Case Formulation and Disorder-Specific Models
“[Formulation is] The lynch pin that holds theory and practice together” (Butler, 1998).
- all of a patient’s symptoms, disorders, and problems;
- hypotheses about the mechanisms causing the disorders and the problems;
- proposes the recent precipitants of the current problems and disorders;
- describes the origins of the mechanisms.

Resource type
Therapy tool.
Alternative Action Formulation

Belief Driven Formulation
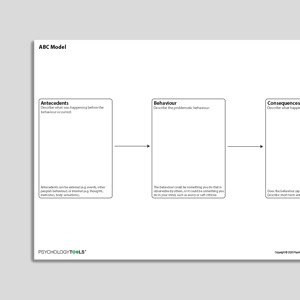
CBT Appraisal Model

Classical Conditioning
Information handouts
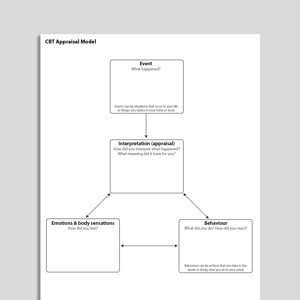
Cognitive Behavioral Model Of Anorexia Nervosa (Fairburn, Cooper, Shafran, 2003)
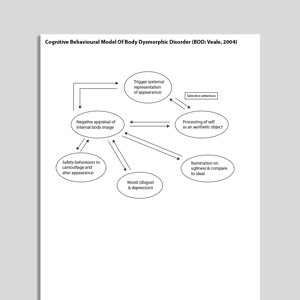
Cognitive Behavioral Model Of Body Dysmorphic Disorder (BDD: Veale, 2004)
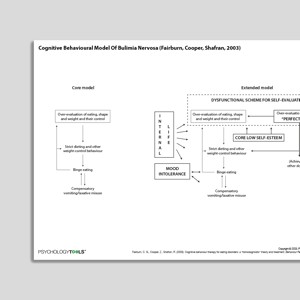
Cognitive Behavioral Model Of Bulimia Nervosa (Fairburn, Cooper, Shafran, 2003)

Cognitive Behavioral Model Of Clinical Perfectionism (Shafran, Cooper, Fairburn, 2002)
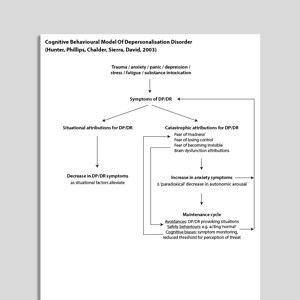
Cognitive Behavioral Model Of Depersonalization (Hunter, Phillips, Chalder, Sierra, David, 2003)
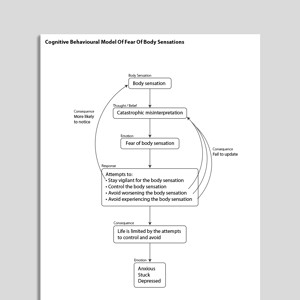
Cognitive Behavioral Model Of Fear Of Body Sensations

Cognitive Behavioral Model Of Generalized Anxiety Disorder (GAD: Dugas, Gagnon, Ladouceur, Freeston, 1998)

Cognitive Behavioral Model Of Health Anxiety (Salkovskis, Warwick, Deale, 2003)
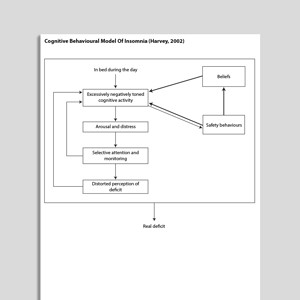
Cognitive Behavioral Model Of Insomnia (Harvey, 2002)

Cognitive Behavioral Model Of Intolerance Of Uncertainty And Generalized Anxiety Disorder Symptoms (Hebert, Dugas, 2019)
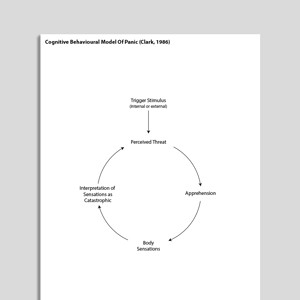
Cognitive Behavioral Model Of Panic (Clark, 1986)

Cognitive Behavioral Model Of Persistent Postural-Perceptual Dizziness (PPPD: Whalley, Cane, 2017)
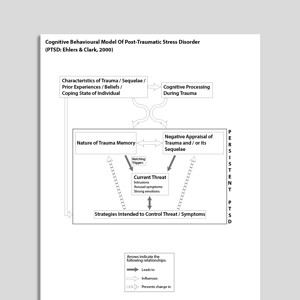
Cognitive Behavioral Model Of Post Traumatic Stress Disorder (PTSD: Ehlers & Clark, 2000)

Cognitive Behavioral Model Of Social Phobia (Clark, Wells, 1995)
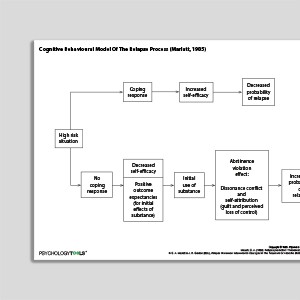
Cognitive Behavioral Model Of The Relapse Process (Marlatt & Gordon, 1985)

Cognitive Behavioral Model Of Tinnitus (McKenna, Handscombe, Hoare, Hall, 2014)

Cognitive Case Formulation

Cross Sectional Formulation

Daily Monitoring Form

Developing Psychological Flexibility

Emotion Focused Formulation

Emotions Motivate Actions

Exploring Problems Using A Cross Sectional Model

Exploring Problems Using An A-B-C Model

Friendly Formulation
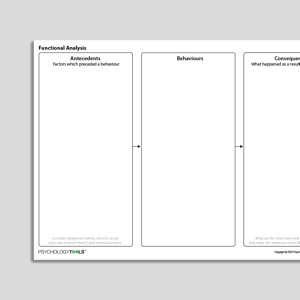
Functional Analysis

Functional Analysis With Intervention Planning

Health Anxiety Formulation

How Does Emotion Affect Your Life?

How Does This All Add Up To A Panic Attack? (Psychology Tools For Overcoming Panic)
Books & Chapters
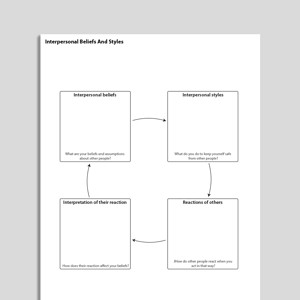
Interpersonal Beliefs And Styles

Longitudinal Formulation 1

Longitudinal Formulation 2

Low Self-Esteem Formulation

Making Sense Of Your Panic (Psychology Tools For Overcoming Panic)
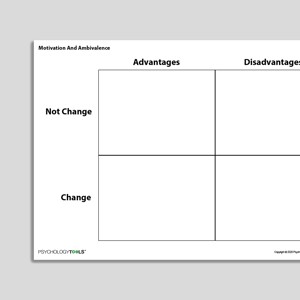
Motivation and Ambivalence

Motivational Systems (Emotional Regulation Systems)

Obsessive Compulsive Disorder (OCD) Formulation

Operant Conditioning

Panic Formulation

Problem List

Process Focused Case Formulation

PTSD Formulation

Putting It All Together (Psychology Tools For Living Well)

Reciprocal CBT Formulation

Recognizing Agoraphobia

Recognizing Anorexia Nervosa

Recognizing Binge Eating Disorder

Recognizing Body Dysmorphic Disorder

Recognizing Bulimia Nervosa

Recognizing Complex Post Traumatic Stress Disorder

Recognizing Depersonalization-Derealization Disorder (DPD)

Recognizing Generalized Anxiety Disorder (GAD)

Recognizing Hoarding Disorder

Recognizing Hypochondriasis

Recognizing Insomnia Disorders

Recognizing Obsessive Compulsive Disorder (OCD)

Recognizing Panic Disorder

Recognizing Post Traumatic Stress Disorder (PTSD)

Recognizing Prolonged Grief Disorder

Recognizing Social Anxiety Disorder

Recognizing Specific Phobia

Schema Formulation

Social Anxiety Formulation

Stages Of Change

Stages Of Social Anxiety

SWOT Analysis

The Parts Of Your Panic (Psychology Tools For Overcoming Panic)
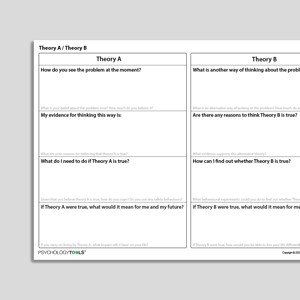
Theory A / Theory B

Theory A / Theory B (Archived)

Therapy Blueprint

Therapy Blueprint (Universal)

Therapy Blueprint For OCD

Therapy Blueprint For Panic

Therapy Blueprint For PTSD

Therapy Blueprint For Social Anxiety

Transdiagnostic Cognitive Behavioral Model Of Eating Disorders (Fairburn, Cooper, Shafran, 2003)

Transdiagnostic Processes

Treatment Planning Checklist

Understanding My Panic

Understanding PTSD

Vicious Flower Formulation

What Keeps Anorexia Going?

What Keeps Body Dysmorphic Disorder (BDD) Going?

What Keeps Bulimia Going?

What Keeps Death Anxiety Going?

What Keeps Depersonalization And Derealization Going?

What Keeps Fears And Phobias Going?

What Keeps Low Self-Esteem Going?

What Keeps Obsessive Compulsive Disorder (OCD) Going?

What Keeps Panic Going?

What Keeps Perfectionism Going?

What Keeps Post-Traumatic Stress Disorder (PTSD) Going?

What Keeps Social Anxiety Going?
Links to external resources.
Psychology Tools makes every effort to check external links and review their content. However, we are not responsible for the quality or content of external links and cannot guarantee that these links will work all of the time.
- Kuyken, W., Beshai, S., Dudley, R., Abel, A., Görg, N., Gower, P., … & Padesky, C. A. (2016). Assessing competence in collaborative case conceptualization: Development and preliminary psychometric properties of the Collaborative Case Conceptualization Rating Scale (CCC-RS).Behavioural and Cognitive Psychotherapy,44(2), 179-192. Download Primary Link Archived Link
- Rating scale & coding manual Download Primary Link Archived Link
- Score sheet & feedback form Download Primary Link Archived Link
Case Conceptualization / Case Formulation
- Formulation in Compassion Focused Therapy | Paul Gilbert | 2007 Download Archived Link
- Maxi formulation | Helen Moya Download Primary Link Archived Link
- A case formulation approach to cognitive-behavior therapy | Jacqueline Persons | 2015 Download Primary Link Archived Link
- The “Blobby” formulation | Helen Kennerley | 2015 Download Primary Link Archived Link
- Good practice guidelines on the use of psychological formulation | British Psychological Society: Division Of Clinical Psychology Download Archived Link
- A quick guide to ACT case conceptualization | Russ Harris | 2009 Download Archived Link
- Outline of ACT assessment / case formulation process | Jason Luoma Download Primary Link Archived Link
- ACT simple case formulation | Julian McNally Download Primary Link Archived Link
- Team formulation: key considerations in mental health services | Association of Clinical Psychologists UK | 2022 Download Primary Link Archived Link
- DBT Case Formulation Format | Comtois Download Archived Link
- The case formulation approach to cognitive behavior therapy | Jacqueline Persons | 2014 Download Primary Link Archived Link
Information Handouts
- Cycle vs. Heart Illustration for EFT | Paul Sigafus | 2013 Download Primary Link
Information (Professional)
- Working with Schemas, Core Beliefs, and Assumptions | Frank Wills | 2008 Download Primary Link Archived Link
Presentations
- The role of a case conceptualization model and core tasks of intervention | Donald Miechenbaum | 2014 Download Primary Link Archived Link
- Cafe formulation in cognitive-behavioral therapy | Caleb Lack Download Primary Link Archived Link
- CBT case formulation | Jacqueline Persons Download Primary Link
- Case Formulation Template Download Archived Link
Recommended Reading
Cognitive behavioral models of disorders.
- Morrison, A. P. (2001). The interpretation of intrusions in psychosis: an integrative cognitive approach to hallucinations and delusions. Behavioural and Cognitive Psychotherapy, 29(3), 257-276.
- Clark, D. M., & Wells, A. (1995). A cognitive model of social phobia.Social phobia: Diagnosis, assessment, and treatment,41(68), 00022-3.
Generalized Anxiety Disorder
- Dugas, M. J., Gagnon, F., Ladouceur, R., & Freeston, M. H. (1998). Generalized anxiety disorder: A preliminary test of a conceptual model.Behaviour research and therapy,36(2), 215-226.
- Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319-345.
- Espie, C. A. (2002). Insomnia: conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annual Review of Psychology, 53, 215–243.
- Fairburn, C. G., Cooper, Z., & Shafran, R. (2003). Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment.Behaviour Research and Therapy,41(5), 509-528.
- Fennell, M. J. (1997). Low self-esteem: A cognitive perspective. Behavioral and Cognitive Psychotherapy, 25(1), 1-26.
- Fernie, B. A., Bharucha, Z., Nikčević, A. V., Marino, C., & Spada, M. M. (2017). A Metacognitive model of procrastination. Journal of Affective Disorders, 210, 196-203.
- Garety, P. A., Kuipers, E., Fowler, D., Freeman, D., & Bebbington, P. E. (2001). A cognitive model of the positive symptoms of psychosis. Psychological Medicine, 31(2), 189-195.
- Harvey, A. G. (2002). A cognitive model of insomnia. Behavior Research and Therapy, 40, 869–894.
- Heimberg, R. G., & Becker, R. E. (1981). Cognitive and behavioral models of assertive behavior: Review, analysis and integration. Clinical Psychology Review, 1(3), 353-373.
- Mansueto, C. S., Golomb, R. G., Thomas, A. M., & Stemberger, R. M. T. (1999). A comprehensive model for behavioral treatment of trichotillomania. Cognitive and Behavioral Practice, 6(1), 23-43.
- Marlatt, G. A. (1985). Relapse prevention: Theoretical rationale and overview of the model. In G. A. Marlatt & J. R. Gordon (Eds.), Relapse prevention (1st ed., pp. 280–250). New York: Guilford Press.
- Clark, D. M. (1986). A cognitive approach to panic. Behaviour Research and Therapy, 24(4), 461-470.
Social Anxiety Disorder
- Moscovitch, D. A. (2009). What is the core fear in social phobia? A new model to facilitate individualized case conceptualization and treatment. Cognitive and Behavioural Practice, 16. 123-134 Download Archived Link
- Salkovskis, P. M., Forrester, E., & Richards, C. (1998). Cognitive–behavioral approach to understanding obsessional thinking.The British Journal of Psychiatry,173(S35), 53-63.
- Salkovskis, P. M., Warwick, H. M. C., Deale, A. C. (2003). Cognitive-Behavioral Treatment for Severe and Persistent Health Anxiety (Hypochondriasis).Brief Treatment and Crisis Intervention, 3, 353-367
- Vlaeyen, J. W. S., & Linton, S. J. (2000). Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain, 85(3), 317–332.
- Wells, A. (1995). Meta-cognition and worry: A cognitive model of generalized anxiety disorder.Behavioural and cognitive psychotherapy,23(3), 301-320 Download Archived Link
- Whalley, M. G., & Cane, D. A. (2017). A cognitive-behavioral model of persistent postural-perceptual dizziness. Cognitive and Behavioral Practice, 24(1), 72-89.

