Disorder Inventory in Argentinian men who exercise: Inventario de Dismorfia Muscular. Body Image 2019, 31:24–34. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Murray SB, Nagata JM, Griffiths S, et al. The enigma of male eating disorders: A critical review and synthesis. Clin Psychol Rev 2017, 57:1–11. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13.*. Murray SB, Brown TA, Blashill AJ, et al. The development and validation of the muscularity-oriented eating test: A novel measure of muscularity-oriented disordered eating. Int J Eat Disord 2019, 52:1389–1398. [ DOI ] [ PubMed ] [ Google Scholar ]; New measure validated measure for muscularity-oriented disordered eating
- 14. Chidiac CW. An update on the medical consequences of anorexia nervosa. Curr Opin Pediatr 2019, 31:448–453. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Vo M, Lau J, Rubinstein M. Eating Disorders in Adolescent and Young Adult Males: Presenting Characteristics. J Adolesc Health 2016, 59:397–400. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Murray SB, Accurso EC, Griffiths S, et al. Boys, Biceps, and Bradycardia: The Hidden Dangers of Muscularity-Oriented Disordered Eating. J Adolesc Health 2018, 62:352–355. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Nagata JM, Carlson JL, Kao JM, et al. Characterization and correlates of exercise among adolescents with anorexia nervosa and bulimia nervosa. Int J Eat Disord 2017, 50:1394–1403. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 18. Nagata JM, Garber AK, Tabler J, et al. Disordered Eating Behaviors and Future Cardiometabolic Risk among Young Adults with Overweight or Obesity. Int J Eat Disord 2018, 51:931–941. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Nagata JM, Park KT, Colditz K, et al. Associations of elevated liver enzymes among hospitalized adolescents with anorexia nervosa. J Pediatr 2015, 166:439–43.e1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Nagata JM, Golden NH. Sex differences in eating disorders. Adolesc Med State Art Rev 2018, 29:245–259. [ Google Scholar ]
- 21. Recio-Barbero M, Fuertes-Soriano S, Cabezas-Garduño J, et al. Delayed Diagnosis of an Eating Disorder in a Male Patient With Superior Mesenteric Artery Syndrome: Results From a Case Study. Front Psychiatry 2019, 10:731. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Nagata JM, Golden NH, Peebles R, et al. Assessment of sex differences in bone deficits among adolescents with anorexia nervosa. Int J Eat Disord 2017, 50:352–58. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Nagata JM, Golden NH, Peebles R, et al. Assessment of Sex Differences in Body Composition Among Adolescents With Anorexia Nervosa. J Adolesc Health 2017, 60:455–459. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Nagata JM, Carlson JL, Golden NH, et al. Comparisons of bone density and body composition among adolescents with anorexia nervosa and atypical anorexia nervosa. Int J Eat Disord 2019, 52:591–596. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Nagata JM, Carlson JL, Golden NH, et al. Associations between exercise, body composition, and bone mineral density in adolescents with anorexia nervosa. Eat Weight Disord 2019, 24:939–945. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Schorr M, Drabkin A, Rothman MS, et al. Bone mineral density and estimated hip strength in men with anorexia nervosa, atypical anorexia nervosa and avoidant/restrictive food intake disorder. Clin Endocrinol (Oxf) 2019, 90:789–797. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 27. Nagata JM, Golden NH, Leonard MB, et al. Assessment of Sex Differences in Fracture Risk Among Patients With Anorexia Nervosa: A Population-Based Cohort Study Using The Health Improvement Network. J Bone Miner Res 2017, 32:1082–1089. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Ganson KT, Murray SB, Nagata JM. Last word: A call to develop specific medical treatment guidelines for adolescent males with eating disorders. Eat Disord 2019:1–7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Golden NH, Katzman DK, Sawyer SM, et al. Update on the medical management of eating disorders in adolescents. J Adolesc Health 2015, 56:370–375. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. National Institute for Health and Care Excellence. Eating disorders: recognition and treatment.; 2017. [ PubMed ]
- 31. Hay P, Chinn D, Forbes D, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders. Aust N Z J Psychiatry 2014, 48:977–1008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Kinnaird E, Norton C, Pimblett C, et al. “There’s nothing there for guys”. Do men with eating disorders want treatment adaptations? A qualitative study. Eat Weight Disord 2019, 24:845–852. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 33.*. Strobel C, Quadflieg N, Naab S, et al. Long-term outcomes in treated males with anorexia nervosa and bulimia nervosa-A prospective, gender-matched study. Int J Eat Disord 2019, 52:1353–1364. [ DOI ] [ PubMed ] [ Google Scholar ]; Reports on long-term outcomes of anorexia nervosa and bulimia nervosa in males
- 34. Quadflieg N, Strobel C, Naab S, et al. Mortality in males treated for an eating disorder-A large prospective study. Int J Eat Disord 2019, 52:1365–1369. [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Bardone-Cone AM, Johnson S, Raney TJ, et al. Eating disorder recovery in men: A pilot study. Int J Eat Disord 2019, 52:1370–1379. [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Nagata JM, Brown TA, Lavender JM, et al. Emerging trends in eating disorders among adolescent boys: muscles, macronutrients, and biohacking. Lancet Child Adolesc Health 2019, 3:444–445. [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Gorrell S, Nagata JM, Hill KB, et al. Eating behavior and reasons for exercise among competitive collegiate male athletes. Eat Weight Disord 2019. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 38. Nagata JM, Peebles R, Bell Hill K, et al. Associations Between Supplement Use and Eating Behaviors among University Students. Eat Disord 2020. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 39. Nagata JM, Ganson KT, Gorrell S, et al. Use of Legal Performance-Enhancing Substances is Prospectively Associated with Anabolic-Androgenic Steroid Use in Young Adults: A Cohort Study. JAMA Pediatr 2020. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 40. Ganson KT, Murray SB, Nagata JM. A call for public policy and research to reduce use of appearance and performance enhancing drugs and substances among adolescents. Lancet Child Adolesc Health 2020, 4:13–14. [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Rodgers RF, Watts AW, Austin SB, et al. Disordered eating in ethnic minority adolescents with overweight. Int J Eat Disord 2017, 50:665–671. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42.**. Beccia AL, Baek J, Jesdale WM, et al. Risk of disordered eating at the intersection of gender and racial/ethnic identity among U.S. high school students. Eat Behav 2019, 34:101299. [ DOI ] [ PubMed ] [ Google Scholar ]; Reports on racial/ethnic differences of disordered eating in US adolescents.
- 43. Goldhammer HB, Maston ED, Keuroghlian AS. Addressing Eating Disorders and Body Dissatisfaction in Sexual and Gender Minority Youth. Am J Prev Med 2019, 56:318–322. [ DOI ] [ PubMed ] [ Google Scholar ]
- 44.*. Calzo JP, Austin SB, Micali N. Sexual orientation disparities in eating disorder symptoms among adolescent boys and girls in the UK. Eur Child Adolesc Psychiatry 2018, 27:1483–1490. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]; Identifies sexual orientation disparities in eating disorder symptoms in adolescent boys in the UK.
- 45. Calzo JP, Turner BC, Marro R, et al. Alcohol Use and Disordered Eating in a US Sample of Heterosexual and Sexual Minority Adolescents. J Am Acad Child Adolesc Psychiatry 2019, 58:200–210. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 46. Zullig KJ, Matthews-Ewald MR, Valois RF. Relationship between disordered eating and self-identified sexual minority youth in a sample of public high school adolescents. Eat Weight Disord 2019, 24:565–573. [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Watson RJ, Adjei J, Saewyc E, et al. Trends and disparities in disordered eating among heterosexual and sexual minority adolescents. Int J Eat Disord 2017, 50:22–31. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48. Nagata JM, Capriotti MR, Murray SB, et al. Community norms for the Eating Disorder Examination Questionnaire among cisgender gay men. Eur Eat Disord Rev 2020, 28:92–101. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 49. Nagata JM, Domingue BW, Darmstadt GL, et al. Gender Norms and Weight Control Behaviors in U.S. Adolescents: A Prospective Cohort Study (1994–2002). J Adolesc Health 2020, 66:S34–S41. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 50. Farber R ‘Transing’ fitness and remapping transgender male masculinity in online message boards. Journal of Gender Studies 2017, 26:254–268. [ Google Scholar ]
- 51. Becker I, Nieder TO, Cerwenka S, et al. Body Image in Young Gender Dysphoric Adults: A European Multi-Center Study. Arch Sex Behav 2016, 45:559–574. [ DOI ] [ PubMed ] [ Google Scholar ]
- 52. Watson RJ, Veale JF, Saewyc EM. Disordered eating behaviors among transgender youth: Probability profiles from risk and protective factors. Int J Eat Disord 2017, 50:515–522. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 53. McClain Z, Peebles R. Body Image and Eating Disorders Among Lesbian, Gay, Bisexual, and Transgender Youth. Pediatr Clin North Am 2016, 63:1079–1090. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (64.7 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Search by category
Popular searches, eating disorder case study, discover another eating disorder recovery story, "eating disorders tend to hide and they don't want to be seen, and if somebody else can see it ... it's a lot harder to hide", contact us to make an enquiry or for more information.
A Tale of Two Runners: A Case Report of Athletes' Experiences with Eating Disorders in College
- PMID: 28010854
- DOI: 10.1016/j.jand.2016.09.032
Athletes are at higher risk than the general population for eating disorders, and risk is heightened for athletes in thin-build sports, including track. Collegiate athletes are particularly vulnerable to disordered eating when the transition from home to the college environment adds to the stress of performance pressures and the high demands of the sport environment. Male and female athletes who develop eating disorders share some common characteristics, yet their experiences can be quite different, in part as a consequence of their sex and how eating disorders develop, and are recognized, acknowledged, and treated, within the culture of sports. This case report describes the experiences of two track athletes, one male and one female, who were recruited to the same Division 1 collegiate track program. Both were elite athletes, freshmen in the same year, experiencing the same urban college environment, and experiencing an eating disorder characterized by restrictive eating, significant weight loss, injury, and compromised performance in sport. Both received treatment from a multidisciplinary team of professionals. Both athletes achieved weight restoration, recovery from the disorder, and success in their sport. In spite of the similarities, striking differences were apparent in clinical presentation, predisposing features, onset of symptoms, entry points to treatment, interventions received, and clinical courses through treatment that depict sex differences in how eating disorders present in athletes and are addressed in the sport environment. Findings endorse the need for research and inform prevention strategies, risk assessment, and intervention approaches for nutrition and sports medicine professionals and collegiate athletic departments.
Keywords: Anorexia nervosa; Case report; Eating disorder, not otherwise specified (EDNOS); Eating disorders; Sports nutrition.
Copyright © 2017 Academy of Nutrition and Dietetics. Published by Elsevier Inc. All rights reserved.

Publication types
- Case Reports
- Athletic Performance*
- Body Mass Index
- Body Weight
- Feeding and Eating Disorders / diagnosis*
- Feeding and Eating Disorders / diet therapy*
- Nutrition Assessment
- Nutritionists
- Risk Factors
- Sports Medicine
- Sports Nutritional Physiological Phenomena
- Universities
- Young Adult
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Family-Based Treatment of a 17-Year-Old Twin Presenting with Emerging Anorexia Nervosa: A Case Study Using the “Maudsley Method”
Katharine l loeb, alicia m hirsch, rebecca greif, thomas b hildebrandt.
- Author information
- Copyright and License information
Correspondence concerning this manuscript may be directed to Katharine L. Loeb, Ph.D., Department of Psychology, Fairleigh Dickinson University, 1000 River Road, T-WH1-01, Teaneck, New Jersey, 07666-1914, [email protected] or [email protected]
This paper describes the successful application of family-based treatment (FBT) for a 17-year-old identical twin presenting with a four-month history of clinically significant symptoms of anorexia nervosa (AN). FBT is a manualized treatment that has been studied in randomized controlled trials for adolescents with AN. This case study illustrates the administration of this evidence-based intervention in a clinical setting, highlighting how the best available research was used to make clinical decisions at each stage of treatment delivery.
This paper describes the successful application of family-based treatment (FBT) ( Lock, Le Grange, Agras & Dare, 2001 ) for a 17-year-old identical twin presenting with a four-month history of clinically significant symptoms of anorexia nervosa (AN). FBT is a manualized treatment that has been studied in randomized controlled trials (RCTs) for adolescents with AN ( Eisler, Dare, Hodes, Russell, Dodge, & Le Grange, 2000 ; Le Grange, Eisler, Dare, & Russell, 1992 ; Lock, Agras, Bryson, & Kraemer, 2005 ; Russell, Szmukler, Dare, & Eisler, 1987 ). This case study illustrates the administration of this evidence-based intervention in a clinical setting, highlighting how the best available research was used to make clinical decisions at each stage of treatment delivery. The parents, patient, and sibling provided permission for de-identified case information to be used in this study; in addition, aspects of descriptive and clinical data have been altered to protect the anonymity of the family.
FBT for AN was originally developed and tested at the Maudsley Hospital in London, England, on a population of adolescents and adults, and was found to be particularly efficacious for patients 18 and younger with a three-year or shorter duration of illness both at one-year post-hospitalization ( Russell, et al., 1987 ) and at five-year follow-up ( Eisler, Dare, Russell, Szmukler, Le Grange, & Dodge, 1997 ). Since this seminal study, which provided initial evidence of FBT’s utility in preventing relapse and facilitating continued improvement following inpatient weight restoration, FBT for adolescent AN has been subjected to further study in additional RCTs, open trials, and clinical case series. Collectively, this literature has demonstrated that FBT is effective for a full course of weight restoration ( Eisler, et al., 2000 ; Le Grange et al., 1992 ; Lock et al., 2005 ) and that gains are sustained several years after treatment ends ( Eisler, et al., 1997 ; Eisler, Simic, Russell, & Dare, 2007 ; Lock, Couturier, & Agras, 2006 ). Further, a version of FBT in which parents are seen separately from their adolescent is superior to the traditional conjoint family therapy format for families with high levels of expressed emotion ( Eisler et al., 2000 ; Le Grange et al., 1992 ). Also, an abbreviated, 10-session course of FBT is as efficacious as the manualized 20-session version ( Lock et al., 2005 ); FBT is feasible and effective when administered by investigators other than its developers ( Loeb et al., 2007 ) and it appears effective for children in addition to adolescents ( Lock, Le Grange, Forsburg, & Hewell, 2006 ).
FBT for AN is manualized and a full description of the protocol has been published ( Lock et al., 2001 ). In summary, FBT is designed to mobilize parents in helping their ill child ultimately achieve remission from AN. Restoring weight and returning the adolescent to her chronologically appropriate stage of physical and psychosocial development are the primary immediate goals of treatment. FBT assumes an agnostic stance with regard to etiology of AN, and actively works to reduce self- and other-directed blame in the family about cause of illness. Parents are seen as a resource for dismantling the individual and environmental factors maintaining the AN. Siblings are assigned a supportive role in treatment, and parents are required to work as a team. FBT consists of three phases encompassing approximately 20 sessions. In Phase I, parents take charge of their adolescent’s eating, organizing and supervising all meals and snacks. An in-session family meal provides an opportunity for the therapist to observe the current family eating patterns and assist the parents in their new mission. Phase II, in which the parents transfer control over eating back to the adolescent, commences once the adolescent’s weight crosses back over the diagnostic threshold for AN and conflict regarding eating is significantly reduced. Phase III transitions to termination and targets more general concerns of adolescent development as the AN recedes.
In the case presented in the current paper, the family consisted of monozygotic twins discordant for AN and their biological, married parents. While this family’s positive response to treatment broadly represents a successful administration of standard FBT, several remarkable factors both at presentation and during the course of FBT merit highlighting in the report. First, the patient had continued, concurrent treatment with a psychodynamically oriented individual therapist whose case conceptualization and corresponding clinical prescriptions were discrepant with FBT. Second, there are a number of issues unique to having an unafflicted identical twin, such as seeing a constantly visible image of oneself at a normal weight and concern over the other twin’s risk for development of AN, given the substantial concordance for AN among monozygotic twins ( Bulik, Sullivan, Wade, & Kendler, 2000 ). Also, there is the tendency on the part of the unafflicted twin to function in a parental role toward her sister during the parents’ absence, in light of the sisters’ shared daily routine and history of a profound twinship bond. Third, the current case had an initial presentation of a clinically significant but technically subthreshold diagnostic profile.
Referral Information
Bella’s mother contacted the Mount Sinai Eating and Weight Disorders Program (EWDP) in November of 2006 at the suggestion of her daughter’s therapist and pediatrician. Six months prior to this, Bella began individual therapy to address her anxiety around academic performance and her perfectionistic tendencies. Bella’s therapist became concerned when she noticed that Bella had lost a significant amount of weight and initially referred her to a nutritionist. Bella had difficulty complying with the proposed meal plan and continued to lose weight. Bella’s therapist then consulted with her pediatrician and referred her to the EWDP.
Assessment and Diagnosis
Presenting problem.
Bella presented as a 17-year old Caucasian female whose parents brought her to treatment based on the collective concern that she was developing AN. Bella herself denied such a problem, reporting that she was merely trying to “eat healthier.” While the evaluation did not include full research-based measures, the diagnostic items from the Eating Disorder Examination (EDE) Version 15.0 ( Fairburn & Cooper, 1993 ), a commonly-used semistructured interview for establishing eating disorder diagnosis and assessing severity ( Pike, Roberto, Wolk, Gluck, & Walsh, 2008 ), were asked as part of the assessment. The EDE, which requires extensive training to administer and, in its complete form, takes approximately one hour to administer, is not typically used in non-research, clinical settings. The therapist also posed modified EDE diagnostic questions separately to the parents to assess their observation-based impressions of their daughter’s symptoms ( Loeb, 2005 ). Height was measured with a stadiometer and weight with a digital physician’s scale. Body mass index (BMI; weight in kilograms / the square of height in meters) was calculated and compared against CDC BMI-forage growth chart norms to assess percentile as well as percent ideal body weight, with weight corresponding to 50 th percentile BMI for age and gender (Bella’s modal growth curve percentile in childhood and adolescence) as the reference point for ideal weight. In cases where a patient’s normal pre-morbid growth trajectory has deviated consistently from the 50 th percentile, the weight at the percentile corresponding to the patient’s individual history is used as the reference point for ideal weight in our program.
Bella and her parents reported that she had lost 14 pounds over the previous 4 months, dropping from 116 pounds at a height of 62” (representing a BMI of 21.3, within normal range, a percentile of 54.5, and a percent expected body weight of 102%) to her current weight of 102 pounds (BMI 18.7, 19.5 th percentile, 89.5 % expected body weight), with the majority of the weight loss occurring over the first two months of dieting. Her last menstrual period was 10 weeks prior to presentation. Bella had been restricting both the quality and quantity of food that she ate, and she particularly avoided consuming carbohydrates, with the exception of fruit. Bella admitted that she was eating less than what her nutritionist prescribed and that she adjusted the food plan to accommodate both her “small bone structure” and reduced energy expenditure since her soccer coach, under orders from the school administration, limited her sports participation. When questioned directly, she denied a fear of weight gain, stating that she simply has a strong aesthetic preference for her current weight and shape compared to her twin sister’s body. When asked if they have reason to believe their daughter experiences a fear of weight gain (e.g., by her report to them or based on any probable manifestations of this symptom that they may have witnessed), the parents cited several behavioral indicators of fear of weight gain that they have observed in Bella, including statements such as “You’re just trying to make me fat!” when encouraged to eat a normal meal, a highly restrictive diet (i.e., fewer than 600 kcal/day), and a panicked reaction when her pediatrician told her he would like to see her gain at least one pound before their next appointment. When asked about body image disturbance in their daughter, the parents reported that Bella made repeated remarks concerning her “wide hips” and “huge thighs” and regarded herself as “fat.” Bella’s own report was consistent with her parents’ endorsement of these items.
The information obtained in this evaluation, based on Bella’s self-report and collateral data obtained from the parents, pointed to a clinical diagnosis of AN, restricting type. Notably, Bella might not have met criteria for AN in the context of a research protocol, which typically interprets DSM criteria more stringently and relies on strict weight cut-offs and direct patient endorsement of the cognitive criteria. With regard to DSM-IV Criterion A for AN [“Refusal to maintain a body weight at or above a minimally normal weight for age and height (e.g., weight loss leading to maintenance of body weight less than 85% of that expected…”)] ( APA, 2000 ), Bella’s percent expected body weight was just below 90%. Bella denied Criterion B (“Intense fear of gaining weight or becoming fat, even though underweight”), but her parents reported several behavioral indicators of fear of weight gain that they have directly observed, illustrating the importance of using multiple informants and behavioral observation to complement self-report in arriving at a psychiatric diagnosis for children and adolescents. Criterion C (“Disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or denial of the seriousness of the current low body weight”) was met by virtue of Bella’s description of her overall shape and specific body parts. In addition, she denied the seriousness of her weight loss, despite the significant concern raised by her doctors, parents, and school. Bella’s last menstrual period was 10 weeks ago, and the treatment team predicted that she would imminently meet Criterion D, which requires the absence of at least three consecutive cycles. Bella denied objective binge eating and purging but did admit to subjective binge eating episodes for which she compensated by engaging in excessive levels of exercise.