Team formulation
- Berry, K., Haddock, G., Kellett, S., Roberts, C., Drake, R., & Barrowclough, C. (2016). Feasibility of a ward‐based psychological intervention to improve staff and patient relationships in psychiatric rehabilitation settings. British Journal of Clinical Psychology, 55(3), 236-252. Download Primary Link Archived Link
- What is the case formulation approach to cognitive-behavior therapy? | Jacqueline Persons | 2008 Download Primary Link Archived Link
Case formulation / Case conceptualization
- Geisser, S., & Rizvi, S. L. (2014). The Case of” Sonia” Through the Lens of Dialectical Behavior Therapy.Pragmatic Case Studies in Psychotherapy,10(1), 30-39. Download Primary Link Archived Link
- Haynes, S. N., Leisen, M. B., Blaine, D. D. (1997). Design of individualized behavioral treatment programs using functional analytic clinical case models. Psychological Assessment, 9(4), 334-348 Download Primary Link Archived Link
- Kuyken, W., Padesky, C. A., Dudley, R. (2008). The science and practice of case conceptualization. Behavioural and Cognitive Psychotherapy, 36, 757-768 Download Archived Link
- Persons, J. B., & Lisa, S. T. (2015). Developing and Using a Case Formulation to Guide Cognitive-Behavior Therapy. Journal of Psychology & Psychotherapy, 5(2), 1 Download Primary Link Archived Link
- Special issue: Team formulation. (2015). Clinical Psychology Forum, 275. Download Archived Link
- Spencer, H. M., Dudley, R., Johnston, L., Freeston, M. H., Turkington, D., & Tully, S. (2022). Case formulation—A vehicle for change? Exploring the impact of cognitive behavioural therapy formulation in first episode psychosis: A reflexive thematic analysis. Psychology and Psychotherapy: Theory, Research and Practice. Download Primary Link Archived Link
- Boelen, P. A., van den Hout, M. A., & van den Bout, J. (2006). A Cognitive-Behavioral Conceptualization of Complicated Grief. Clinical Psychology: Science and Practice, 13(2), 109–128.
- Borkovec, T. D., Alcaine, O., & Behar, E. (2004). Avoidance theory of worry and generalized anxiety disorder.Generalized anxiety disorder: Advances in research and practice,2004.
- Chapman, A. L., Gratz, K. L., & Brown, M. Z. (2006).Solving the puzzle of deliberate self-harm: The experiential avoidance model.Behaviour Research and Therapy, 44(3), 371–394.
What Is Case Conceptualization / Case Formulation?
Types of case formulation.
Case formulations can vary according to their purpose, and according to the information they attempt to convey. A number of types of formulation have been described:
- A cross-sectional formulation presents information relevant to a short time period, as though an event were sliced open at a particular moment in time to reveal the triggering event, thoughts (interpretations/appraisals), emotions, body feelings, and behaviors or reactions. One of the most popular formats for a cross-sectional formulation is Padesky and Mooney’s ‘hot cross bun’ (1990).
- A longitudinal formulation presents information relevant to the origin and maintenance of a problem. Weerasekera’s “Multiperspective model” popularized the use of the “5 Ps” approach (presenting, predisposing, precipitating, perpetuating, and protective) to case formulation (Weerasekera, 1993). Judith Beck’s cognitive conceptualization (1995) links longitudinal factors (including relevant childhood data, core beliefs, conditional assumptions, coping strategies) to cross-sectional breakdowns (situation, automatic thought and appraisal, emotion, behavior).
- Micro-formulations have been described as a helpful way of understanding the origin and effects of troubling imagery (Hackmann, Bennett-Levy, & Holmes, 2011). In this approach problematic images are explored along with their origin, associated appraisals, current impact, maintenance factors, and cognitive consequences.
- Disorder-specific models describe the critical presenting, predisposing, precipitating, and perpetuating factors relevant to a condition. Disorder-specific cognitive behavioral conceptualizations have been published for most conditions including low self-esteem , panic , obsessive-compulsive disorder , psychosis , post-traumatic stress disorder .
- Beck, J. S. (1995). Cognitive behavior therapy: Basics and beyond . New York: Guilford Press.
- Butler, G. (1998). Clinical formulation. In A. S. Bellack and M. Hersen (eds) Comprehensive clinical psychology . New York: Pergamon Press
- Hackmann, A., Bennett-Levy, J., & Holmes, E. A. (2011). Oxford guide to imagery in cognitive therapy . New York: Oxford University Press.
- Padesky, C. A., & Mooney, K. A. (1990). Presenting the cognitive model to clients. International Cognitive Therapy Newsletter , 6 , 13–14.
- Persons, J. B. (1989). Cognitive therapy in practice: A case formulation approach . New York: WW Norton.
- Persons, J. (2008). The case formulation approach to cognitive-behavior therapy (guides to individualized evidence-based treatment).
- Weerasekera, P. (1993). Formulation: A multiperspective model. Canadian Journal of Psychiatry , 38 (5), 351–358.
- For clinicians
- For students
- Resources at your fingertips
- Designed for effectiveness
- Resources by problem
- Translation Project
- Help center
- Try us for free
- Terms & conditions
- Privacy Policy
- Cookies Policy
Case Formulation in Cognitive-Behavioral Therapy: A Principle-Driven Approach

By Gillian A. Wilson, MA, and Martin M. Antony, PhD––Department of Psychology, Ryerson University
Cognitive-behavioral treatments are often described in step-by-step manuals. They provide strategies for treating a specific psychological disorder or diagnosis as opposed to addressing the specific problems and symptoms of a particular person.
Manualized treatments may fall short as they tend to adopt a general approach to treatment versus creating a specific approach tailored to each client.
While manualized treatments may be useful under certain circumstances—for example when individuals with a specific diagnosis have highly overlapping symptoms and problems—there are circumstances that call for a more flexible, individualized approach.
Here, we will focus on this specialized method known as a case formulation .
What is case formulation and when is it useful?
A case formulation is a hypothesis about the psychological mechanisms that cause and maintain an individual’s symptoms and problems (Kuyken et al., 2009; Persons, 2008).
It’s a principle-driven approach that targets mechanisms grounded in basic psychological theories—such as cognitive theory, classical and operant conditioning.
As outlined by Persons (2008), a case formulation can be useful when:
- A client has several disorders or problems.
- No treatment manual exists for a particular disorder or problem.
- A client has numerous treatment providers.
- Problems arise that are not addressed in a manual—nonadherence or therapeutic relationship ruptures.
Steps in Case Formulation
The case formulation should be developed in collaboration with the client to ensure engagement and increase commitment to treatment.
To develop a strong case formulation, the following steps are recommended (Persons, 2008):
- Conduct a thorough assessment to determine the presence of specific diagnoses, symptoms, and problems. It’s important to create a list of all of the client’s presenting symptoms and problems in various areas and life domains (i.e., panic attacks, excessive worry, low mood, poor academic performance, relationship difficulties).
- Factors that predisposed the client to develop the symptoms and problems
- Factors that precipitated the most recent episode
- Maintaining factors
- Protective factors
- Set up experiments to test out the initial case formulation. The results of these tests will confirm or disprove hypotheses about factors that cause or maintain the client’s symptoms and problems. For example, a therapist may use a thought record to test out whether a client’s procrastination stems from perfectionistic beliefs, which may reveal that procrastination or difficulty initiating tasks is instead due to thoughts of hopelessness. The case formulation should be revised based on the results.
- The case formulation should continue to be tested and revised throughout treatment with the goal of targeting mechanisms involved in the onset and maintenance of the client’s symptoms and problems. With ongoing consent of the client, it should be used as a guide for treatment planning and clinical decision making.
Components of Case Formulation
A case formulation should provide a coherent summary and explanation of a client’s symptoms and problems. It should include the following components (Persons, 2008):
- Problems: Psychological symptoms and features of a disorder, and related problems in various areas of life—social, interpersonal, academic, occupational.
- Mechanisms: Psychological factors—cognitive, behavioral—that cause or maintain the client’s problems. Mechanisms are the primary treatment targets.
- Origins: Distal factors or processes that lead to the mechanisms and thereby predispose the client to developing certain psychological symptoms and problems.
- Precipitants: Proximal factors that trigger or worsen the client’s symptoms and problems. Precipitants can be internal—physiological symptoms that trigger a panic attack—or external—a stressful life event that triggers a depressive episode.
The following is an example of a case formulation, based on recommendations by Persons (2008). It illustrates how a case formulation approach provides a parsimonious description of the cognitive and behavioral mechanisms underlying a client’s myriad of symptoms and problems.
When Rachel was in elementary school, her classmates laughed at her during her class presentations and teased her because of her stutter (ORIGINS). This led Rachel to develop the core schemas “I am socially awkward,” and “People are overly critical.” (COGNITIVE MECHANISMS). As an adult, she was preparing for a presentation at work (PRECIPITANT), and thought to herself, “I am going to humiliate myself in front of my colleagues.” (COGNITIVE MECHANISM). This lead to feelings of anxiety (PROBLEM). As a result, she called in sick the day of her presentation (BEHAVIORAL MECHANISM) and thought “I am a failure” (COGNITIVE MECHANISM) which lead to feelings of sadness and shame (PROBLEMS). She stayed in bed all day (PROBLEM) to avoid these feelings (BEHAVIORAL MECHANISM).
See also: Exposure Therapy for Anxiety-Related Disorders
A case formulation is an invaluable tool for highlighting how a client’s problems and symptoms are related. It aids the therapist in accurately identifying and targeting underlying psychological mechanisms with increased efficiency, leading to improved therapeutic outcomes
Join Us for a Training in Your Area!
Recommended Readings
Kuyken, W., Padesky, C. A., & Dudley, R. (2009). Collaborative case conceptualization: Working effectively with clients in cognitive-behavioral therapy. New York, NY: Guilford Press.
Persons, J. B. (2008). The case formulation approach to cognitive-behavior therapy. New York, NY: Guilford Press.

In this article, I use a fictitious case study to help to describe and demonstrate how CBT Therapy can be used to reduce depression and anxiety.
CBT Therapy – A Simple Case Study
Carol is a fictional character used to explain the ways in which I may work. She presented with anxiety and feelings of depression, and hopelessness. I helped her challenge her thinking and fear.