Bella had never been hospitalized for her eating disorder; however her pediatrician sent her to the emergency room in September 2006 for dehydration. Bella denied a history of other psychiatric disorders or significant psychiatric symptoms, including depression and suicidality.
Psychosocial history and family functioning
Bella reported that she had a “great” relationship with her family and that she was extremely close to her identical twin sister, Kayla. Bella achieved excellent grades in school, and described a social network consisting of her sister and their four “best friends.” Bella appeared slightly introverted during the evaluation, although she and her parents reported that Bella was the “more outgoing twin.” Her parents stated that they had raised their daughters as individuals (e.g., never dressing them alike, following their elementary school’s advice to place them in separate classrooms), but that Bella and Kayla had always identified and related as twins and had a unique form of communication when they were younger.
The parents reported that Bella’s eating pathology had been extremely stressful on the entire family, and both parents expressed deep concern about the welfare of their child. Bella’s parents appeared to have a good relationship with one another, and were committed to jointly helping their child achieve a healthy weight. They did express concern about fulfilling their professional responsibilities while participating in FBT. The parents’ psychiatric histories were significant for obsessive compulsive disorder in the mother and major depression in the father.
Treatment Plan
The therapist recommended FBT for Bella and her family. Per FBT protocol, the therapist requested that all family members, including the unafflicted twin, Kayla, attend all treatment sessions. Since the clinical assessment did not suggest high levels of criticism in the family, the therapist planned on seeing the parents and adolescent conjointly. This decision is consistent with research on the moderating effects of expressed emotion in FBT, wherein highly critical families have been shown to achieve a better outcome in a separated format of the approach ( Eisler et al., 2000 ; Le Grange et al., 1992 ). Bella’s pediatrician deemed her medically stable and provided clearance for outpatient treatment with biweekly medical monitoring.
With regard to her other concurrent treatment, the therapist supported Bella’s wish to continue in individual psychotherapy, and, after obtaining a release to exchange information, spoke to the individual therapist at length. Her own case conceptualization characterized the AN symptoms as arising from Bella’s dual challenge for successful individuation, representing a maladaptive attempt to both separate from her parents and differentiate from her twin sister. Moreover, the individual therapist had previously suggested that the parents refrain from any involvement in Bella’s eating, consistent with more traditional philosophies of AN treatment based on etiological theories of familial enmeshment and personal control. She was particularly concerned with the appropriateness of FBT for a late adolescent. However, she was willing to support the radically different approach within FBT, agreeing that hospitalization for AN – which the pediatrician was considering as an alternative – would be potentially more disruptive to Bella’s psychosocial development. The two therapists spent much time determining how the individual therapist would discuss and process FBT with Bella since it represents a diametrically opposed approach to what she initially prescribed. The family therapist explained the atheoretical nature of FBT and that she would not be presenting an alternative etiological model of the development of Bella’s eating disorder. While the strategies inherent in FBT may imply a discrepant etiological theory, the explicit messages are of blame reduction between the parents and child and of mobilizing the parents as the key resource in achieving wellness for their ill daughter. The individual therapist was most comfortable being honest with Bella about her wish to see Bella reverse the weight loss outside of the hospital and about her recognition of the positive outcomes associated with FBT, while refraining from conveying her doubts about the treatment. The two therapists agreed that neither would express even subtle disagreement with the other’s tactics to Bella or her parents, and also decided to speak on a weekly basis to ensure coordinated care, and to reduce the likelihood of splitting.
After several discussions between the therapist, Bella, her parents, and the treating nutritionist, the family determined that they would temporarily suspend nutritional counseling out of concern regarding intervention compatibility and “mixed messages” during Phase I of FBT, in which the adolescent is not expected to independently and willingly follow nutritional recommendations. However, the parents decided that they would consult with the nutritionist during Phase I if they needed assistance in determining how to best accomplish Bella’s weight restoration from a nutritional perspective. Bella did not object to postponing her next nutritional counseling session but vehemently objected to the notion that her parents would be directing her food consumption for a period of time. Nevertheless, she assented to participate in FBT.
Course of Treatment
Session one.
In FBT, the therapist begins each session by weighing the patient alone and discussing with the adolescent whether there are any issues she would like help or support raising in the family session. The weight is reviewed openly with the parents, but the adolescent can elect to report the weight or have the therapist do so. Bella lost 3.5 lbs between the evaluation and Session 1, rendering her at 86.35% expected body weight. She was pleased with the weight loss, but anxious about her parents’ reaction, stating that she doesn’t want them to worry. Bella also expressed concern that her pediatrician would hospitalize her if her weight continued to decrease. When the parents and sister joined the session, the therapist marked the new weight on a graph, showing how close Bella was to the cutoff for full AN.
Per the manual, the therapist commenced FBT with a somber family session to convey both the seriousness of the illness and that it is external to Bella herself. The purpose of these dual maneuvers is to heighten parental anxiety to the point of mobilization while reducing blame for illness directed toward the adolescent. This is crucial so that the parents can facilitate weight restoration effectively and without anger. Moreover, the therapist in FBT is explicit that the cause of AN is not known, thereby mitigating parental self-directed blame. In addition to highlighting the medical and psychological risks inherent in each of Bella’s AN-like symptoms (e.g., the risks of a highly restrictive diet, of precipitous deliberate weight loss, of restriction-induced oligomenorrhea, etc.), the therapist also emphasized that given Bella’s steep and consistent weight loss trajectory, her eating disorder had a strong potential to progress to full-blown AN, a pernicious and sometimes deadly disorder. The therapist used the analogy of the eating disorder as an octopus whose tentacles have taken hold and are squeezing harder and harder over time. This emphasis of risk for AN, beyond the risks of AN, was the only modification to the manual necessary to address Bella’s technically subthreshold presentation, which is more likely to represent an artifact of our current diagnostic system than a truly distinct clinical state ( WCEDCA, 2007 ). She also raised the issue of the family having a narrow window in which to resolve the eating disorder before college next fall.
Another goal of the first session of FBT is to take a history of how the eating disorder has affected each family member. This process provided Kayla with an opportunity to express how worried she was about her sister, how this is the only aspect of Bella she does not understand, and how alienated she feels from her twin. The parents admitted that the majority of their attention and resources have been directed to Bella recently, but Kayla was quick to deny any resentment toward her sister for this. When the therapist charged the parents at the close of Session 1 with the task of actively reversing Bella’s weight loss, Kayla immediately offered to help during lunches at school or times when their parents were unavailable. The therapist was clear that Kayla’s role was strictly to be supportive of Bella, and proscribed a supervisory or parental role for Kayla in the course of Bella’s nutritional rehabilitation. The therapist also emphasized that while weight gain would be essential to the resolution of Bella’s eating disorder, general normalization of eating behaviors is equally essential, even beyond its utility in directly facilitating weight restoration. The parents were encouraged to re-introduce foods that Bella had recently deemed forbidden, both for their caloric value in accomplishing weight gain and to directly challenge the rigid food practices dictated by Bella’s eating disorder.
The final instruction in Session 1 is for the parents to bring in a picnic meal for the family to the next session. The therapist stated, “In deciding what to bring for Bella to eat, consider her degree of weight loss and how you want to help her eat normal, healthy amounts of food again. Please include at least one food that she used to like but has stopped eating.” The parents became anxious about the details of this task, as well as about the larger job of resolving Bella’s eating disorder symptoms. They asked the therapist for a meal program so that they could plan the picnic, as well as Bella’s daily food consumption from this point forward. The therapist sensitively explained that every family approaches these tasks differently and that while the therapist has expertise in AN, the parents have expertise in their daughter and family. The therapist encouraged Bella’s parents to use common sense in determining the quantity and quality of her food, as well as the frequency of eating, stating, “You successfully fed and raised two healthy daughters, and then this illness struck Bella. Don’t be intimidated by the eating disorder or by the resistance that it will generate. Consider how you might feed Bella if she were underweight because of a medical condition.” This is consistent with the goal in FBT to empower parents. Moreover, the therapist refrained from providing more specific and directive instructions for the picnic meal, as observing if and how the basic missive was followed is an important part of the assessment that takes place in Session 2.
Session two
Bella lost another 2.7 lbs between Sessions 1 and 2. In addition, she had missed a third menstrual period. Together, the persistence of weight loss and amenorrhea now placed Bella fully within the parameters for a diagnosis of AN. When this was discussed as a family, the mother started crying, stating that she had been desperately trying to get Bella to eat since the last session, but that nothing seemed to be working. The father reported that he had been on a business trip for most of the week and that he felt guilty for the extra burden this placed on his wife for implementing the new plan. Using language consistent with the FBT goal to externalize the illness, the therapist explained that the AN was clever and was trying to thwart the parents’ efforts, and that like a parasite, it viewed Bella as a host for its own survival without a care for her suffering. The therapist reassured the parents that they would use today’s session and the picnic meal as an opportunity to refine their strategies.
One of the goals of Session 2 is to assess the family process with regard to eating. The therapist’s questions revealed that the mother had prepared the meal with consideration for her husband’s cardiovascular health diet, as well as with input from Bella, which was typical for the family in recent months. All family members participated in setting the table and laying out the food. The meal consisted of Caesar salad with fat free dressing and fat free croutons, grilled chicken breasts, whole grain rolls, fruit salad, and bottled water. The mother reported that the dressing, croutons, and rolls represented items that Bella currently avoided, and that when she reviewed the menu with Bella in advance of the session, Bella successfully negotiated for a fat-free salad and whole grain bread. Bella had cried when her mother suggested bringing brownies, previously her favorite dessert. The parents and Kayla served themselves, while Bella sat with an empty plate until her father placed an array of foods on it. Bella cut her food into small pieces and slowly ate approximately one-fourth of her chicken breast and the watermelon from her fruit salad while the remainder of the family ate normal portions of the full array of foods. When the parents encouraged Bella to eat more, she protested, stating that she was full. The parents reported that this pattern represented a typical dinner at home.
The therapist provided feedback on the meal process, explaining that by negotiating with the AN regarding meal selection, only the illness will triumph; that trying to accomplish weight gain with low-fat foods will make the course of weight gain longer and more arduous. The therapist further stated that she is confident that the parents can make good decisions about the quantities and types of food that will eradicate the AN. She reminded the parents that AN has a mortality rate that rivals some cancers, and that food is medicine in this case. She then asked the parents to convince Bella to eat at least one more bite of food, which represents the key intervention in Session 2 and an opportunity for direct coaching by the therapist as necessary. The therapist reminded Kayla that she was there to be a support to Bella.
The parents asked Bella to eat a bite of the roll and she refused, stating again that she was full. Kayla immediately offered to take a matching bite, asking Bella if it would help if Kayla did this along with her. The parents told Kayla that they appreciated her solidarity with Bella, but that Bella will need to eat a substantial amount to gain weight and they do not expect Kayla to do the same. Kayla then took Bella’s hand and held it for the remainder of the session.
With minimal additional coaching from the therapist, and a judicious blend of firmness and kindness, Bella’s parents accomplished the task of convincing her to eat the bite of the roll. In response to Bella’s protests that she was too old to be fed and it was her choice to be thin, Bella’s parents responded that they were stepping in where Bella was not able to adequately care for herself, and would not let her choose to be ill. The therapist also reminded the family that Bella’s developmentally appropriate level of autonomy in other psychosocial domains was to be preserved, and that her parents were taking control exclusively in relation to her AN – and that this was to be tapered in Phase II of FBT and ultimately stopped.
Remainder of phase I (sessions 3-7)
While the FBT manual allows for 10 sessions to complete Phase I, Bella’s family required 7, speaking both to the discrepancies between intervention protocols and naturalistic clinical course, as well as to the efficacy of shorter-term FBT as demonstrated in clinical research ( Lock et al., 2005 ). She gained a mean of 1.7 lbs per week in the remainder of Phase I. Given her initial loss, she did not surpass her evaluation weight until Session 6. At Session 7, she had reached a weight of 106 lbs, corresponding to a BMI of 19.4, a growth curve percentile of 29.5, and a percent expected body weight of 93. Notably, the transition to Phase II, in which control over eating is gradually transferred back to the adolescent, does not presume full weight restoration, but rather weight at a minimum of 87% expected (i.e., above the diagnostic threshold), in combination with reduced conflict around eating and increased parental empowerment. In Bella’s case, the weight criterion was met by Session 5, but the full complement of transition criteria was not achieved until two sessions later.
The remainder of Phase I of Bella’s treatment included the following topics and strategies. First, the father limited his business travel as much as possible. When he was away, he participated in decisions about Bella’s meals by phone. He also attended Session 4 by speakerphone. Bella’s mother decided to let her colleagues know that one of her daughters was ill and that she would need to reduce her working hours accordingly for a period of time. Bella’s parents also enlisted the help of the school nurse to monitor her lunches. Kayla ate with her as well, but was not put in the position of supervising the meal or reporting what was eaten to her parents. This was in response to Kayla’s continued tendencies to assume the parental role, especially at school. The parents also worked out with the school that Bella could return to the soccer team during Phase II of treatment. This served as a significant incentive for Bella in the weight gain process. The parents had a recurring disagreement about the amount of food Bella should be asked to eat, with the father expecting more than the mother. The therapist encouraged the parents to work this out privately and always present a united front to Bella. The parents did not consult with Bella’s nutritionist during Phase I. Initially, Bella insisted on knowing all the ingredients and food preparation details of her meals and snacks. Her parents complied, but hid certain information to reduce Bella’s anxiety. When Bella discovered their misrepresentation, she was angry and resolved to restrict her eating further. The parents altered their strategy to respond to Bella’s request for such information either with complete honesty or by reminding her that they were making decisions about what would most effectively battle the AN at a time when she could not make such decisions for herself.
In Phase I, the parents requested a private session with the therapist to discuss issues pertaining to Kayla. Since both conducting a separated session and devoting a Phase I session to concerns about another family member represent protocol deviations, the therapist and parents compromised by being open with Bella and Kayla that such a session would be taking place and about the general topic of the meeting. The parents had read about the heritability of AN and feared for Kayla’s risk for developing AN. They were especially concerned given that Bella’s outbursts had included statements such as, “You’re trying to make me fat like Kayla!” which Kayla had heard at least once in a family session. The parents had discussed with Kayla that this was the AN speaking, not her sister, but they felt that simply externalizing the illness was an insufficient response. They were also worried about the effect the negative body comparison was having on Bella and Kayla as individuals and as sisters. For example, each twin expressed extreme guilt after the outburst in session, Bella for insulting Kayla, and Kayla for raising Bella’s anxiety by functioning as a mirror. While FBT is designed to reduce anger and resentment on the part of siblings, the parents believed that Kayla was not exhibiting healthy levels of these emotions. The parents ultimately offered Kayla her own therapy to address her individual needs, which Kayla accepted.
Phase II (sessions 8-10)
Session took place approximately biweekly in this phase of treatment. Bella gained 1 lb per week, ending Phase II at 113 lbs (BMI 20.7, growth curve percentile 47.4, 99% expected body weight). It is not uncommon for the rate of weight gain to decrease in Phase II as a function of reduced parental supervision and, as in Bella’s case, a reintroduction of physical activity. In consultation with the therapist at Session 8, the parents decided to make an agreement with Bella that she could play soccer only if her weight continued to increase. The parents informed Bella that her daily food intake would need to increase to offset her physical activity. Bella chose to add to her afternoon snack and dinner. The parents decided to remain in control of the food for her first week of sports, and then assuming that she made the necessary gains, to gradually give Bella more responsibility with food. This gradual process started off with the mother supervising Bella make her own breakfast, then plan her lunch, and serve herself at dinner. This worked well, and by the end of Phase II, Bella was eating independently and having dinner with friends several times per week.
College acceptances were a major theme during the later part of Phase II. Bella and Kayla had applied to and were accepted to the same colleges, and they were trying to decide whether or not to separate for the next four years. They eventually chose to attend their mutual top choice university. Between Sessions 9-10, Bella’s menses returned. By Session 10, Bella also reported a significant decrease in concern over her weight and shape, and a renewed interest in social activities including dating. The parents and Kayla corroborated this, and the family expressed how relieved they were to be at this stage of treatment.
Phase III (sessions 11-12)
Sessions were spaced monthly during Phase III, per the FBT protocol, but there were only two sessions, at the family’s request, because of the twins’ summer and college plans. Between Sessions 10-11, Bella had lost two pounds, to 111. This frightened all family members, including Bella, who resolved to eat more. She stated that she hadn’t realized how vigilant she needed to be about her eating and that she hadn’t been consciously restricting her food intake. The therapist emphasized the importance of avoiding any weight loss, deliberate or non-purposeful, as either could trigger a relapse. By Session 12, Bella had regained the lost weight plus 0.8 additional pounds, ending treatment at 100% of expected body weight (weight 113.8, BMI 20.9, growth curve percentile 49.4), and just over two pounds shy of her baseline weight. Since all functional markers were intact, the family decided to not push the weight back to 116. Her menses was regular, and she no longer met the psychological criteria for AN, either by self- or parent-report. However, she remained sensitive to her weight and expressed a strong preference to remain within this range. In addition to addressing issues of late-adolescent development, these final sessions focused on how Bella and her parents would best identify and manage any potential relapses during the college years.
Six-Month Follow-Up and Summary
Bella was medically monitored by a physician at college, but chose not to continue in psychological treatment. Her symptom status was generally stable. A vacation home revealed a two-pound weight loss. Erring on the side of caution, Bella and her parents did not want to attribute this to normal weight fluctuations, and agreed that the weight should be actively regained. Bella was successful in this with her parents’ support, but not supervision. She reported enjoying college life. She and Kayla chose separate dormitories and different majors.
Bella’s outcome is consistent with results achieved in published RCT data on FBT, and her weight and menstrual status at termination place her in the best of three categorical outcomes applied in Maudsley studies ( Eisler et al., 2000 ; Le Grange et al., 1992 ; Lock et al., 2005 ; Russell et al., 1987 ). Weight was chosen as the primary objective measure of treatment progress because early weight gain in the course of FBT predicts remission ( Lock, Couturier, Bryson, & Agras, 2006 ), and weight is the least vulnerable to patients’ denial or distortion among the complement of diagnostic criteria for AN. The psychological criteria for AN may be denied or minimized (e.g., Couturier & Lock, 2006 ) by virtue of motivated deception, lack of insight, or, in the case of children or adolescents, because of developmental limitations in cognitive capabilities necessary to endorse abstract concepts. Similarly, tracking changes in “denial of seriousness of low body weight” may not be valid for younger patients because it is normative, not pathological, for adolescents to exhibit deficits in risk appraisal relative to adults ( Boyer, 2006 ), particularly for distal outcomes. (For a review of challenges in child/adolescent identification and classification of eating disturbance, see WCEDCA, 2007 ). This case suggests that concurrent individual psychodynamic treatment is compatible with FBT provided that the individual therapist agrees that FBT should be implemented and the two therapists communicate frequently, although its specific effect on outcome is unknown. Moreover, the success of FBT does not require that the individual therapist relinquish a distinct case formulation or personally subscribe to the approach. Finally, this report highlights the importance of early intervention for a disorder as serious as AN.
Acknowledgments
This work was supported in part by a Career Development Award granted to the first author by the NIMH (K23-MH074506).