My Response
I can hear your emotional distress and the presentation seems impossible for you at the moment. Let’s see if we can break things down and work on a little at a time, to hopefully make things feel more positive and manageable for you.
Using the ABC model of CBT.
This is based on the premise that an Activating event (A)
- In your case, it is your presentation at work.
Leads to emotional and behavioural Consequences (C)
- Which you could avoid the presentation/ phone in sick, and others will not see how well you know your stuff. This is discounting the positive.
The consequences are seen as arising from your individual belief (B)
- You described self-doubt. It makes you feel nervous and afraid, you think you might feel humiliated in front of others, and they might think you are an idiot.
From past experience, you have shared some unpleasant physical symptoms: your heart racing, feeling tongue-tied, sweating.
- These inferences could be seen as jumping to conclusions, every situation is different, and you are also describing emotional reasoning. If you do your presentation, symptoms will happen because it did last time.
You have evaluated that you cannot do it, others will judge you, and others can do better. You are magnifying the negatives, discounting the positives.
Fact – You have explained that you know your subject thoroughly and the management seem to have faith in you as they have asked you to do this. Let’s focus on this and aim to achieve your presentation.
To make this more manageable, we break things down into small tasks. We work on these smaller tasks in our sessions and as homework.
- Practice your presentation in front of others, trust the feedback, work on this and practice as necessary.
- While you concentrate on your knowledge, projection, confidence, delivery, body language and professionalism, record as necessary and we can discuss.
- Tap into the emotions and physical sensations you are feeling; we could look at grading them compared to the last time you spoke publicly and each time you practiced.
- We can practice relaxation strategies and positive thinking to help with physical symptoms and nervousness. You can continue to practice alone when in times of need.
- We will look at your common cognitive errors, look for evidence of them and disregard those that do not fit.
- We can check into your self-esteem and confidence levels and record results as we go along. Assessing progress and exploring and working on sticking points.
- I would like you to list all of the facts why you can complete your presentation, and we will explore the results.
I will support you through this Carol. I have faith in this process and in you, and evidence says you can do it. We can make a plan for the sessions/homework for the time we have before your presentation.
CBT Techniques and behavioural techniques used: The ABC Model
- Identifying faulty thoughts and feelings
- Identifying faulty thinking and looking at how it affects feelings and behaviour
- Challenging facts and focusing on positive
- Setting homework and goal and revisiting to look at progress
- Relaxation techniques
- Looking for evidence and Correcting distorted thinking
- Focusing on the client’s thoughts and feelings and underlying and irrational beliefs
- Looking at self-defeating beliefs and unrealistic beliefs
- Distinguishing between inferences and evaluations
- Teaching the client understanding and CBT method of change
- Triadic structure of CBT
- To help the client overcome blocks to change and independence
- To encourage positive thinking and change
- Looking at Schemata- underlying beliefs
- Applying distancing and decentring
- Using graded task performance
- Explaining and setting tasks/homework if the client agrees, and checking understanding.
- Explain and Test client commitment to tasks.
- Demonstrating how Carol might benefit from the sessions
- Reality testing
- Work on changing unhelpful work patterns
- Highlighting gaps between fears, experience and reality
- Review blocks and failure
- Empowering client to successfully take control
- Encouraging self-monitoring
So to summarise, for CBT therapy we work in manageable chunks. We identify the negatives and work on the fears you feel, finding strategies for you to cope and be calmer. We focus on you feeling confident and well equipped to deliver your presentation as we know you can.
About the Author:
I have many years of experience counselling individuals, young people and couples, supporting them through their struggles. I hope this article is of some help to you.
Please do get in touch through my “ Contact Me ” page to discuss your interest in CBT Therapy , or if you prefer, you are welcome to give me a call for a free introductory consultation.
Yours sincerely
BACP Accredited Counsellor Manchester
Writing a Counselling Case Study
As a counselling student, you may feel daunted when faced with writing your first counselling case study. Most training courses that qualify you as a counsellor or psychotherapist require you to complete case studies.
Before You Start Writing a Case Study

However good your case study, you won’t pass if you don’t meet the criteria set by your awarding body. So before you start writing, always check this, making sure that you have understood what is required.
For example, the ABC Level 4 Diploma in Therapeutic Counselling requires you to write two case studies as part of your external portfolio, to meet the following criteria:
- 4.2 Analyse the application of your own theoretical approach to your work with one client over a minimum of six sessions.
- 4.3 Evaluate the application of your own theoretical approach to your work with this client over a minimum of six sessions.
- 5.1 Analyse the learning gained from a minimum of two supervision sessions in relation to your work with one client.
- 5.2 Evaluate how this learning informed your work with this client over a minimum of two counselling sessions.
If you don’t meet these criteria exactly – for example, if you didn’t choose a client who you’d seen for enough sessions, if you described only one (rather than two) supervision sessions, or if you used the same client for both case studies – then you would get referred.
Check whether any more information is available on what your awarding body is looking for – e.g. ABC publishes regular ‘counselling exam summaries’ on its website; these provide valuable information on where recent students have gone wrong.
Selecting the Client
When you reflect on all the clients you have seen during training, you will no doubt realise that some clients are better suited to specific case studies than others. For example, you might have a client to whom you could easily apply your theoretical approach, and another where you gained real breakthroughs following your learning in supervision. These are good ones to choose.
Opening the Case Study
It’s usual to start your case study with a ‘pen portrait’ of the client – e.g. giving their age, gender and presenting issue. You might also like to describe how they seemed (in terms of both what they said and their body language) as they first entered the counselling room and during contracting.

If your agency uses assessment tools (e.g. CORE-10, WEMWBS, GAD-7, PHQ-9 etc.), you could say what your client scored at the start of therapy.
Free Handout Download
Writing a Case Study: 5 Tips
Describing the Client’s Counselling Journey
This is the part of the case study that varies greatly depending on what is required by the awarding body. Two common types of case study look at application of theory, and application of learning from supervision. Other possible types might examine ethics or self-awareness.
Theory-Based Case Studies
If you were doing the ABC Diploma mentioned above, then 4.1 would require you to break down the key concepts of the theoretical approach and examine each part in detail as it relates to practice. For example, in the case of congruence, you would need to explain why and how you used it with the client, and the result of this.
Meanwhile, 4.2 – the second part of this theory-based case study – would require you to assess the value and effectiveness of all the key concepts as you applied them to the same client, substantiating this with specific reasons. For example, you would continue with how effective and important congruence was in terms of the theoretical approach in practice, supporting this with reasoning.
In both, it would be important to structure the case study chronologically – that is, showing the flow of the counselling through at least six sessions rather than using the key concepts as headings.
Supervision-Based Case Studies
When writing supervision-based case studies (as required by ABC in their criteria 5.1 and 5.2, for example), it can be useful to use David Kolb’s learning cycle, which breaks down learning into four elements: concrete experience, reflective observation, abstract conceptualisation and active experimentation.
Rory Lees-Oakes has written a detailed guide on writing supervision case studies – entitled How to Analyse Supervision Case Studies. This is available to members of the Counselling Study Resource (CSR).
Closing Your Case Study
In conclusion, you could explain how the course of sessions ended, giving the client’s closing score (if applicable). You could also reflect on your own learning, and how you might approach things differently in future.

Accreditation
- Wellbeing Registration
- Conferences
- What is CBT?
- Find a Therapist

Are you a member yet? Membership is open to all and is the first step towards accreditation.
- Case Study Marking Criteria
- Close Supervision Guidelines
- Cognitive Behavioural Psychotherapist Accreditation FAQs
- Core Professions
- Knowledge Skills and Attitudes
Guidance for assessing case studies
The BABCP Minimum Training standards require that at least four training cases must be presented and formally assessed as case studies. Case studies must meet our standards for formal assessment listed below.
The BABCP case study marking criteria (formerly known as Criteria for Evaluating Academic Case studies 2013) can be downloaded here .
Case studies are normally assessed as part of post-graduate CBT training. However, not all courses include all four we require. If this applies to you, or you do not have evidence of all the passed case studies, this document provides guidance on both how to write and assess case studies marked independently for accreditation.
Details of Training Cases
The criteria for BABCP CBT Practitioner Accreditation are set out in our Minimum Training Standards (MTS 2021) -
- at least four of the eight training cases must be presented and formally assessed as case studies, a further three must have received close supervision
- written case studies should be between 2000-4000 words (or 3-5000 if extended).
- the case studies can cover the same cases that are closely supervised or they can be different
- two of your formally assessed case studies may be delivered as a ‘live’ case report or presentation instead of a written study – if so, there should be supporting information such as slides or a written summary as part of the formal assessment
- case studies must be marked as a ‘pass’
- the marker must have experience of marking CBT case studies in an academic setting
- the completed mark sheet for the case study should be submitted along with an application for accreditation
A Suitable Assessor
The assessor should be accredited by BABCP or be a CBT therapist who is trained and qualified in CBT to postgraduate diploma level or equivalent (or would meet Minimum Training Standards ).
In addition, they should have experience of marking as a lecturer or tutor on an academic post-graduate CBT training course or equivalent. The assessor may, however, currently be independent of an academic institution.
If possible, we recommend that you contact assessors from your course, local courses or through other contacts. Otherwise, you can download a list of independent assessors here . It will be your responsibility to check that they still meet the criteria for a suitable assessor and to negotiate fees, timescale and, if appropriate, reasonable adjustments with them.
Assessors are asked to confirm that the case study has passed– this means that it is of an acceptable standard for a competent CBT therapist. Feedback should be given to the candidate and expectations of quality, content, layout, writing style and structure should be of a similar standard as case studies marked in a post-graduate programme.
Reasonable adjustments should be made where appropriate where the applicant can provide evidence of relevant additional needs.
The case study should demonstrate theoretical understanding and a research-based rationale for choosing a specific approach and knowledge of alternative options, which is consistent with evidence-based CBT practice. There should be a reflective element which identifies new learning.
All the areas described below should be covered where relevant.
Evidence of structured assessment, including the following areas -
- risk assessment
- current circumstances
- details of current presenting problem(s) and/or diagnosis, including co-morbidity and reason for seeking treatment at this point
- relevant personal history including development of the problem, previous treatment(s) and current coping
- use of appropriate standardised psychometric and idiographic measures
- suitability for CBT and socialisation to the model
- identified treatment goals
- assessment of diversity and relevant socio-cultural factors
Literature Review
- detailed description, explanation and critical evaluation of relevant CBT model(s) with rationale for choice of model
- knowledge of evidence base underpinning the theoretical model and chosen intervention(s)
- any adaptations to the model needed for the case
Case Formulation
The report should outline a coherent, concise formulation developed collaboratively over treatment with explicit input from client and include-
- evidence of individualised formulation at maintenance or cross-sectional level in keeping with diagnosis specific or generic CBT model, which is appropriate to the presentation and justified by the evidence base
- explanation of links between elements in maintenance cycle
- diagrams of maintenance cycles (and longitudinal formulation, if appropriate)
- identification of a trigger or critical incident/explanation of onset of problems (precipitating factors)
- underlying beliefs/assumptions (predisposing cognitive vulnerability factors) and explanation of links between these and maintenance cycles
- explanation of how past events may have contributed to/reinforced the beliefs
- awareness of any missing elements
Course of Therapy and Outcome
- Identification of theoretical aims of treatment according to the model used, and in relation to client’s presenting difficulties and goals for treatment
- treatment plan explicitly linked to formulation
- clear identification and description of the main phases of treatment and detail on at least two specific change processes, including the cognitive and/or behavioural interventions utilised and the rationale for their use
- examples of written materials used (may be in appendices)
- justification of any deviation from model or protocol used
- identification of client’s learning
- continued refinement of formulation (if necessary)
- evaluation of outcome including progress towards treatment goals
- changes in psychometric and idiographic measures, changes to client’s general functioning and client’s evaluation of therapy relapse prevention plan
- reflection on the progress of therapy and outcome of therapy, and the therapist’s learning. Including identification of therapist and client factors that helped or hindered therapy, use of supervision, the role of the therapeutic relationship and likelihood of treatment gains being maintained
- comment on the therapeutic alliance (interpersonal process) and if relevant how difficulties in treatment or the therapeutic relationship are understood in terms of the formulation, and how these were managed
- identification of what therapist may have done differently given another chance
- broader implications for the model or evidence base
- reflection on diversity and relevant socio-cultural factors
Structure, Presentation, References
The overall presentation should include -
- coherent structure with logical flow
- clarity of communication, grammar and spelling
- use of diagrams, tables and/or figures where appropriate
- quality of referencing in text and in reference list
- limited, judicious use of appendices
Additional guidance for verbally presented case studies
The criteria for written case reports above should be applied to marking verbally presented case studies, including the assessor criteria and the requirement for the report to pass. In addition -
- the presentation should include the opportunity for assessor(s) to give feedback and ask questions
- the presentation should be a minimum of 30 minutes’ duration (which may include the time for questions)
- there should be supporting information such as slides or a written summary
- any marking criteria that relate to the written aspect of the presentation should be used to assess the verbal aspect of a verbally presented report e.g. adhering to the word count would be equivalent to adhering to the allocated time
- as with written reports, the presentation should meet the standards expected of a healthcare profession with a post-graduate level qualification e.g. accurate and detailed slides, clarity of expression, logical sequence covering the areas outlined above, clarity and coherence of the content, respect for client confidentiality, effective use of tables and figures, lack of grammatical and spelling errors, appropriate links to evidence base and referencing
Marking and Feedback
A BABCP case study feedback sheet is available here . It is optional and assessors can use a different system of ensuring and demonstrating that the case studies have met all of the requirements.
A copy of the feedback sheet should be sent to the applicant for them to include with their accreditation application.
If the case study is not marked as a pass, please provide the applicant with constructive feedback.
We may request a copy of the report in order to moderate the marking.