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text revision. [ Google Scholar ]
- Bulik CM, Sullivan PF, Wade TD, Kendler KS. Twin studies of eating disorders: A review. International Journal of Eating Disorders. 2000;27:1–20. doi: 10.1002/(sici)1098-108x(200001)27:1<1::aid-eat1>3.0.co;2-q. [ DOI ] [ PubMed ] [ Google Scholar ]
- Boyer TW. The development of risk-taking: A multi-perspective review. Developmental Review. 2006;26:291–345. [ Google Scholar ]
- Couturier JL, Lock J. Denial and minimization in adolescents with anorexia nervosa. International Journal of Eating Disorders. 2006;39:212–216. doi: 10.1002/eat.20241. [ DOI ] [ PubMed ] [ Google Scholar ]
- Eisler I, Dare C, Hodes M, Russell G, Dodge E, Le Grange D. Family therapy for adolescent anorexia nervosa: The results of a controlled comparison of two family interventions. Journal of Child Psychology and Psychiatry. 2000;41:727–736. [ PubMed ] [ Google Scholar ]
- Eisler I, Dare C, Russell GFM, Szmukler G, Le Grange D, Dodge E. Family and individual therapy in anorexia nervosa: A 5-year follow-up. Archives of General Psychiatry. 1997;54:1025–1030. doi: 10.1001/archpsyc.1997.01830230063008. [ DOI ] [ PubMed ] [ Google Scholar ]
- Eisler I, Simic M, Russell GFM, Dare C. A randomised controlled treatment trial of two forms of family therapy in adolescent anorexia nervosa: A five-year follow up. Journal of Child Psychology and Psychiatry. 2007;48:552–560. doi: 10.1111/j.1469-7610.2007.01726.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- Fairburn CG, Cooper Z. The eating disorder examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature assessment and treatment. twelfth edition. New York: Guilford Press; 1993. pp. 317–360. [ Google Scholar ]
- Le Grange D, Eisler I, Dare C, Russell GFM. Evaluation of family treatments in adolescent anorexia nervosa: a pilot study. International Journal of Eating Disorders. 1992;12:347–357. [ Google Scholar ]
- Lock J, Agras WS, Bryson S, Kraemer HC. A comparison of short- and long-term family therapy for adolescent anorexia nervosa. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:632–639. doi: 10.1097/01.chi.0000161647.82775.0a. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lock J, Couturier J, Agras WS. Comparison of long-term outcomes in adolescents with anorexia nervosa treated with family therapy. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:666–672. doi: 10.1097/01.chi.0000215152.61400.ca. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lock J, Couturier J, Bryson S, Agras S. Predictors of dropout and remission in family therapy for adolescent anorexia nervosa in a randomized clinical trial. International Journal of Eating Disorders. 2006;39:639–647. doi: 10.1002/eat.20328. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lock J, Le Grange D, Agras W, Dare C. Treatment manual for anorexia nervosa: A family-based approach. New York: Guilford Publications, Inc; 2001. [ Google Scholar ]
- Lock J, Le Grange D, Forsburg S, Hewell K. Is family therapy effective for children with anorexia nervosa? Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:1323–1238. doi: 10.1097/01.chi.0000233208.43427.4c. [ DOI ] [ PubMed ] [ Google Scholar ]
- Loeb KL, Walsh BT, Lock J, Le Grange D, Jones J, Marcus S, Weaver J, Dobrow I. Open trial of family-based treatment for full and partial anorexia nervosa in adolescence: Evidence of successful dissemination. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:792–800. doi: 10.1097/chi.0b013e318058a98e. [ DOI ] [ PubMed ] [ Google Scholar ]
- Loeb KL. Eating Disorder Examination – Parent Version 2005Unpublished measure based on Fairburn CG, Cooper Z. The eating disorder examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature assessment and treatment. twelfth edition. New York: Guilford Press; 1993. pp. 317–360.
- Pike KM, Roberto C, Wolk SL, Gluck M, Walsh BT. Eating disorders measures. In: Rush AJ, First MB, Blacker D, editors. Handbook of psychiatric measures. second edition. Arlington, VA: American Psychiatric Publishing, Inc; 2008. pp. 621–647. [ Google Scholar ]
- Russell GFM, Szmukler GI, Dare C, Eisler I. An evaluation of family therapy in anorexia nervosa and bulimia nervosa. Archives of General Psychiatry. 1987;44:1047–1056. doi: 10.1001/archpsyc.1987.01800240021004. [ DOI ] [ PubMed ] [ Google Scholar ]
- Workgroup for Classification of Eating Disorders in Children and Adolescents (WCEDCA) Classification of child and adolescent eating disturbances. International Journal of Eating Disorders. 2007;40:S117–S122. doi: 10.1002/eat.20458. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (43.5 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
- Open access
- Published: 14 November 2023
Experiences of living with binge eating disorder and facilitators of recovery processes: a qualitative study
- Marit Fjerdingren Bremer 1 ,
- Lisa Garnweidner-Holme 2 ,
- Linda Nesse 1 , 3 &
- Marianne Molin 2 , 4
Journal of Eating Disorders volume 11 , Article number: 201 ( 2023 ) Cite this article
2504 Accesses
Metrics details
Binge eating disorder (BED) is the most prevalent eating disorder worldwide. BED is often associated with low quality of life and mental health problems. Given the complexity of the disorder, recovery may be challenging. Since BED was only recently specified as a diagnostic category by the World Health Organization (2021), little is known about how patients experience living with BED in everyday life. This study aimed to explore how patients experience living with BED and to investigate factors perceived as facilitating recovery.
Individual interviews were conducted with six patients in a rehabilitation programme for recovery from BED. Interviews were conducted digitally and verbally transcribed between December 2020 and January 2021. The analysis was based on Malterud’s systematic text condensation.
Being diagnosed with BED could be experienced as a relief. The participants perceived living with BED as a challenging addiction. They struggled with a low self-image and experienced a lack of understanding from others, resulting in shame. Self-compassion and social support from friends and family and through participation in a rehabilitation programme were important facilitators of recovery.
Participants perceived living with BED as a challenging addiction. They struggled with low self-esteem and experienced a lack of understanding from others, resulting in shame. Being diagnosed with BED was perceived as a relief. They appreciated that issues related to mental health were addressed during rehabilitation to better understand the complexity of BED. Knowledge about BED, as well as the difficulties of living with BED among family members and friends might help patients with BED feel less ashamed of their disorder and could thus contribute to increased self-compassion.
Plain English summary
We interviewed six patients with binge eating disorder (BED) about their experiences living with BED, which is the most prevalent eating disorder worldwide. However, difficulties diagnosing patients with BED and a lack of knowledge about BED among healthcare professionals make it challenging to provide patients with appropriate help to recover from BED. The participants in our study participated in a rehabilitation programme for BED. They experienced living with BED as a challenging addiction. Low self-image and others’ lack of understanding made the individuals ashamed of their eating disorders. Self-compassion and social support through taking part in the rehabilitation programme were important facilitators of recovery. This study indicates that more knowledge about BED among family members, friends and healthcare professionals and social support are notable facilitators for recovering from BED.
Article Highlights
Even though BED is the most prevalent eating disorder, we have limited knowledge about how patients experience living with BED and their recovery processes
Patients with BED described the disorder as a challenging addiction
Low self-image and lack of understanding by others made the participants ashamed of their disordered eating behaviours
Self-compassion and social support were perceived as core facilitators of recovery
The key characteristics of binge eating disorder (BED) are the tendency to engage in binge eating episodes during which excessive amounts of food are consumed in a short period of time, paired with a subjective sense of loss of control [ 1 ]. BED was first recognised as a diagnostic category in the fifth version of the American Diagnostic and Statistical Model of Mental Disorders (DSM) in 2013 [ 2 ]. In the European System’s International Classification of Diseases, BED was first specified in 2018 [ 3 ]. The lifetime prevalence of BED is estimated to between 1.5 and 1.9%, making it the most prevalent of the eating disorders [ 4 , 5 ]. Although BED is considered the most common eating disorder, it can be argued to be the eating disorder that receives the least attention in mental health care. Several models of environmental factors contributing to BED have been proposed [ 6 ]. These for instance include media exposure, thin-ideal internalisation, and personality traits such as negative emotionality [ 6 ]. People with overweight or obesity appear to be at particular risk of developing BED although the directionality in the relationship between overweight, obesity and BED is complex and unclear [ 7 ].
Recovery from eating disorders is a non-linear process that includes psychological and social changes, including experiences of empowerment, relationships with others, as well as improvements in body image and reductions in disordered eating patterns [ 8 ]. Given the complexity of BED, recovery can be a challenging process [ 9 ]. Recovery rates, on average, remain below 50% and largely depend on how recovery is defined [ 10 ]. Recovery from BED may be understood and defined differently by patients and health professionals [ 10 ].
There is an increasing awareness of BED in the research literature on eating disorders, with several studies exploring patients’ positive and negative experiences of participation in treatment and rehabilitation [ 11 , 12 , 13 , 14 ]. However, there appears to be fewer studies on patients’ experiences of living with BED in everyday life [ 15 , 16 , 17 , 18 , 19 ]. In qualitative studies, patients have described living with BED as characterized by experiences of guilt and shame, as well as a loss of control [ 15 , 16 , 17 , 18 , 19 ]. However, accepting the disorder and being validated by others have been described as important steps in the recovery process [ 17 ]. Furthermore, psychotherapy and person-centred treatment may facilitate recovery [ 15 , 16 , 17 ]. Although some studies have investigated patients’ experiences with recovery from BED [ 8 , 17 , 20 , 21 ], we have limited in-depth knowledge on facilitators of recovery. Knowledge about how patients experience living with and recovering from BED may be important for better informing our understanding of the influence of BED on everyday life and for tailoring treatment to best promote recovery [ 22 ]. This study explores how persons with BED experience living with this eating disorder and investigates factors that were perceived as facilitating recovery.
Design and data collection
Semi-structured individual interviews were conducted by MFB between December 2020 and January 2021. MFB holds a master’s degree in public health science and a bachelor’s degree in public nutrition. MFB currently works at a rehabilitation centre as a nutritionist with patients with obesity. The individuals in this study were recruited from another rehabilitation centre and MFB did not have former knowledge to the participants. Due to the COVID-19 pandemic, the interviews took place online using a digital platform called Visiba Care (visibacare.com), an application or web interface that offers secure communication through video. The interview guide (Additional file 1 ) was developed by MFB, LN and MM. LN is a clinical psychologist with a PhD in public health science who works in addiction research. MM holds a PhD in nutrition and is a professor in public health and public health nutrition. The themes in the interview guide were developed inductively guided by the research questions of the investigators. The interview guide was pilot tested with a patient with BED. The pilot interview did not change the interview guide. Hence, the pilot interview was included in the sample and analysis of this article. 11 participants attending the rehabilitation programme were invited to participate in the study. 6 agreed to participate. We did not include more participants because we reached information power [ 23 ], due to these 6 informants provided very relevant information for the actual research questions in the study. Before participation, the interviewees gave their written informed consent. Recruitment continued until we reached informational power related to the richness of the data [ 23 ]. Interviews were audio-recorded with a Dictaphone application [ 24 ] and lasted 45–60 min. The interviews were transcribed verbatim by MFB. All the authors read the transcribed interviews. The study was conducted in accordance with COREQ guidelines [ 25 ].
Participants and setting
The participants were all women between 30 and 70 years old. In Norway, persons who have a Body Mass Index (BMI) > 40 without comorbidities or a BMI > 35 with comorbidities qualify for treatment at rehabilitation centres [ 26 ]. In some of these centres, patients are screened for eating disorders to identify the potential coexistence of BED. Participants in this study were in treatment for obesity at one of these rehabilitation centres. Based on screening procedures after entering rehabilitation, patients who experienced co-occurring challenges with binge eating were offered participation in a rehabilitation programme focusing on coping with and recovering from BED. The screening process consisted of six questionnaires and a consultation with a psychologist. A clinical assessment was made of whether the person met BED criteria. The questionnaires explored the patients’ eating behaviours and thoughts and feelings related to food. Two questionnaires mapped the patients’ mental health, including anxiety and depressive symptoms.