Thought Records in CBT: 7 Examples and Templates

The good news is that by helping people view experiences differently and changing how they think, we can alter how they react. This shift in perception can offer clients the opportunity to gain control and handle situations more effectively.
But first, it is vital to capture negative and unhelpful thinking accurately. In this article, we explore how to do that using Thought Records and introduce examples, tips, and techniques that can help.
Before you continue, we thought you might like to download these three Positive CBT Exercises for free . These science-based exercises will provide you with detailed insights into Positive CBT and give you the tools to apply it in your therapy or coaching.
This Article Contains:
What is a thought record and does it work, how are thought records used in cbt, real-life example, 3 tips for thought catching, thought records for anxiety and depression, 6 template worksheets.
- Aditional PositivePsychology.com Tools
A Take-Home Message
Unlike some forms of psychoanalysis, Cognitive-Behavioral Therapy does not focus on the past. Instead, while acknowledging the importance of earlier experiences, CBT recognizes that our current thinking shapes how events are perceived (Wilding, 2015).
Perceptions are often more crucial than actual events.
CBT addresses our current irrational, illogical, and incorrect thinking. It offers a well-researched and widely validated tool for treating anxiety, stress, and many other mental health issues (Widnall, Price, Trompetter, & Dunn, 2019).
The strength of CBT comes from it being both short term and solution focused. People also get the commonsense approach of CBT. This is essential as, according to the American Psychological Association (2017), CBT “emphasizes helping individuals learn to be their own therapists.”
While CBT can be understood by the untrained, complex and persistent problems typically require a professional’s support to make negative automatic thoughts visible and learn better ways of coping.
How do we recognize negative thinking?
Negative (and illogical and incorrect) thinking is likely to stop us from reaching short-term and life goals.
CBT does not suggest we try to block such thoughts, but rather identify them before considering their accuracy and effectiveness. Unhelpful ones can be reevaluated and replaced with thoughts that are rational and open minded.
Negative thoughts can take many forms yet often arise from specific types of thinking, for example (Wilding, 2015):
- You believe you know what others are thinking
- You expect disaster
- You tend to personalize general comments
- You generalize specific incidents
- You blame others for your thoughts and actions
As opposed to positive or even neutral thinking, such thought patterns lead us to interpret events negatively; in the long term, they can lead to depression and anxiety.
Such cognitive distortions are often automatic; they pop into our heads, unannounced and unwanted, and linger. They profoundly affect how we feel, with thoughts such as “I can’t cope” or “I feel awful,” and how we behave by avoiding opportunities and situations.
How do we capture negative thinking?
It can be useful to check in and ask ourselves if our thoughts are positive and constructive or negative and damaging throughout the day.
A simple example is given below (modified from Wilding, 2015):
Does it work?
Once identified, Thought Records (TRs) provide a practical way to capture unhelpful thinking for functional analysis and review (Beck, 2011).
Indeed, TRs are potent tools for evaluating automatic thoughts at times of distress and remain a popular choice for therapists.
Research has confirmed that TRs are highly successful at effecting belief change and are recommended for CBT practitioners working with a client (McManus, Van Doorn, & Yiend, 2012).

Completing a thought record
The more often clients practice completing TRs, the greater their awareness of negative or dysfunctional thinking.
A good time to complete a TR is shortly after noticing a change in how we feel.
Begin by asking the client to consider the following questions regarding the thinking behind a recent emotional upset, difficult situation, or concern (modified from Beck, 2011):
- Is there any evidence to support this idea?
- What is the evidence for and against it?
- Are there other explanations or viewpoints?
- What is the worst that could happen, and how would I cope?
- What is the best that could happen?
- What outcome is most realistic?
- What is the result of such automatic thinking?
The following questions encourage us to start considering how we can challenge our thinking:
- What would happen if I changed my thinking?
- What would I tell a close friend if they were in this situation?
- What should I do next?
While automatic thoughts may have some supporting evidence, that evidence is typically inadequate and inaccurate and ignores evidence to the contrary.
When ready, ask your client to complete a Thought Record Worksheet , describing:
- A situation that led to unpleasant feelings (e.g., being turned down for a job)
- The negative thoughts that arose (I’m useless)
- The emotions running through your mind (I’m ashamed)
- Your response (blame interviewer, stop applying for jobs)
- A better, more adaptive response (ask for feedback from the interviewer)
Thought challenging
Our thinking style is influenced by inherited personality traits, upbringing, and meaningful events and interprets what we experience. Two people can have precisely the same encounter yet respond very differently.
CBT is a practical way to identify and challenge unhelpful thought patterns.
Thought challenging begins with focusing on the most powerful, negative thoughts captured in the TR Worksheet.
Ask your client to complete the first few columns in the Thought Record Worksheet, describing the situation in question. Here again is an example (modified from Wilding, 2015).
Is there anything you could do differently in the future? For example, rather than jumping to conclusions, challenge your thinking with questions.
With practice, such a change in thinking can become second nature. And the act of challenging thoughts will increasingly become internalized, with no need to write them down.
You don’t need to remove all negative thinking; instead, you are trying to find a more balanced outlook.
Download 3 Free Positive CBT Exercises (PDF)
These detailed, science-based exercises will equip you or your clients with tools to find new pathways to reduce suffering and more effectively cope with life stressors.
Download 3 Free Positive CBT Tools Pack (PDF)
By filling out your name and email address below.
Sally is with her therapist and has already been asked to consider a set of questions similar to those above to evaluate her thought “Bob won’t want to go out with me” (modified from Beck, 2011).
Taking one column at a time, she completes a TR, including percentage scores to indicate likelihood or intensity:
Sally was then asked to consider what cognitive distortion category her thinking might fall into (in this case, it’s fortune telling or mind reading ). She assumed that she knew what Bob was thinking, but she didn’t.
Next, Sally was asked to consider the following set of questions, write down her thoughts, and rate the likelihood (%) of each one:
- What is the evidence that the automatic thought is true?
- Is there a different explanation?
- What’s the worst (and best) that could happen?
- What’s the most likely outcome?
- What’s the effect of believing this automatic thought?
- How could changing my thinking help?
- What should I do about it?
- What would you say to a friend?
Adaptive responses
- I don’t really know if he wants to go or not (90%).
- He is friendly to me in class (90%).
- The worst that will happen is that he will say no, and I’ll feel bad for a while, but I could talk to my friend Alison about it (90%).
- The best is that he will say yes (100%).
- The most realistic outcome is that he will say he’s busy but still be friendly to me (80%).
- If I keep assuming he doesn’t want to go with me, I won’t ask him at all (100%).
- I should just go up and ask him (50%).
- What’s the big deal anyway (75%)?
Lastly, Sally was asked to rate how much she now believes the automatic thought, how intense her sadness is, and what she would do next.
- Automatic thought – 50%
- Sad (emotion) – 50%
- I’ll ask him
Completing a TR will not remove all negative emotions, but even reducing their impact by a small amount makes the effort worthwhile.

1. Complete the TR in stages
Most clients find that TRs are incredibly useful for organizing their thoughts and considering their responses.
However, if less daunting or confusing, ask the client to complete the first four columns (date and time, situation, automatic thoughts, and emotions) in one session, and then the last two columns (adaptive response, outcome) in the next session (Beck, 2011).
2. TR alternative
TRs aren’t the only way to capture thoughts. The following questions can be used to replace the worksheet and more easily guide the client as they challenge a thought (modified from Beck, 2011):
- What is the situation? My friend didn’t call .
- What am I thinking? She doesn’t like me anymore.
- Why do I think this is true? She said she would call .
- Why might this not be true? She has forgotten to call in the past, and her mother is not well .
- What’s another way to look at this? Something important came up .
- What’s the worst outcome? She stops being my friend, and I focus on my other friends .
- What’s the best outcome? She will call and say she is sorry, but something came up .
- What will probably happen? She will call and tell me she lost her phone .
- What will happen if I keep reacting in this way? I will keep getting upset and push friends away .
- What could happen if I changed my thinking? I could feel better and check if she is okay .
- What would I tell a friend if this happened to them? Give the person extra time to call, or call to see if everything is okay .
3. Positive and negative event TRs
We don’t have to limit our focus to negative TRs; it can be useful to explore positive ones too (Wilding, 2015):
Choose a recent event and complete a TR that also includes:
- Positive thoughts – I’m excited about my new job .
- Neutral thoughts – What am I going to have for dinner ?
- Evaluative thoughts – I wonder where I will sit in my new job ?
- Rational thoughts – If it’s not the right job, I can always take another .
- Action-oriented thoughts – I’m determined to be good in my new job; if I need to do some extra hours to catch up, then that’s okay .
It’s useful to understand multiple categories of thoughts. It is then easier to spot the negative ones; for example, I will be useless in the job, and they only gave it to me because no one else showed up .
Negative thoughts are the ones that will leave you feeling upset, unhappy, and anxious.
3 Steps of thought journaling using CBT – The Lukin Center
Reviewing our TRs is a vital exercise for recognizing repeating negative (or unhelpful) behavioral patterns.
We may spot the signs of anxiety – difficulty focusing and sleeping, feeling on edge – as we review our thoughts and responses.
Perhaps rather than addressing an issue, we reduce the unwanted symptoms through avoidance. We may decline invitations to social events or refuse to apply for more senior positions at work.
While such coping mechanisms may stop us from feeling bad, they do not solve underlying problems (Wilding, 2015).
As we assess our thoughts, it can be worth asking if this will make me feel better or get better. If it is the former, it can be worth seeking other ways of addressing feelings of anxiety, such as relaxation or working on our coping techniques.
Depression can leave us exhausted. Constant tiredness and staying in bed can all be signals to watch out for when reviewing TRs.
We may misguidedly think that additional rest will mean we are more ready for the world from which we are hiding. So, we avoid the effort of doing things. We call in sick, tell friends we can’t make social events, and miss the office party.
And yet, this behavior reinforces our negative feelings. If we don’t show up, we start to believe that no one notices or cares that we are absent. We are strengthening the negative.
Wilding (2015) describes this as the all-too-much error and suggests that the answer can come from adopting a do-the-opposite approach.
By first being aware of these negative thoughts while reviewing TRs, behavior can be turned on its head. Going into work and accepting the invitation can build mastery over emotions and an all-important sense of control.

Thought Record Worksheet
This Automatic Thought Record Worksheet provides an excellent way to capture faulty thinking and begin the process of cognitive restructuring .
‘Mood first’ thought record
The following variation on the TR theme provides a simple way to record feelings , situations , and automatic thoughts in one place.
If there are multiple, automatic thoughts for the same situation, circle the strongest one (for example, I can’t take on new responsibilities ). Focus on the thoughts and feelings that upset you the most and give them a score (fearful 60% and irritated 40%).
The thought that scores the highest is the causal thought – the base thought that caused the emotions – and should be addressed first.
Assess cognitive distortions
Review the TRs and complete the Exceptions to the Problem Questionnaire to understand how each one could be responded to differently. What happened when things were better?
Finding Discrepancies
Use the Finding Discrepancies Worksheet to challenge negative thoughts.
Understanding the impact of continuing with existing behavior is extremely valuable. What happens if I continue as I am versus taking a new, healthier approach?
Cognitive Restructuring Worksheet
Use Socratic questioning in the Cognitive Restructuring Worksheet to challenge irrational or illogical thinking. For example, ask yourself:
- Could I be misinterpreting the facts?
- How likely is this scenario?
- Could others have different perspectives?
Once complete, clients can determine whether they are misinterpreting facts or repeating a habit.
Facts or opinions
We often mistake subjective opinions for facts, leading to cognitive distortions about ourselves.
Use the Facts or Opinions Worksheet to practice how to differentiate between opinion and fact.
World’s Largest Positive Psychology Resource
The Positive Psychology Toolkit© is a groundbreaking practitioner resource containing over 500 science-based exercises , activities, interventions, questionnaires, and assessments created by experts using the latest positive psychology research.
Updated monthly. 100% Science-based.
“The best positive psychology resource out there!” — Emiliya Zhivotovskaya , Flourishing Center CEO
Additional PositivePsychology.com Tools
PositivePsychology.com is a great source of information and help for Positive CBT .
The Positive Psychology Toolkit© provides various worksheets and exercises designed to help individuals conquer negative thinking.
If you’re looking for more science-based ways to help others through CBT, this collection contains 17 validated positive CBT tools for practitioners. Use them to help others overcome unhelpful thoughts and feelings and develop more positive behaviors.
Cognitive-Behavioral Therapy provides a practical way to identify and challenge illogical and incorrect thought patterns.
To address a person’s unhelpful and often untrue beliefs, we must first capture their thoughts accurately and in sufficient detail. Thought Records are an invaluable and proven aid in capturing automatic thinking that can plague us and appear believable, despite being unreliable (McManus et al., 2012).
Paying attention to what is running through our minds – thoughts and pictures – when feelings and situations change can become a positive habit, helped by writing them down.
Capturing the situation, thought, and emotion to check its accuracy begins the process of changing the way we think.
Is there a more helpful way to think about myself and what has happened ? Most likely, yes .
Use Thought Records to collect data about your clients’ specific thoughts, emotions, and behaviors, and plan a strategy for overcoming their difficulties. Include problem solving and changes to thinking and behavior to help them build a better life.
We hope you enjoyed reading this article. For more information, don’t forget to download our three Positive CBT Exercises for free .
- Beck, J. S. (2011). Cognitive behavior therapy: Basics and beyond . Guilford Press.
- McManus, F., Van Doorn, K., & Yiend, J. (2012). Examining the effects of thought records and behavioral experiments in instigating belief change. Journal of Behavior Therapy and Experimental Psychiatry , 43 (1), 540–547.
- American Psychological Association (2017). What is cognitive behavioral therapy? Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder . Retrieved November 12, 2020, from https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
- Widnall, E., Price, A., Trompetter, H., & Dunn, B. D. (2019). Routine cognitive behavioural therapy for anxiety and depression is more effective at repairing symptoms of psychopathology than enhancing wellbeing. Cognitive Therapy and Research , 44 , 28–39.
- Wilding, C. (2015). Cognitive behavioural therapy: Techniques to improve your life . Quercus.
Share this article:
Article feedback
What our readers think.
Thank you for all the information
What happened? I was not able to download the PDF of worksheets from your newsletter. Indicated the email address had already been used. Of course it has!! I get your newsletter!!!!
Thanks for reaching out – we are sorry that you are experiencing this! If you have still not received the worksheets, please email our customer support team at [email protected] , and they will help you immediately!
Kind regards, -Caroline | Community Manager
Thank you! The article was very insightful. The process to challenge the negative thinking so beneficial. I intend to read it again.
It was very useful.I feel use of CBT will certainly help a person to think in different ways whichvwill help them to be at peace.Thank you foe providing examples to understand the process of CBT. How can we effectively use this technique to treat adults with mobile or TV addiction.
Hi Vatsala,
Glad you found the post useful. That’s a tricky question. Research on mobile and TV addiction is still in the early stages, so I’m not sure how much work is out there linking the practice of thought records to treating these addictions. You may find it helpful to do a search for CBT-IA (internet addiction), which will cover different CBT techniques that apply to internet usage (and mobile phones by extension). You’ll also find a review on treatments for television addiction here .
I hope this helps a little!
– Nicole | Community Manager
Thank you. It’s very practical skills.
I enjoy reading this article. Very insightful.
thanks so much for those examples. very easy way to understand CBT concepts.
Thank you a whole lot for reminding me of this valuable thought correction process. Have a great day and year.
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

Fundamental Attribution Error: Shifting the Blame Game
We all try to make sense of the behaviors we observe in ourselves and others. However, sometimes this process can be marred by cognitive biases [...]

Halo Effect: Why We Judge a Book by Its Cover
Even though we may consider ourselves logical and rational, it appears we are easily biased by a single incident or individual characteristic (Nicolau, Mellinas, & [...]

Sunk Cost Fallacy: Why We Can’t Let Go
If you’ve continued with a decision or an investment of time, money, or resources long after you should have stopped, you’ve succumbed to the ‘sunk [...]
Read other articles by their category
- Body & Brain (49)
- Coaching & Application (58)
- Compassion (25)
- Counseling (51)
- Emotional Intelligence (23)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (20)
- Mindfulness (44)
- Motivation & Goals (45)
- Optimism & Mindset (34)
- Positive CBT (30)
- Positive Communication (21)
- Positive Education (47)
- Positive Emotions (32)
- Positive Leadership (19)
- Positive Parenting (16)
- Positive Psychology (34)
- Positive Workplace (37)
- Productivity (18)
- Relationships (44)
- Resilience & Coping (38)
- Self Awareness (21)
- Self Esteem (38)
- Strengths & Virtues (32)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)
3 Positive CBT Exercises (PDF)
- Technical Support
- Find My Rep
You are here
Low-intensity CBT Skills and Interventions a practitioner's manual
- Paul Farrand - CEDAR; University of Exeter
- Description
This book takes you step-by-step through the Low-intensity CBT interventions, competencies and clinical procedures. It provides a comprehensive manual for trainee and qualified Psychological Wellbeing Practitioners within NHS Talking Therapies anxiety and depression services or for other roles that support Low-intensity CBT.
New to this edition:
- Updated research and references
- Updated further reading and resources
- New chapters covering the different modalities available for remote LI-CBT and their benefits and drawbacks: telephone, email, and video
- New chapter on CBT Self-help in Groups
- New chapter on Working with People from Ethnic Minority Backgrounds
- New chapter on Working with Long-term Health Conditions
- Updated chapter on patient Assessment
- Updated chapter on Clinical Decision-Making
- Revised chapter on Using Behaviour Change Models
- Updated to reflect changes in the new LI-CBT National Curriculum
Supplements
Student Resources (Free to access)
1. Worksheet templates and short exercises for a patient to work through independently or a practitioner and patient to work through together are available at https://study.sagepub.com/farrand 2e
7.1 Example of a relapse prevention worksheet
12.1 Reflection record for use in clinical skills supervision
14.1 Behavioural activation schedule
14.2 Example of a classifying activity worksheet
14.3 Example of an activity grading worksheet
15.1 Thought diary
15.2 Evidence recording and revised thought
15.3 Behavioural experiments plan
15.4 Behavioural experiments review
17.1 Exposure goal diary
18.1 Jordan’s areas of my life that are really important to me
18.2 Jordan’s worry worksheet
18.3 Jordan’s my types of worry
18.4 Jordan’s my worry time
18.5 My worry time review 1
19.1 Example of an LICBT problem-solving worksheet
19.2 Jamie’s problem list
19.3 Jamie’s problem selection and potential solutions – in book but missing from worksheets
19.4 Advantages and disadvantages analysis
20.1 Sleep diary
20.2 Stimulus control worksheet
20.3 Stimulus restriction worksheet
24.1 Physical symptom diary
2. Workbooks and resources that Psychological Wellbeing Practitioners (PWP) can use in low-intensity training and practice with patients. They cover topics such as ‘Managing Your Worry’, ‘Unhelpful Thoughts’, ‘Facing Your Fears’ and support the specific interventions described in the chapters. Available at https://cedar.exeter.ac.uk/resources/iaptinterventions/
5.1 The Improving Access to Psychological Therapies Manual
5.2 Common Mental Health Disorders: Identification and Pathways to Care
12.1 IAPT Supervision Guidance
14.1 Get Active, Feel Good Workbook
14.2 Get Active, Feel Good: Helping Yourself to Get on Top of Low Mood Workbook
14.3 Case study: Jane
14.4 Case study: Mark 12.1 Unhelpful Thoughts: Challenging and Testing Them Out Workbook
15.1 Unhelpful Thoughts: Challenging and Testing Them Out Workbook
16.1 Facing Your Fears Workbook
17.1 Obsessive Compulsive Disorder: A Self-Help Book
18.1 Managing Your Worries Workbook
19.1 From Problems to Solutions Workbook
3. Obsessive Compulsive Disorder: A Self-Help Book (Lovell and Gega, 2011) is from the University of Manchester: https://documents.manchester.ac.uk/display.aspx?DocID=47030
This book provides LI IAPT trainee and practitioners need a step-by-step guide to clinical protocols and interventions, covering assessment, decision-making and the seven key interventions.
This books provides granular information on how to implement LI CBT, including suggested phrases, tips for trouble-shooting, worksheets and workbooks to support the interventions. This new edition is also updated to reflect changes in the new LI-CBT National Curriculum
Preview this book
For instructors.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 21 May 2024
Investigating nutrient biomarkers of healthy brain aging: a multimodal brain imaging study
- Christopher E. Zwilling ORCID: orcid.org/0000-0002-2873-0115 1 , 2 ,
- Jisheng Wu ORCID: orcid.org/0009-0003-6000-453X 3 , 4 , 5 &
- Aron K. Barbey ORCID: orcid.org/0000-0002-6092-0912 1 , 2 , 3 , 4 , 5 , 6
npj Aging volume 10 , Article number: 27 ( 2024 ) Cite this article
13k Accesses
539 Altmetric
Metrics details
- Cognitive ageing
The emerging field of Nutritional Cognitive Neuroscience aims to uncover specific foods and nutrients that promote healthy brain aging. Central to this effort is the discovery of nutrient profiles that can be targeted in nutritional interventions designed to promote brain health with respect to multimodal neuroimaging measures of brain structure, function, and metabolism. The present study therefore conducted one of the largest and most comprehensive nutrient biomarker studies examining multimodal neuroimaging measures of brain health within a sample of 100 older adults. To assess brain health, a comprehensive battery of well-established cognitive and brain imaging measures was administered, along with 13 blood-based biomarkers of diet and nutrition. The findings of this study revealed distinct patterns of aging, categorized into two phenotypes of brain health based on hierarchical clustering. One phenotype demonstrated an accelerated rate of aging, while the other exhibited slower-than-expected aging. A t-test analysis of dietary biomarkers that distinguished these phenotypes revealed a nutrient profile with higher concentrations of specific fatty acids, antioxidants, and vitamins. Study participants with this nutrient profile demonstrated better cognitive scores and delayed brain aging, as determined by a t-test of the means. Notably, participant characteristics such as demographics, fitness levels, and anthropometrics did not account for the observed differences in brain aging. Therefore, the nutrient pattern identified by the present study motivates the design of neuroscience-guided dietary interventions to promote healthy brain aging.
Similar content being viewed by others

Alzheimer’s disease risk reduction in clinical practice: a priority in the emerging field of preventive neurology

Associations of dietary patterns with brain health from behavioral, neuroimaging, biochemical and genetic analyses