As part of the rehabilitation programme, sessions were held once a week over three months. The programme involved individual and group-based sessions, with 10 participants, about behaviour change, physical activity, diet, mental health, motivation and empowerment. The group-based sessions were led by a specialist in clinical psychology and a clinical nutritionist. The group-based sessions focused on challenges with binge eating, and important parts of the group discussions were self-esteem, causes and triggers of binging, knowledge of physiological mechanisms, understanding of thoughts and emotions’ influence on behaviours, and further work on recovery. Respondents were given fictive names in the presentation of the results to secure their privacy.
The analysis was conducted by MFB and was guided by Malterud’s systematic text condensation [ 27 ], a descriptive and explorative method inspired by phenomenology. LGH, LN and MM assisted with the analysis. The analysis involved the following steps: (1) reading all the transcribed interviews to obtain an overall impression and rereading them with a focus on the study’s aim; (2) identifying and sorting meaning units representing aspects of participants’ lived experiences with BED and perceived facilitators for recovery and coding; (3) condensing the contents and meanings of each coded group and (4) synthesising the contents of each code group to generalise descriptions and concepts. The process to formulate meaning units and the subsequent coding of the content and meaning involved discussion and clearance of the text. The main focus was to discuss understanding of the text, compare main impressions and themes, which again could provide an overview of similarities and differences. We highlighted recurring citations and citations that gave information on equal topics.
We identified the following two main themes related to patients’ experiences with BED (Fig. 1 ): (1) A challenging addiction with the subthemes giving it a name , living in a negative spiral and it’s in your head ; and (2) shame with the subthemes painful thoughts and feelings , negative self-image and feeling misunderstood . We found three main themes regarding the perceived facilitators of recovery: (1) recovery is a long process with the subthemes acceptance of the disorder and give yourself time ; (2) coping with the subthemes self-compassion and strategies to manage the disorder ; (3) community with the subthemes group affiliation and social support .
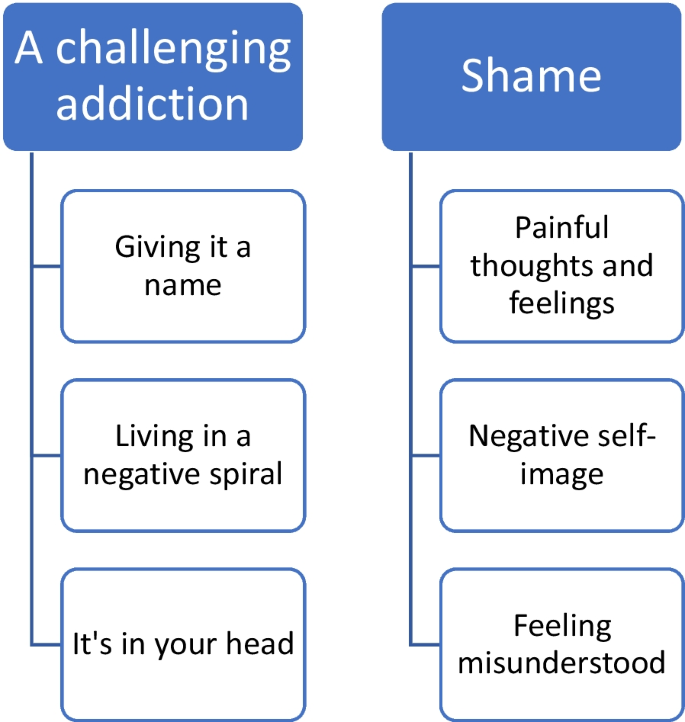
Main themes and subthemes concerning the experience of living with BED
Experiences of living with BED
The participants described living with BED as a challenging addiction . Berit explained how difficult it was to stop eating: ‘When I eat, I get happy right there and then, but when I think about it, and the dopamine or whatever it is stops working, I feel completely unsuccessful, and then I think that I can just give up. It is over. I just continue to eat. … I can’t do anything right anyway’.
Giving it a name describes participants’ experienced relief of being diagnosed with BED. The participants experienced BED as a complex condition and a challenging disorder that removed their focus from other notable areas of life. They often told stories of repeated feelings of failure in their management of BED. They felt too embarrassed to tell anyone in their lives about their diagnoses and, thus, kept it a secret, even though they thought their family members already probably knew. Their frustration with not being able to control their eating was described as confusing and time consuming. They felt hopeless and stupid. However, being diagnosed with BED was often described as a relief, which Nora expressed:
‘It’s actually been really nice. (...) I was referred because of my overweight, uhh, and based on mapping and such, I was diagnosed with binge eating disorder. And I was about to say, uhh, that I wasn’t completely surprised. I’ve realised in a way that there has been a problem, uhh, but at the same time, it was kind of good to have it confirmed (...)’.
All participants were diagnosed with BED at the rehabilitation centre.
The participants described living with BED as a negative spiral that was difficult to escape and characterised by periods of guilt when they could not control their eating habits. Tuva explained, ‘Yes, it’s like I don’t use my head. I don’t do what I’m supposed to, ehh, and I don’t enjoy it. I sit and eat with a guilty conscience’. Conversely, the participants stated that binging gave them good feelings and satisfaction. These binge eating episodes were considered a reward or a strategy to escape stressful experiences in daily life.
Dealing with binge eating was often viewed in the context of how they otherwise felt in life. A negative spiral was also mentioned concerning weight management experiences. Individuals had experiences in which they lost weight but had trouble maintaining weight loss. This led to dissatisfaction and hopelessness and resulted in episodes of increased binge eating. Some participants had lived with BED for a long time and had experienced BED as a permanent part of them.
Participants experienced BED as something that is in your head , as Pia expressed: ‘At least it starts there, that the body is a symptom of what’s in the head. I think that about my suffering, that the physical kind of reflects the mental’. It was vital for participants to understand the connection between physical and mental challenges and how these affect each other. Negative thoughts and feelings often led to binge eating episodes, and subjects appreciated the focus on mental health in the rehabilitation centre to learn strategies to cope and choose differently.
All participants associated BED with shame , as illustrated by Berit’s statement:
‘It is very taboo, very taboo. I try to hide it from everyone. When we’re with others, I don’t eat more than others, but when I’m at home and no one sees me, that’s when I eat. So, it’s tiring, and you always watch out. You never feel well enough, and uhh yeah, it really hurts’. Shame was often described as painful feelings and negative thoughts . The participants often felt ashamed when other people asked them, ‘Why can’t you just stop eating?’ This question made them feel ashamed of not being in control of their eating behaviours. In this context, the respondents explained that most binge eating episodes occurred when they were alone to avoid feelings of shame. The participants had many negative thoughts and spent much time ruminating about what others thought about them. Thus, shame often related to subjects’ negative self-image , as this comment by Pia illustrated: ‘That’s kind of what the body ideals are today, thin and slim, and if you don’t fit in that category, there’s something wrong with you’.
Several participants described having a negative self-image and critical thoughts about their bodies and behaviours. They mentioned that they already had negative self-images before developing obesity and being diagnosed with BED. Obesity was considered challenging in terms of physical limitations and mental health struggles. They described feelings of not fitting into the bodily ideals in today’s society, where thinness and health are expected.
Living with shame was also connected to a feeling of being misunderstood by family members, friends or even health professionals. Berit stated: ‘I had a doctor who said, “You just have to pull yourself together. You just have to eat right”. I think there are probably a lot of doctors who don’t have knowledge about binge eating’.
Participants experienced little openness about BED. They expressed that they feel it is more common to talk and hear about anorexia and bulimia. Having a less-known eating disorder makes it harder to be open and honest. Some kept the disorder a secret from family and friends, which again worsened their shame and hopelessness.
Facilitators of recovery processes
Recovery from BED was often considered a long process involving accepting the disorder and giving oneself time . Participants defined ‘recovery’ as the process of reducing binge eating and enhancing coping. Being healthy did not imply the total absence of binge eating episodes, but having greater control over the occurrence and amount of food consumed during binge eating episodes, as Kari explained: ‘It is about coping with it so that it does not happen so often and regularly, but to accept that it can happen once in a while and that it is normal and that you should not feel that you have failed. Because I think that when it happens once, seldom, that I have succeeded in recovering’. The participants did not perceive recovery from BED as being healthy, since they often had other diseases that they had to handle, such as diabetes.
They perceived it as important to have strategies to manage recovery, as Pia described: ‘ I think that you have to work on it continuously. But I see a change because I have gotten some tools that I can use in such situations, and I have another mindset now. I feel more relaxed’.
Managing to cope with recurring binge eating episodes was considered an important facilitator of recovery. Participants associated coping with exerting control over their eating behaviours. Many subjects felt more in control with others but felt they could lose it when they were alone, as Silje explained: ‘It’s kind of like how you compare yourself to others and how they manage to control their eating, uhh, and that's what I want, too’.
The participants often managed to have control by avoiding access to foods that triggered BED (e.g. sweets). Nora said, ‘I have the knowledge to choose the food that’s right for me, and I need to have it available’ . Furthermore, they related coping to ‘inner factors’ that influence their health and quality of life. For instance, focusing on health aspects was considered more important than focusing on weight. Health aspects were also an important motivation for recovery. Several participants explained that pain due to being overweight, such as knee arthrosis, motivated them to control their BED.
In addition, self-compassion was often mentioned as a significant facilitator of recovery. Participants gave themselves credit and bragged about periods without binge eating as positively self-reinforcing, often disrupting their negative spirals. Pia explained, ‘Self-compassion is very important for me, hm, being good with myself, being my own best friend and to think about what is good for me. Like, ‘Are episodes with binge eating good for me? No, they are not. It is better for me to go for a walk or to eat fruit’. However, the participants said that self-compassion requires awareness and practice. They highlighted getting older, gaining life experience and being more mature and reflective as factors that made it easier to give oneself acceptance.
‘Time outs’ from eating were reported as an important strategy to manage the disorder . The patients stated that breaks gave them time to reflect on why they were eating, as Berit explained: ‘It has also helped me to wait for 15 min and to eat what you like. Take a 15-min break to see if I really want to eat. Very often, you actually don’t want to. I may start to eat, but then I am at least more aware of eating.’ Another participant stated that it was important not to be too strict with oneself and not to have overly strict rules, such as ‘yes food’ and ‘no food’, to cope with BED. Good eating routines were another factor that facilitated recovery. Outdoor activities, listening to music, reading books, knitting and talking to oneself often helped interviewees to avoid new BED episodes. They appreciated that the present rehabilitation programme focused on mental health, well-being and personal relationships with food. Learning about BED gave them a better understanding that obesity did not just result from a lack of self-control and willpower.