Temporal dynamics of the multi-omic response to endurance exercise training
Introduction.
Accumulating evidence in Nutritional Cognitive Neuroscience indicates that diet and nutrition may benefit the aging brain (for a review, see ref. 1 ). A recent review of the literature surveyed 52 studies comprising more than 21,000 participants and found that dietary markers of the Mediterranean Diet were associated with healthy brain aging, as measured by MRI indices of structural and functional connectivity 2 . Despite the promise of these findings, questions remain about the causal effects of diet and nutrition on brain health and their role in age-related neurobiological decline; for example, whether elements of the Mediterranean Diet, such as polyunsaturated fatty acids (PUFAs), may limit the reduction in white matter volume with age. The potential benefits of the Mediterranean Diet may result from its focus on nutrient classes that have known functional relationships with the brain. For example, fatty acids, including monounsaturated, polyunsaturated, and saturated fatty acids, are necessary for structural brain integrity and development, cellular energy metabolism, and neurotransmission and neuromodulation 3 . Indeed, randomized controlled trials (RCTs) examining the effects of fatty acids on brain health typically observe improvements in brain function, white matter integrity, and gray matter volume 4 , 5 , 6 , 7 . Notably, however, RCTs that investigate the effects of fatty acids on cognitive performance (without additional measures of brain health) demonstrate mixed results, with positive 8 or null findings 9 . In addition to fatty acids, the Mediterranean Diet includes antioxidants (i.e., vitamins, flavonoids, and carotenoids), which are known to reduce oxidative stress and therefore to benefit brain health 10 , 11 . RCTs examining the effects of antioxidants on the aging brain demonstrate benefits in cerebral blood flow and for measures of functional brain connectivity (e.g., functional brain network integration 12 ). Evidence further suggests that antioxidants may have favorable effects on episodic memory, although these findings do not extend to all forms of memory affected by aging 7 , 13
More broadly, a large association study of ~75,000 participants revealed that greater consumption of antioxidants was associated with a lower chance of developing subjective cognitive impairment in late life 14 . Finally, research also suggests that choline, an essential nutrient that promotes structural brain integrity, cellular energy metabolism, and neurotransmission, may improve multiple facets of cognition in older adults 15 . Taken together, these findings suggest that nutrition may support and enhance cognitive function and brain health, especially in healthy older adults.
The potential for nutritional interventions to promote healthy brain function is particularly significant given the well-established effects of aging on cognitive performance and brain health 16 , 17 , 18 , 19 , 20 , 21 . Senescence is accompanied by age-related neurodegeneration in gray and white matter structures and an increase in ventricular space 22 . White matter fiber integrity declines with age, as indexed by decreased fractional anisotropy and increases in axial, radial, and mean diffusivity 23 . Concentrations of metabolic markers of neuronal integrity, measured by magnetic resonance spectroscopy (MRS), also decline with age 22 . Advancing age is associated with smaller cerebral volume, likely due to cortical neuronal degeneration and synaptic density reduction, in addition to reduced cortical thickness and surface area 24 , 25 . The observed changes in the aging brain are also known to affect cognitive function, producing declines in cognitive control, fluid intelligence, processing speed, and memory 21 , 26 , 27 , 28 , 29 .
Age-related changes in brain health are known to vary within the population, reflecting individual differences in the onset, duration, and severity of age-related neurological symptoms 19 , 30 , 31 . Thus, chronological age alone does not fully explain the complex trajectory of brain health in late life. Indeed, recent evidence demonstrates that although structural MRI measures can predict chronological age, there are often deviations in the predicted and observed aging trajectory, such that accelerated aging results in a brain that is older than expected, whereas delayed aging results in a brain that is younger than predicted 32 , 33 .
Although the literature on healthy aging has identified important risk factors that accelerate brain aging, much less is known about preventative factors that reduce the severity of neurobiological disease in late life 34 . Our research therefore sought to identify nutrient biomarker patterns that are associated with Accelerated versus Delayed Brain Aging, with an interest in guiding the development of nutritional interventions designed to promote healthy brain aging. Specifically, the present study was motivated by three primary aims. First, we sought to identify distinct phenotypes of Accelerated versus Delayed Brain Aging within a sample of 100 healthy older adults. Brain imaging measures were acquired from a comprehensive battery of over 100 neuroimaging markers of brain health, including measures of brain structure (i.e., volumetrics and white matter tracts), functional brain connectivity, and brain metabolites, as measured by MRS. Second, using a well-validated neuropsychological test battery, we compared performance on measures of intelligence, executive function, and memory in the Accelerated versus Delayed Brain Aging phenotypes. Finally, we investigated whether the observed phenotypes captured distinct nutrient biomarker profiles, with a focus on nutrients that are known to have favorable effects on cognitive function and brain health from the Mediterranean Diet (i.e., fatty acids, antioxidants, and vitamins).
We predicted that phenotypes of Accelerated versus Delayed Brain Aging would emerge, given well-established individual differences in brain aging trajectories. We also predicted that these distinct phenotypes would embody differences in cognitive function manifested by the observed differences in brain aging. Finally, our predictions about the role of nutrition in healthy brain aging were guided by findings to suggest that specific nutrients may benefit brain health, including poly- and mono-unsaturated fatty acids, vitamins, antioxidants, and carotenoids. Thus, by combining advances in Nutritional Cognitive Neuroscience—nutrient biomarkers of diet, multimodal brain imaging, and statistical modeling of brain aging—this interdisciplinary study aimed to identify nutrient profiles associated with Accelerated versus Delayed Brain Aging and to establish nutritional targets for future interventions designed to promote brain health.
Brain health phenotypes
A total of 139 variables of brain health were collected in the study, including measures of structure, function, and metabolism (Table 1 ). Brain volumes were measured separately for the left and right hemispheres for the Structural Regions listed in Table 1 , for a total of 68 regions. Total white matter integrity was measured for each of the Structural Regions in Table 1 , for a total of 34 tracts. Functional connectivity was assessed using four graph theory metrics on each of 8 brain networks, for a total of 32 measures. Finally, three metabolite concentrations were measured within each brain region.
Hierarchical clustering of all 139 brain measures collected in the study revealed two distinct phenotypes of brain health: Accelerated and Delayed Aging. Hierarchical clustering uses a similarity metric that identifies individuals who are most like one another across all brain measures. The two phenotypes identified by hierarchical clustering indicate that, across all study participants, one group is similar with less optimal brain health while the other group is similar with more optimal brain health. The dendrogram is presented in Supplementary Fig. 1 . The average value for the two phenotypes for each brain imaging domain from Table 1 —structure, metabolism, and functional connectivity—is listed in Table 2 . Relative to individuals with Accelerated Aging, those with Delayed Aging have larger brain volumes (0.48 vs 0.43), increased white matter integrity (0.61 vs 0.49), increased concentrations of brain metabolites (0.444 vs 0.441), increased functional connectivity for the whole brain (0.51 vs 0.45) and small world propensity (0.52 vs 0.43). Network functional connectivity was greater for individuals with Accelerated Aging relative to those with Delayed Aging for strength (0.57 vs 0.45), local efficiency (0.52 vs 0.47) and global efficiency (0.55 vs 0.43). Supplementary Figs. 2 , 3 and 4 present heatmaps of the values for each participant for each network or region of all brain measurements presented in Table 1 .
Brain age and brain health phenotypes
Brain Age (BA) was estimated for both brain health phenotypes. Individuals in the Accelerated Aging phenotype have an average BA of 65.1 whereas those in the Delayed Aging have an average BA of 59.7. This difference of 5.4 BA years is significant ( t statistic = 2.66, p value = 0.010). Chronological Age (CA) and BA are presented in Fig. 1 for both brain phenotypes. Many individuals in the Accelerated Aging phenotype have BAs closer to their CAs whereas many individuals in the Delayed Aging phenotype have BAs less than their CAs. Correlations between BA were computed with multiple brain modalities. BA was negatively associated with brain volumes ( r = −0.19, p value = 0.058), white matter tracts ( r = −0.37, p value = 0.00014), brain metabolites ( r = −0.25, p value = 0.017) and functional connectivity measures ( r = −0.19, p value = 0.063). These robust negative correlations suggest that a young BA is associated with the Delayed Brain Aging phenotype, indicating multiple brain modalities can predict BA specifically and brain health generally.
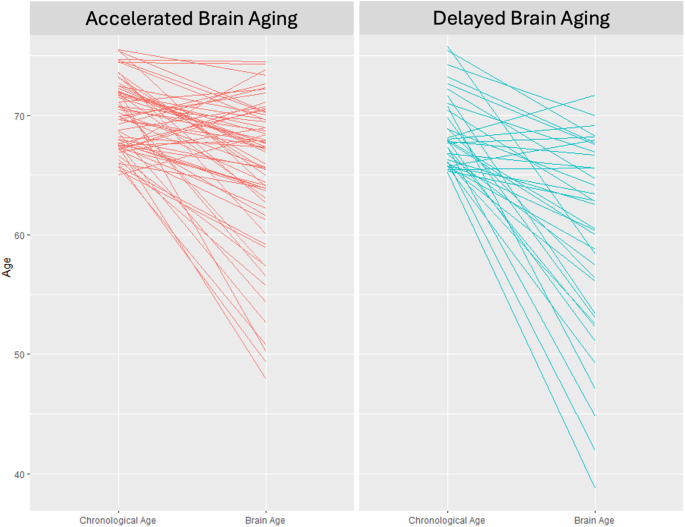
Chronological age (left side of each panel) versus brain age (right side of each panel) for the accelerated (left panel) and delayed (right panel) brain aging phenotypes.
Brain health and cognition
The study results established robust differences in brain structure, function, and metabolism between the two phenotypes of brain health. Furthermore, these phenotypes were inversely correlated with BA, where the individuals with Accelerated Aging have an Old BA and those with Delayed Aging have a Young BA. We next examined how differences in Delayed and Accelerated Brain Aging phenotypes map onto cognition. We assessed measures of intelligence (WASI), executive function (DKEFS), and memory (WMS). Individuals with Delayed Brain Aging outperformed those with Accelerated Brain Aging for all cognitive tests (see Fig. 2 ). Two scores for the Delayed Brain Aging Phenotype, reaction time (DKEFS Trails 5) and response errors (DKEFS Trails Errors), are negative and smaller than the Accelerated Brain Aging Phenotype, reflecting better cognitive performance for the Delayed Brain Aging Phenotype. A t test comparing the means between the Delayed and Accelerated Brain Aging groups is significant (p-value < 0.05) for tests of general and fluid intelligence (WASI_FSIQ4 and WASI_PRI), executive function (DKEFS_Trails.1) and memory (WMS_IMI). Supplementary Table 1 includes the scaled scores for all 15 cognitive tests.
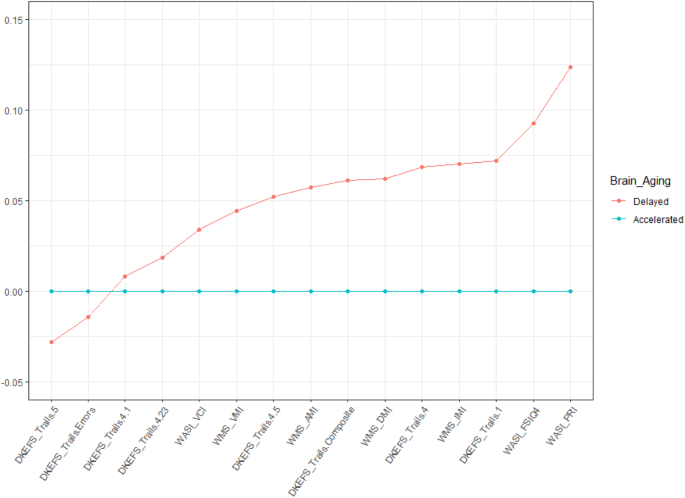
The scores for Accelerated Brain Aging were set to a baseline of 0 for each cognitive measure and the Delayed Brain Aging group is expressed as a difference relative to that baseline, with values further from the baseline reflecting a larger difference. All cognitive scores were scaled between 0 and 1.
Nutrient profile of healthy brain aging
Having established two distinct phenotypes of brain aging derived from measures of brain structure, function, and metabolism, and based on a comprehensive cognitive battery, we lastly determined the nutritional profile of the Delayed Brain Aging phenotype (illustrated in Table 3 ). We examined the nutritional status of study participants using blood-based biomarkers. The nutrient biomarker profile of individuals in the Delayed Brain Aging phenotype was characterized by greater concentrations of 13 key nutrients compared to the Accelerated Aging phenotype, as determined by a t-test comparing the group means. Notably, the observed nutrient profile encompassed several nutrient categories important for brain health, including monounsaturated fatty acids (C18:1n-7 and C20:1n-9), ω-3 polyunsaturated fatty acids (C18:3n-3 and C20:5n-3, commonly known as ALA and EPA, respectively), ω-6 polyunsaturated fatty acids (C22:2n-6 and C20:2n-6), one long-chain saturated fatty acid (C24:0), the carotenoids lutein and zeaxanthin, and vitamin E and choline (see Supplementary Table 2 ). Nutrients that did not differ between the Accelerated versus Delayed Brain Aging phenotypes include Vitamins A, B2, B6, B12, D and E, carotenoids lycopene and carotene, short and medium chain saturated fatty acids (i.e., C10:0 to C22:0), and some PUFAs (e.g., C18:4n-3 and C22:4n-6). The coefficient of variability and intraclass correlation coefficient for the blood biomarkers in Table 3 are presented in Supplementary Table 3 .
Additionally, to rule out the possibility that other covariates contributed to brain aging differences between the phenotypes, we investigated multiple measures of demographics, anthropometrics, and physical fitness collected in the study. None of these variables differed between the two phenotypes using a t-test of the means, suggesting these factors do not explain the observed differences in brain aging (see Supplementary Table 4 ). Finally, following standard conventions, we controlled for BMI, sex, income, and education by including these factors as covariates in the analysis.
Nutritional Cognitive Neuroscience aims to identify specific foods and nutrients that promote healthy brain aging. Central to this effort is the discovery of nutrient profiles that can be targeted in nutritional interventions designed to promote brain health with respect to multimodal neuroimaging measures of brain structure, function, and metabolism. The present study advances four primary conclusions pursuant to this goal.
First, we provide evidence for a multimodal characterization of healthy brain aging, classified according to neuroimaging measures associated with Delayed or Accelerated Brain Aging. Specifically, relative to Accelerated Brain Aging, older adults with Delayed Brain Aging exhibited: (1) larger brain volumes, (2) better structural DTI integrity across 34 brain regions, (3) better functional connectivity for whole brain and network-level measures of local and global efficiency, and for small world propensity, and (4) greater concentrations of the brain metabolites choline, creatine, and NAA. These findings are notable given that prior research has focused primarily on a single brain imaging modality, limiting the nature and scope of conclusions drawn about the role of diet and nutrition in healthy brain aging.