One of the most significant facilitators for managing recovery was a community characterised by group affiliation and social support . All outlined the importance of the community at the rehabilitation centre, as Pia described: ‘It was very good to meet others in the same situation and to get validation that there are more people in the same situation and that you can talk to them openly about these episodes without being judged’.
Some participants feared how they would cope with BED once they no longer belonged to a rehabilitation programme. The perceived social support of others in the group gave them safety. Nora explained, ‘It was very good to not feel alone (…) to hear that others have the same problems. This made it easier to share my experiences. Being together with others in the same situation makes me feel safe’. The subjects learned to share BED-related experiences and feelings in the group. For recovery, they also considered it important to learn to share their feelings with others outside the programme, as Nora said: ‘I have been better about talking about my feelings at home, for example “Now I am alone, and I am sad because you are not here”’.
The participants in this study perceived living with BED as a challenging addiction. Being diagnosed with BED could be a relief; however, a negative self-image and experiencing a lack of understanding from others made the participants ashamed of their disorder. The participants experienced limited openness about BED and mental disorders in their social surroundings. Even though participants were still living with BED, perceived facilitators of recovery were self-compassion and social support received during rehabilitation.
In a study comparing how obese women with and without BED experienced binge eating [ 28 ], the authors found that women experienced BED as a form of addiction. In this context, the participants in our study experienced living with BED as characterised by negative thoughts and feelings. A review of research on emotion regulation in BED found that negative emotions play an important role in the onset and maintenance of binge eating [ 29 ]. Likewise, the participants in our study perceived living with BED as a rollercoaster ride of emotions, where the distance between positive and negative feelings was short. Experiences of living with BED as a negative spiral was also described in another study of patients with BED in the US [ 14 ].
The participants in our study often experienced living with BED as characterized by the shame of not having control over their eating habits and weight. Negative comments from family members or friends about their eating habits or obesity exacerbated shame. The participants also related shame to feeling misunderstood by family members, friends or even health professionals. This finding corroborates studies that found that patients with BED often felt misunderstood by health professionals [ 8 ]. There are indications that health professionals have limited knowledge of BED. A cross-sectional study in the US identified low awareness of and knowledge about BED among health professionals.
Shame of not having control was identified as hindering recovery in other studies [ 17 , 29 , 30 ]. For instance, a qualitative study investigating using online messages in a rehabilitation programme for BED found that self-blame promoted a feedback cycle of binging, which was perceived as barrier for recovery [ 17 ]. As mentioned in the background, some studies have investigated patients’ experiences with recovery from BED [ 8 , 17 , 20 , 21 ]. Our participants experienced recovery as a long process that mainly concerned coping. Interestingly, recovery did not imply being fully recovered from binge eating episodes but rather control over the disorder. We found that self-compassion and social support within a rehabilitation programme were the most important facilitators for recovery. Self-compassion involves developing an accepting relationship with oneself, particularly in instances of perceived failure, inadequacy and personal suffering [ 31 ], while social support constitutes the availability of potential supporters, or structural support, and the perception of support, or functional support [ 32 ]. Studies have revealed promising results for compassion-focused therapy for recovery from BED [ 33 , 34 ]. Social support may play an important role in BED recovery process [ 32 , 35 , 36 ]. An Australian mixed-methods study outlined the social support in a Instagram community as important facilitator for recovery [ 37 ]. Similarly, social support was also a notable facilitator of group-based recovery for patients with BED, combining guided physical exercise and dietary therapy in a study from Norway [ 14 ]. Our participants outlined that for recovery, they considered it important to learn to share their feelings with others outside the programme.
All of our participants outlined the importance of being part in a rehabilitation programme for recovery from BED. Several studies have investigated participants’ experiences with different rehabilitation programmes for BED [ 12 , 14 , 17 , 37 ]. For instance, a qualitative study exploring participants’ experiences of a web-based programme for bulimia and BED found that interventions should be flexible, considering individual preferences [ 38 ]. The participants in our study described the value of addressing cognitive behavioural change and mental health and appreciated receiving support from an interprofessional team that collaborated in their recovery process. However, it should be acknowledged that all of the participants were overweight or obese before their diagnosis with BED. Their experiences with previous weight-loss programmes might have influenced their preferences for addressing mental health in rehabilitation. Women with BED in the US have also reported appreciating receiving weight-neutral rehabilitation programmes for BED after experiences of being blamed for their weight and health conditions [ 11 ]. Thus, rehabilitation programmes for patients with BED should be tailored towards subjectively relevant themes to facilitate recovery.
Limitations
This study was conducted in a small sample size, which is usual for qualitative research aiming to investigate participants’ experiences [ 23 ]. However, it has to be acknowledged that the findings of this study are primarily applicable to the specific setting of the study and perhaps only transferable to patients in similar situations or rehabilitation programmes. Participants were interviewed a short time after they completed the programme. Hence, their responses might have been influenced by the focus of the content in programme in regard to facilitators for recovery. In addition, interviews were conducted digitally, which might have influenced the openness of the participants [ 39 ].
Conclusion and implications for practice
The participants perceived living with BED as a challenging addiction. They struggled with low self-esteem and experienced a lack of understanding from others, resulting in shame. They appreciated that issues related to mental health were addressed during rehabilitation to better understand the complexity of BED. Knowledge about BED as well as the difficulties of living with BED among family members and friends might help patients with BED feel less ashamed of their disorder and could thus contribute to increased self-compassion.Rehabilitation programmes should address social support in order to promote recovery from BED.
Availability of data and materials
The data analysis for this manuscript can be made available upon reasonable request by contacting the corresponding author.
Abbreviations
- Binge eating disorder
World Health Organization
Giel KE, Bulik CM, Fernandez-Aranda F, Hay P, Keski-Rahkonen A, Schag K, et al. Binge eating disorder. Nat Rev Dis Primers. 2022;8(1):16.
Article PubMed PubMed Central Google Scholar
American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders: Diagnostic and Statistical Manual of Mental Disorders. 5 ed. Arlington, VA, USA: American Psychiatric Association; 2013.
World Health Organization. International Classification of Diseases (ICD-11). The global standard for diagnostic health information 2018. Available from: https://icd.who.int/en .
Qian J, Wu Y, Liu F, Zhu Y, Jin H, Zhang H, et al. An update on the prevalence of eating disorders in the general population: a systematic review and meta-analysis. Eat Weight Disord. 2022;27(2):415–28.
Article PubMed Google Scholar
Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry. 2013;73(9):904–14.
Culbert KM, Racine SE, Klump KL. Research review: what we have learned about the causes of eating disorders—a synthesis of sociocultural, psychological, and biological research. J Child Psychol Psychiatry. 2015;56(11):1141–64.
Davis HA, Graham AK, Wildes JE. Overview of binge eating disorder. Curr Cardiovasc Risk Rep. 2020;14(12):26.
Article Google Scholar
Richmond TK, Woolverton GA, Mammel K, Ornstein RM, Spalding A, Woods ER, et al. How do you define recovery? A qualitative study of patients with eating disorders, their parents, and clinicians. Int J Eat Disord. 2020;53(8):1209–18.
de Vos JA, LaMarre A, Radstaak M, Bijkerk CA, Bohlmeijer ET, Westerhof GJ. Identifying fundamental criteria for eating disorder recovery: a systematic review and qualitative meta-analysis. J Eat Disord. 2017;5:34.
Bardone-Cone AM, Alvarez A, Gorlick J, Koller KA, Thompson KA, Miller AJ. Longitudinal follow-up of a comprehensive operationalization of eating disorder recovery: concurrent and predictive validity. Int J Eat Disord. 2019;52(9):1052–7.
Salvia MG, Ritholz MD, Craigen KLE, Quatromoni PA. Women’s perceptions of weight stigma and experiences of weight-neutral treatment for binge eating disorder: a qualitative study. EClinicalMedicine. 2023;56: 101811.
Rørtveit K, FurnesPh DB, DysvikPh DE, UelandPh DV. Patients’ experience of attending a binge eating group program—qualitative evaluation of a pilot study. SAGE Open Nurs. 2021;7:23779608211026504.
PubMed PubMed Central Google Scholar
Moghimi E, Davis C, Bonder R, Knyahnytska Y, Quilty L. Exploring women’s experiences of treatment for binge eating disorder: Methylphenidate vs cognitive behavioural therapy. Prog Neuropsychopharmacol Biol Psychiatry. 2022;114:110492.
Bakland M, Rosenvinge JH, Wynn R, Sundgot-Borgen J, FostervoldMathisen T, Liabo K, et al. Patients’ views on a new treatment for Bulimia nervosa and binge eating disorder combining physical exercise and dietary therapy (the PED-t). A qualitative study. Eat Disord. 2019;27(6):503–20.
Perelman H, Gilbert K, Grilo CM, Lydecker JA. Loss of control in binge-eating disorder: Fear and resignation. Int J Eat Disord. 2023.
Brownstone LM, Mihas P, Butler RM, Maman S, Peterson CB, Bulik CM, et al. Lived experiences of subjective binge eating: an inductive thematic analysis. Int J Eat Disord. 2021;54(12):2192–205.
Lord VM, Reiboldt W, Gonitzke D, Parker E, Peterson C. Experiences of recovery in binge-eating disorder: a qualitative approach using online message boards. Eat Weight Disord. 2018;23(1):95–105.
Salvia MG, Ritholz MD, Craigen KLE, Quatromoni PA. Managing type 2 diabetes or prediabetes and binge eating disorder: a qualitative study of patients’ perceptions and lived experiences. J Eat Disord. 2022;10(1):148.
Lewke-Bandara RS, Thapliyal P, Conti J, Hay P. It also taught me a lot about myself: a qualitative exploration of how men understand eating disorder recovery. J Eat Disord. 2020;8:3.
Eaton CM. Eating disorder recovery: a metaethnography. J Am Psychiatr Nurses Assoc. 2020;26(4):373–88.
van Bree ESJ, Slof-Op't Landt MCT, van Furth EF. Predictors of recovery in eating disorders: A focus on different definitions. Int J Eat Disord. 2023.
Bray B, Bray C, Bradley R, Zwickey H. Binge eating disorder is a social justice issue: a cross-sectional mixed-methods study of binge eating disorder experts' opinions. Int J Environ Res Public Health. 2022;19(10).
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–60.
Nettskjema Diktaphone Application. [Available from: https://www.uio.no/tjenester/it/adm-app/nettskjema/hjelp/diktafon.html .
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Norwegian Directorate for Health. Forebygging, utredning og behandling av overvekt og fedme hos voksne. Nasjonale retningslinjer for primærhelsetjenesten Oslo2011 [Available from: https://www.helsedirektoratet.no/retningslinjer/overvekt-og-fedme-hos-voksne/Overvekt%20og%20fedme%20hos%20voksne%20%E2%80%93%20Nasjonal%20faglig%20retningslinje%20for%20forebygging,%20utredning%20og%20behandling.pdf/_/attachment/inline/24ec824b-646d-4248-951f-db6b867ce6cb:4e0740b933ffd5bc03c8f0fdcab00b4135fe4ae9/Overvekt%20og%20fedme%20hos%20voksne%20%E2%80%93%20Nasjonal%20faglig%20retningslinje%20for%20forebygging,%20utredning%20og%20behandling.pdf .
Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand J Public Health. 2012;40(8):795–805.
Curtis C, Davis C. A qualitative study of binge eating and obesity from an addiction perspective. Eat Disord. 2014;22(1):19–32.
Dingemans A, Danner U, Parks M. Emotion regulation in binge eating disorder: a review. nutrients. 2017;9(11).
Duarte C, Pinto-Gouveia J, Ferreira C. Escaping from body image shame and harsh self-criticism: exploration of underlying mechanisms of binge eating. Eat Behav. 2014;15(4):638–43.
Kirby JN, Gilbert P. Commentary regarding Wilson et al. (2018) Effectiveness of ‘self-compassion’related therapies: a systematic review and meta-analysis. All is not as it seems. Mindfulness. 2019;10:1006–1016.
Verheijden MW, Bakx JC, van Weel C, Koelen MA, van Staveren WA. Role of social support in lifestyle-focused weight management interventions. Eur J Clin Nutr. 2005;59(Suppl 1):S179–86.
Kelly AC, Carter JC, Borairi S. Are improvements in shame and self-compassion early in eating disorders treatment associated with better patient outcomes? Int J Eat Disord. 2014;47(1):54–64.
Messer M, Anderson C, Linardon J. Self-compassion explains substantially more variance in eating disorder psychopathology and associated impairment than mindfulness. Body Image. 2021;36:27–33.
Hammarström A, Wiklund AF, Lindahl B, Larsson C, Ahlgren C. Experiences of barriers and facilitators to weight-loss in a diet intervention—a qualitative study of women in northern Sweden. BMC Womens Health. 2014;14:59.
Costa MB, Melnik T. Effectiveness of psychosocial interventions in eating disorders: an overview of Cochrane systematic reviews. Einstein. 2016;14(2):235–77.
Au ES, Cosh SM. Social media and eating disorder recovery: An exploration of Instagram recovery community users and their reasons for engagement. Eat Behav. 2022;46: 101651.
Yim SH, Bailey E, Gordon G, Grant N, Musiat P, Schmidt U. Exploring participants’ experiences of a web-based program for bulimia and binge eating disorder: qualitative study. J Med Internet Res. 2020;22(9): e17880.
Archibald MM, Ambagtsheer RC, Casey MG, Lawless M. Using Zoom videoconferencing for qualitative data collection: perceptions and experiences of researchers and participants. Int J Qual Methods. 2019;18:1609406919874596.
Download references
Acknowledgements
We thank the patients and the recruitment site for their participation in this study.
Not applicable.
Author information
Authors and affiliations.
Department of Public Health Science, Faculty of Landscape and Society, Norwegian University of Life Sciences, 1433, Ås, Norway
Marit Fjerdingren Bremer & Linda Nesse
Department of Nursing and Health Promotion, Faculty of Health Sciences, Oslo Metropolitan University, P.O. Box 4, St. Olavs Plass, 0130, Oslo, Norway
Lisa Garnweidner-Holme & Marianne Molin
SERAF, Norwegian Centre for Addiction Research, University of Oslo, Oslo, Norway
Linda Nesse
Department of Health and Exercise, Faculty of Health Sciences, Kristiania University College, Oslo, Norway
Marianne Molin
You can also search for this author in PubMed Google Scholar
Contributions
MFB, LN and MM designed the research. MFB performed the analysis. MFB conducted the interviews. LN, MM and LGH assisted with the analysis. MFB and LGH drafted the manuscript. LN and MM critically reviewed and revised the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Correspondence to Lisa Garnweidner-Holme .
Ethics declarations
Ethics approval and consent to participate.
The Norwegian Centre for Research Data (NSD, approval number 121485) approved the study. All subjects gave written informed consent according to the Declaration of Helsinki.
Consent for publication
Competing interests.
The authors declare that they have no conflicts of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
. Interview guide.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bremer, M.F., Garnweidner-Holme, L., Nesse, L. et al. Experiences of living with binge eating disorder and facilitators of recovery processes: a qualitative study. J Eat Disord 11 , 201 (2023). https://doi.org/10.1186/s40337-023-00929-2
Download citation
Received : 10 August 2023
Accepted : 10 November 2023
Published : 14 November 2023
DOI : https://doi.org/10.1186/s40337-023-00929-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Eating disorders
- Qualitative study
- Lived experience
- First-person perspectives
Journal of Eating Disorders
ISSN: 2050-2974
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
The medical complications of eating disorders are well established in the medical literature. 4,5 This patient was ketotic and dehydrated and essentially refused to eat, and thus she met the ...
Abstract. In the present article we review findings from an emerging body of research on attachment issues in adolescents with eating disorders from a developmental perspective. Articles for inclusion in this review were identified from PsychINFO (1966-2013), Sciencedirect (1970-2013), Psychindex (1980-2013), and Pubmed (1980-2013).
Background Most individuals with eating disorders will either recover, settle into an unrecovered but self-defined acceptable quality of life, or continue to cycle from crisis to relative stability over time. However, a minority of those with severe and enduring eating disorders recognize after years of trying that recovery remains elusive, and further treatment seems both futile and harmful ...
Eating disorders are a potentially fruitful area of study for understanding the links between values—in particular cultural values—and mental distress and disorder. Eating disorders show widely different prevalence rates across cultures, and much attention has been given to theories linking these differences with variations in cultural values.
eating disorder studies (Lebow et al., 2019; Murray et al., 2017; Rodgers et al., 2018; Vo, Lau, & Rubinstein, 2016). These findings suggest that a primary care-based approach to eating disorder identification and treatment could be more accessible for patients from diverse backgrounds. Here, we describe one case in greater detail to provide a
Abstract. Anorexia nervosa is an eating disorder characterized by excessive restriction on food intake and irrational fear of gaining weight, often accompanied by a distorted body self-perception. It is clinically diagnosed more frequently in females, with type and severity varying with each case. The current report is a case of a 25-year-old ...
In another study, men with eating disorders at 12-month follow-up had partial recovery (19%) or full recovery (14%) . Special Populations. ... Results From a Case Study. Front Psychiatry 2019, 10:731. [PMC free article] [Google Scholar] 22. Nagata JM, Golden NH, Peebles R, et al. Assessment of sex differences in bone deficits among adolescents ...
Anorexia Nervosa (AN) poses significant therapeutic challenges, especially in cases meeting the criteria for Severe and Enduring Anorexia Nervosa (SE-AN). This subset of AN is associated with severe medical complications, frequent use of services, and the highest mortality rate among psychiatric disorders. In the present case series, 14 patients were selected from those currently or previously ...
Eating disorder case study. Emma's* parents, Mr and Mrs James*, were worried about their 16 year old; for over a year she had been on a diet that didn't seem to stop. They didn't understand why she was on a diet because she had never been overweight, and it didn't seem as though she had secured any happiness from her diet.
To systematically review the literature on perceived barriers and facilitators of help-seeking for eating disorders. Informants. Patient perspective. Diverse groups of people with past or current ED or disordered eating. Most studies were based on community samples (mostly female) via advertisement. Included studies in total (number) 13 studies
This case report describes the experiences of two track athletes, one male and one female, who were recruited to the same Division 1 collegiate track program. Both were elite athletes, freshmen in the same year, experiencing the same urban college environment, and experiencing an eating disorder characterized by restrictive eating, significant ...
Eating disorders are serious conditions of increasing prevalence among young people. 1 In the UK, out-patient treatment 2 was historically delivered in generic child and adolescent mental health services (CAMHS) or highly specialised eating disorder services, with significant regional variation in provision. 3 Although there is growing evidence about the efficacy of particular treatments, 2 ...
The case of eating disorders is a case that is not easy to solve. This case study once explored the experience of ... nervosa, and binge-eating disorder [6]. In Indonesia, a study conducted by Tantiani and Syafiq in Jakarta found that there are 37.3% of adolescents experience eating disorders, with a specification of 11.6%
Despite a growing literature demonstrating the significant impacts of climate change on mental health, research is urgently needed to investigate how climate change-related concerns may contribute to the development, exacerbation, or re-emergence of eating disorders, as well as affect the effectiveness of existing interventions. This case report contributes to this scant knowledge base by ...
This case study involved the treatment of a young adult female, referred to as "Marie," who presented for treatment seeking help with her eating disorder. Marie evinced symptoms of dietary restriction, amenorrhea, low weight, and low body mass index (BMI); she was subsequently diagnosed with anorexia nervosa.
This case report describes the experiences of two track athletes, one male and one female, who were recruited to the same Division 1 collegiate track program. Both were elite athletes, freshmen in the same year, experiencing the same urban college environment, and experiencing an eating disorder characterized by restrictive eating, significant ...
Case Study Details. Maria is a 38-year-old divorced woman who works in a higher level administrative position for a large federal agency. She is well-established in her career and has several close friends with whom she enjoys spending time. She comes to you following years of unsuccessful attempts to get appropriate treatment for her binge eating.
Eating disorders (ED) are a public health concern due to their increasing prevalence and severe associated comorbidities. The aim of this study was to identify mental health and health behaviours associated with each form of EDs. A case-control study was performed: cases were patients with EDs managed for the first time in a specialized nutrition department and controls without EDs were ...
This case study illustrates the administration of this evidence-based intervention in a clinical setting, highlighting how the best available research was used to make clinical decisions at each stage of treatment delivery. ... Twin studies of eating disorders: A review. International Journal of Eating Disorders. 2000; 27:1-20. [Google ...
Eating disorders (ED), especially Anorexia Nervosa (AN), are internationally reported to have amongst the highest mortality and suicide rates in mental health. With limited evidence for current pharmacological and/or psychological treatments, there is a grave responsibility within health research to better understand outcomes for people with a lived experience of ED, factors and interventions ...
Background Binge eating disorder (BED) is the most prevalent eating disorder worldwide. BED is often associated with low quality of life and mental health problems. Given the complexity of the disorder, recovery may be challenging. Since BED was only recently specified as a diagnostic category by the World Health Organization (2021), little is known about how patients experience living with ...