Second, Delayed Brain Aging was inversely correlated with neuroimaging biomarkers of BA, demonstrating that a younger BA is associated with favorable brain health outcomes with respect to measures of brain structure, function, and metabolism 35 .
Third, scores on cognitive assessments of intelligence, executive function, and memory were higher for older adults with Delayed Brain Aging compared to those with Accelerated Brain Aging. These results are consistently supported by findings from the cognitive neuroscience of aging, namely that older adults with larger brain volumes, white matter tracts with greater integrity, and more efficient functional connectivity also demonstrate better cognitive performance 26 , 27 , 28 .
Fourth, the discovered nutrient profile for healthy brain aging was not derived from dietary questionnaires, as is typically employed in nutritional epidemiology, but from nutrient biomarkers which accurately reflect the concentrations of nutrients from the diet 36 , 37 . The observed nutrient profile is both broad, including fatty acids, carotenoids, and vitamins, and specific, identifying the amount and type of specific nutrients in each category.
Finally, the current study identified a nutrient profile related to healthy brain aging and a clinically relevant neuroimaging biomarker of BA. Although nutrition represents an established risk factor for age-related neurological disease 34 , the potential benefits of nutrition for promoting brain health are less well understood. Thus, the nutrient pattern identified by the present study motivates the design of neuroscience-guided dietary interventions to promote healthy brain aging. We now review the primary elements of the observed nutritional pattern and the mechanisms of action that have been proposed in the nutritional sciences to explain their benefits on cognitive and brain health.
Fatty acids
In our study, the fatty acid nutritional profile of individuals in the Delayed Brain Aging phenotype includes increased concentrations of EPA, ALA, docosadienoic acid, and eicosadienoic acid, all of which are known to reduce inflammation. Inflammation makes the vascular blood–brain barrier more permeable to cytokines, and chemokines, which interfere with neuronal and glial well-being and interrupt brain homeostasis 38 , 39 , 40 . Accumulating evidence has linked increased inflammation to decline in brain structure and function, cognitive decline, and increased risk of dementia 41 , 42 , 43 . We review the relationship between inflammation and each of these fatty acids in turn below.
Eicosanoids, signaling molecules responsible for cellular functions regulating inflammation and the central nervous system, derive from competing metabolic pathways that begin with three different 20-carbon fatty acids: arachidonic acid (20:4 ω-6, AA), eicosapentaenoic acid (20:5 ω-3, EPA), and di-homo γ linolenic acid (20:3 ω-6, DGLA) 44 . The ω-6 AA pathway promotes inflammation whereas the ω-3 DGLA and EPA pathways are less inflammatory, biologically inert, or even anti-inflammatory. Moreover, the three pathways compete for the same enzymes, rate-limiting molecules, transport, and acylation pathways. Hence, the greater the presence of anti-inflammatory generating ω-3 EPA in the diet, as is observed in our nutrient profile of Delayed Brain Aging, the fewer inflammatory eicosanoids will be generated by the AA pathway.
Another nutrient in the Delayed Brain Aging phenotype related to EPA and beneficial inflammation is α-linolenic acid or ALA. ALA is one of two essential fatty acids. EPA is obtained through diet or endogenously produced, via a metabolic pathway beginning with ALA. ALA converts to EPA with 10–20% efficiency 45 . Thus, greater concentrations of ALA in the diet, as is the case for individuals with healthy brain aging, can theoretically yield more of the beneficial EPA to compete with the inflammatory AA cascade. Excellent dietary sources of EPA and ALA include fish and shellfish, flaxseed, hemp seed, olive oil, soya oil, canola oil, chia seeds, pumpkin seeds, sunflower seeds, leafy vegetables, and walnuts.
The DGLA pathway is another beneficial competitor to the AA cascade, resulting in less severe inflammation or even anti-inflammatory metabolites. Two other nutrients in the profile of Delayed Brain Aging, eicosadienoic and docosadienoic acids, are closely related to the DGLA pathway. Eicosadienoic acid is the direct precursor of DGLA while docosadienoic acid is the immediate elongation product of DGLA. These two fatty acids have antioxidant abilities and anti-inflammatory properties meeting or exceeding those of DHA 46 . They also exhibit inhibitory activity against inflammation-causing enzymes by exerting similar physiological effects as over the counter non-steroidal anti-inflammatory drugs (e.g., ibuprofen) that block the COX-I and COX-II enzymes responsible for inflammation and pain 47 .
Saturated fatty acids are traditionally viewed as unhealthy 48 . However recent research suggests some long-chain fatty acids, with more than 20 carbon atoms, may confer health benefits, with evidence suggesting that they are associated with lower risk of coronary heart disease and type 2 diabetes, and may promote healthy aging 49 . Our nutrient profile of Delayed Brain Aging includes one very long chain saturated fatty acid, lignoceric acid (C24.0). Peanuts, macadamia nuts, and certain seed oils are excellent sources of lignoceric acid 49 . A recent study demonstrated that higher concentrations of long-chain fatty acids in plasma in mid-life resulted in reduced cognitive decline in a test of verbal fluency 20 years later 50 . Another study examined the concentration of lignoceric acid in brain tissue and discovered that females without cognitive impairment exhibited a larger concentration of C24.0 compared to females who developed Alzheimer’s disease. These findings provide a rationale for suggesting that long-chain saturated fatty acids, and lignoceric acid specifically, are important biomarkers of cognitive and brain health.
The final two fatty acids discovered in our nutrient profile of Delayed Brain Aging, vaccenic and gondoic acids, are both mono-unsaturated fatty acids, or MUFAs. MUFAs, which are common in olive oil and the Mediterranean Diet, are known to support brain and cognitive health 51 . Both vaccenic and gondoic acid have robust antioxidant activities 47 . Vaccenic acid is the primary type of fat from dairy products, such as milk, butter, and yogurt. Increasing consumption of dairy products increases the concentration of vaccenic acid in plasma 52 . The importance of vaccenic acid for brain health may lie in its metabolic conversion to conjugated linoleic acid, or CLA 53 . CLA is incorporated and metabolized into brain tissue, which further extends its anti-neuroinflammatory properties 54 . Nervonic acid is the predominant fatty acid in the white matter tissue of humans and one of its metabolic precursors is gondoic acid 55 . Based on these findings, it is possible that increased dietary concentrations of vaccenic and gondoic acids may enhance white matter brain integrity, although future research in Nutritional Cognitive Neuroscience is needed to clarify the precise role of these MUFAs in brain and cognitive health.
Carotenoids
Three different carotenoids, phytopigments that give many fruits and vegetables their characteristic color, figure prominently in the nutritional profile of Delayed Brain Aging. Carotenoid-rich foods include spinach, kale, corn, bell peppers (red, green, or yellow), tomatoes, watermelon, grapefruit, cantaloupe, broccoli, and carrots. Carotenoids have known benefits to cognitive and brain health, as demonstrated by studies that examine their effects on brain structure, brain network function, and memory 7 , 56 , 57 , 58 . Carotenoids accumulate in the retina of the eye and in the brain, and greater consumption of carotenoids increases their concentration in these tissues 59 . Carotenoids are known to benefit the brain because of their antioxidant properties. The brain is particularly vulnerable to oxidative stress due to its high lipid concentrations and high energy requirements 60 .
Vitamin E and choline were identified as important nutrients that promote cognitive and brain health in the Delayed Brain Aging phenotype. Multiple studies, including RCTs, have shown that high concentrations of Vitamin E in plasma are associated with better cognitive performance in healthy populations, aging populations, and Alzheimer disease patients 56 , 61 . Vitamin E’s efficacy in mitigating cognitive decline is likely through its antioxidant properties and its ability to aid in the transporting of fatty acids 62 . A recent RCT demonstrated that supplementation of Vitamin E, along with ω-3 fatty acids and carotenoids, improves performance on tests of working memory 57 . These findings are consistent with the results of the present study, which observed higher scores on tests of intelligence and memory within the Delayed Brain Aging phenotype. Notably, intelligence and memory are supported by multiple cortical regions (e.g., prefrontal, cingulate, and parietal cortices) and networks (e.g., frontoparietal network, the default mode network, and the salience network) 63 . Within the Delayed Brain Aging phenotype, we observed that these regions and networks demonstrated superior performance compared to the Accelerated Brain Aging phenotype based on measures of cortical volume and functional brain network efficiency, respectively. Excellent dietary sources of Vitamin E include nuts, seeds, and vegetable oils while significant amounts also come from green leafy vegetables and fortified cereals.
Choline, an essential B-vitamin-like nutrient, is also in the nutrient profile of Delayed Brain Aging. Choline plays at least two critical functions for cognitive and brain health: it is a necessary precursor for phosphatidylcholine, the predominant lipid in cell membranes and it is required for the synthesis and release of acetylcholine, a critical neurotransmitter 64 . Furthermore, brain white matter tracts and brain volume, which are enhanced in the Delayed Brain Aging phenotype, critically depend on choline for their cellular structure and integrity. Choline benefits both executive function and memory 15 , 64 . Excellent dietary sources of choline include animal-based proteins such as meat, poultry, fish, and eggs, while cruciferous vegetables and certain beans are also rich in choline.
Overall, there is strong evidence to support the nutrient profile underlying the Delayed Brain Aging phenotype in promoting cognitive and brain health. Many of the biochemical pathways underlying fatty acid synthesis and metabolism are well-known; but the implications of those competing pathways for cognitive and brain health, which importantly depend on the nutrients available from the diet, are only beginning to be understood. Moreover, future research should examine the differential impact of nutrition on different brain regions and networks, as certain nutrients may be important for different regions of the brain whereas other nutrients are required by the brain globally. Applying methods from Nutritional Cognitive Neuroscience, future RCTs should systematically investigate the effects of specific nutrient profiles on the structural integrity and functional efficiency of specific cortical regions and networks (e.g., combining nutrient biomarker analysis with MRI measures of local and global brain network operations). The current results provide evidence that some metabolic pathways (e.g., the DGLA pathway compared to the AA pathway) may yield more optimal brain and cognitive outcomes. Furthermore, the observed metabolic pathways that are less optimal for cognitive and brain health often result in higher levels of inflammation. Carotenoids and vitamins identified in the current study that benefit cognitive and brain health, such as lutein, choline, and Vitamin E, require regular consumption to have their beneficial effect. Importantly, these nutrients may accumulate preferentially in certain brain regions or networks, motivating an investigation of the selectivity of nutrition for promoting the health and function of specific brain regions and cortical networks.
Limitations
While some of the nutrients observed in the present study have solid molecular mechanisms to help explain their role in cognitive and brain health, other nutrients are less well understood. Research on long-chain saturated fatty acids and MUFAs (vaccenic acid and gondoic acid) have several preliminary studies suggesting their benefits on cognitive and brain health, but more research is needed to establish the precise mechanisms by which they exert an effect. Another limitation of the present study concerns the cross-sectional study design, sample size, and Caucasian participants. The Delayed Brain Aging phenotype identifies a set of nutrients that longitudinal and randomized controlled trials should target in future studies to determine their effects on cognitive and brain aging. Other statistical tools, such as canonical correlation analysis and structural equation modeling, may also be applied to draw new insights about the associations between brain aging and nutrition. The results of the present study need to be examined in non-Caucasian participants to assess the generality of findings. Moreover, while the current study examined brain health applying measures of brain structure, function, and metabolism, future research should also seek to understand how diet and nutrition effect the trajectory of brain aging within each of these measures. Additionally, the nutrient profile of Delayed Brain Aging identified in the current study does not imply they are the only nutrients that matter for brain health. Clearly, the brain needs many nutrients for healthy functioning, including amino acids, multiple B vitamins, ω-3 and ω-6 polyunsaturated fatty acids, monounsaturated fatty acids, choline, Vitamins C and D, and minerals like iron, zinc, and magnesium 65 . The nutrient profile identified in the current study differentiates Delayed Brain Aging from Accelerated Brain Aging. Finally, while the nutrient profiles discovered here suggest a basis for future testing of dietary interventions for optimal brain health, additional studies are needed to further establish and validate the present findings. It will also be important to build large-scale studies and research consortia to investigate the relationship between alternate measures of dietary intake and nutritional status, examining the reliability and validity of nutrient biomarkers, food frequency questionnaires, and their respective merits and limitations 66 , 67 .
The present study identified a specific profile of nutrients that may promote healthy brain aging, motivating further research to establish and validate these findings in the context of a randomized controlled trial. By building upon the observed findings, future research can inform the development of more effective, targeted dietary interventions that apply methods in Nutritional Cognitive Neuroscience. We believe this approach holds promise for the development of dietary strategies to support cognitive function and brain health in the aging population.
This cross-sectional study enrolled 100 healthy elderly adults from the Illinois Brain Aging Study cohort, a sample of community-dwelling Caucasian men and women aged 65–75 years. Participants were neurologically healthy and did not have evidence of cognitive impairment, as determined by a score of lower than 26 on the Mini-Mental State Examination 68 . Participants with mild cognitive impairment, dementia, a psychiatric illness within the last three years, a stroke within the past twelve months, cancer in the last three years, an inability to complete study activities, prior involvement in cognitive training or dietary intervention studies, or contraindications for magnetic resonance imaging (MRI) were excluded. All participants were right-handed with normal, or corrected to normal, vision.
Standard protocol approval and patient consent
In accordance with the University of Illinois and Carle Foundation Hospital Institutional Review Boards, informed consent was obtained from all participants in this study.
Nutrient biomarker acquisition and analysis
Fasting plasma was collected from each participant between 7:00 AM and 12:00 noon Central Time. Nutrient biomarkers were assayed, comprising three general classes of nutrients: fatty acids, carotenoids, and vitamins. Ethylenediaminetetraacetic acid (EDTA) plasma carotenoids and tocopherols were analyzed by high-performance liquid chromatography with a photodiode array detector (HPLC-PDA) using UV detection 69 . Plasma lipids were measured with gas chromatography using flame ionization and peaks of interest were identified by comparison to authentic fatty acid standards 70 . Vitamins were measured by a chemiluminescent immunometric assay or after extraction by radioimmunoassay 71 , 72 .
MRI data acquisition and processing
All data were collected on a Siemens Magnetom 3T Trio scanner using a 32-channel head coil in the MRI Laboratory of the Beckman Institute Biomedical Imaging Center at the University of Illinois.
MRI data acquisition
A high-resolution multi-echo T1-weighted magnetization prepared gradient-echo structural image was acquired for each participant (0.9 mm isotropic, TR: 1900 ms, TI: 900 ms, TE = 2.32 ms, with GRAPPA and an acceleration factor of 2). The functional neuroimaging data were acquired using an accelerated gradient-echo echoplanar imaging sequence sensitive to blood oxygenation level dependent (BOLD) contrast (2.5 × 2.5 × 3.0 mm voxel size, 38 slices with 10% slice gap, TR = 2000 ms, TE = 25 ms, FOV = 230 mm, 90° flip angle, 7 min acquisition time). During the resting-state fMRI scan, participants were shown a white crosshair on a black background viewed on an LCD monitor through a head coil-mounted mirror. Participants were instructed to lie still, focus on the visually presented crosshair, and to keep their eyes open 73 .
MRI data preprocessing
All MRI data processing was performed using FSL tools available in Functional Magnetic Resonance Imaging of the Brain (FMRIB) Software Library version 5.0. The high-resolution T1 Magnetization-Prepared Rapid Gradient-Echo (MPRAGE) was extracted using the Brain Extraction Tool 74 . FMRIB’s Automated Segmentation Tool 75 was applied to delineate gray matter, white matter, and cerebral spinal fluid (CSF) voxels. The resting-state fMRI data were pre-processed using the FSL FMRI Preprocessing and Model-Based Analysis (FEAT) analysis tool 76 , 77 . Pre-processing entailed: slice timing correction, motion correction, spatial smoothing (3 mm full width at half maximum kernel), nuisance signal regression (described below), standard fMRI temporal bandpass filtering (0.009–0.1 Hz, linear registration of functional images to structural images, and non-linear registration of structural images to the MNI152 brain template (2 mm isotropic voxel resolution).
Nuisance variables were modeled via General Linear Modeling (GLM) analyses to remove spurious correlations, noise introduced by head motion, and variables of no interest. These included head motion correction parameters (using the extended 12 motion parameters estimated in FEAT preprocessing), modeling of individual volume motion outliers estimated using DVARS (outliers flagged using the boxplot cutoff 1.5 × interquartile range 76 ), and averaging of mean white matter and cerebrospinal fluid signals across all voxels identified from the segmentation of the high resolution MPRAGE. The fully preprocessed resting-state fMRI data comprised the residual obtained from fitting these nuisance variables in the GLM framework. The residuals were transformed into normalized MNI152 space and re-sampled to 4 mm isotropic voxels to reduce computational complexity in post data processing for network analysis.
Brain volumetrics
Cortical reconstruction was performed with the Freesurfer image analysis software 78 . For this analysis, all the cortical gray matter volumes provided by the Freesurfer parcellation were examined. This included 68 regions throughout the frontal, parietal, temporal, and occipital lobes. Volumetric measures were adjusted for intracranial volume and sex using a regression model. The adjusted values were then used in further statistical analyses.
Volumetric analysis was performed on data from a 3D high-resolution (0.9 mm isotropic) T1-weighted scan using MPRAGE acquisition. Cortical reconstruction was performed with the Freesurfer image analysis suite, which is documented and freely available for download online ( http://surfer.nmr.mgh . harvard.edu/ ). All cortical reconstructions were manually checked for accuracy, as recommended by the software developers. The volumetric analyses focused on gray matter volume in the temporal cortex provided by Freesurfer parcellation. Regions of interest included the superior temporal cortex, middle temporal cortex, inferior temporal cortex, banks of the superior temporal sulcus, fusiform cortex, transverse temporal cortex, entorhinal cortex, temporal pole, and parahippocampal cortex.
Diffusion tractography imaging (DTI)
Whole brain diffusion tensor imaging was acquired with the following parameters: FOV = 240 × 240 mm; 72 slices, slice thickness = 2 mm; TE = 98 ms; TR = 10,000 ms; in-plane resolution = 1.875 × 1.875 mm; diffusion encoding directions = 30; b = 0 s/mm 2 and 1000 s/mm 2 . Data were processed using the University of Oxford’s Center for FMRIB Software Library (FSL) release 5.0 79 diffusion toolbox 80 , 81 . Eddy current correction was accomplished using the eddy correction tool and a diffusion tensor model was fit in each voxel using the DTIFIT tool, which generates fractional anisotropy (FA) values in every voxel. FA images were further processed using the FSL tract-based spatial statistics 82 toolbox, which projects each subjects’ FA data onto a mean white matter skeleton, representing the white-matter tracts common to all subjects. Mean FA within the white matter skeleton for specific regions of interest were calculated for each subject using the JHU ICBM DTI-81 atlas 83 .
Graph theory metrics of brain efficiency
The efficiency of brain network function was examined by investigating the small-world organization 84 of seven well-established intrinsic connectivity networks of the brain 85 . A small-word organization represents the optimal balance of local and global network efficiency, providing a parsimonious neural architecture that supports high local clustering (local efficiency) and short average path length (global efficiency). The procedure for computing small-world propensity is presented below.
First, the mean fMRI BOLD time series was extracted from subjects’ gray matter voxels using the Craddock parcellated brain atlas as a mask 86 . This parcellation of 200 regions provided whole-brain coverage and sufficiently high spatial resolution for conducting network analysis. A subject-wise functional connectivity matrix reflecting pairwise Pearson correlations between the mean BOLD time series signals obtained from nodes defined by the Craddock atlas was then computed and Fisher’s Z-transformed to achieve normality. These were standardized to Z-scores through multiplication with their standard deviation approximated as σ = 1/√( n − 3), where n is the number of time points corresponding to the BOLD signal 87 . A Bonferroni-corrected statistical Z-threshold was applied to identify significant positive correlations ( p < 0.05) within each subject’s whole-brain functional connectivity matrix derived from Craddock’s 800 parcellation atlas 88 , 89 . The thresholded Z-scores were rescaled to represent connection weights ranging from 0 to 1. Based on these positive connection weights, weighted connectivity matrices representing functional connectivity between nodes representative of seven intrinsic connectivity networks were obtained for each subject. The seven intrinsic connectivity network maps—visual, somatosensory, limbic, default mode, dorsal attention, ventral attention and frontoparietal—are at https://surfer.nmr.mgh.harvard.edu/fswiki/CorticalParcellation_Yeo2011 .
We then examined small-world propensity within the rescaled connectivity matrices derived for each of the seven intrinsic connectivity networks. Small world propensity Φ is calculated as the fractional deviation between a network’s clustering coefficient, C obs , and characteristic path length, L obs , from both lattice ( C latt , L latt ) and random ( C rand , L rand ) networks constructed with the same number of nodes and the same degree distribution:
The ratios Δ C and Δ L represent the fractional deviation of the metric ( C obs or L obs ) from its respective null model (a lattice or random network).
Magnetic resonance spectroscopy (MRS)
Metabolite concentration from MRS was determined using the procedure in ref. 90 . The anatomical scan was used to position a single voxel spectroscopy (SVS) scan in the parietal cortex extending into posterior cingulate cortex (voxel size: (20 mm), TR: 3000 ms, TE: 30 ms, 40 averages, BW: 2000 Hz, vector size: 1024). The voxel straddled the midline, including equal portions of the right and left hemispheres. Weak water suppression was employed, and six regional saturation bands were placed around the voxel to reduce contamination from subcutaneous fat. An additional scan was performed without water suppression to aid with quantification. Immediately following the spectroscopy acquisition, a T2-weighted overlay scan was performed with the same center location and orientation as the spectroscopy scan (TR = 5000 ms, TE = 84 ms, slice thickness 2 mm with 0.5 mm of spacing, FOV: 240 × 240 mm, 128 × 128 matrix size, GRAPPA acceleration factor: 2, 35 slices).
Metabolite quantitation was performed using tissue water as a reference. Water-scaled spectra were analyzed using LCModel software (Version 6.3-1H). No correction was performed to account for relaxation of metabolite signal. Because NAA and NAAG are difficult to differentiate, here we analyze the combined concentration of NAA + NAAG, labeled herein as NAAt with a peak appearing at 2.02 ppm.
Accurate water scaling requires corrections for the tissue composition of the voxel. Using the high-resolution structural scan, we calculated the volume fractions of gray matter (GM), white matter (WM), and CSF within each voxel using Matlab scripts (MathWorks, Natick, MA) that called functions from SPM8 (Wellcome Trust Centre for Neuroimaging). First, we segmented the MPRAGE using SPM8 to obtain tissue probability maps of GM, WM and CSF. We then created a mask in the space of the T2 overlay corresponding to the location of the spectroscopy scan. This mask has the same center and orientation as the T2 overlay but higher resolution (0.5 × 0.5 × 0.5 mm). We then registered the MPRAGE to the T2 overlay. The rotations and translations required for the registration were then applied to the tissue probability masks. We resliced the tissue probability maps into the space of the mask, and used the mask to calculate the volume fractions of GM, WM, and CSF within the volume of the spectroscopy voxel. These tissue fractions were later used to statistically correct NAAt for tissue volume-fraction dependencies.
Brain age (BA)
BA was derived using Brain-Age Regression Analysis and Computation Utility Software, or BARACUS, using T1-weighted structural images 33 , 91 .
Cognitive assessments
Neuropsychological tests investigating multiple facets of memory, executive function, and intelligence were administered. Our battery included the Wechsler Adult Intelligence Scale (WAIS 92 ), the trail-making test from the Delis-Kaplan Executive Function System (DKEFS 93 ), and the Wechsler Memory Systems (WMS 94 ).
Memory was measured by the Wechsler Memory Scale—Fourth Edition (WMS-IV) Older Adult Battery 94 . This assessment measured memory by way of four indices: Auditory Memory Index, Visual Memory Index, Immediate Memory Index, and Delayed Memory Index. The Auditory Memory Index indicates a participant’s ability to remember orally presented information. The Visual Memory Index indicates a participant’s ability to remember visually presented information. The Immediate Memory Index indicates a participant’s ability to recall visually and orally presented information immediately after it is presented. The Delayed Memory Index indicates a participant’s ability to recall and recognize visually- and orally-presented information after a 20 to 30-min delay. Participants’ raw scores on each subtest were converted to normalized scaled scores and subsequently combined into indices. Z-scores for each index were calculated and then averaged to create a composite memory score 95 .
Executive function
Executive functions were measured by the Delis–Kaplan Executive Function System (D–KEFS) Trail Making Test 93 . This assessment yields a measure of the executive functions that can be isolated from underlying skills, including visual scanning, number sequencing, letter sequencing, and motor speed. In this task, participants alternate between multiple task goals (either number or letter sequencing), which elicits a specific component of the executive functions known as cognitive flexibility. The reported results from the D-KEFS Trail Making Test assess cognitive flexibility while controlling for number and letter sequencing trials and therefore provide a measure of cognitive flexibility that is not confounded by underlying cognitive abilities (i.e., number and letter sequencing) required by the task.
Intelligence
General intelligence was measured by the Wechsler Abbreviated Scale of Intelligence– second edition (WASI-II 92 ). Per the scoring guidelines, this assessment measured general intelligence by way of an estimated intelligence quotient score, derived from fluid and crystallized test scores which, in turn, were derived from four subtests: a block design subtest, a matrix reasoning subtest, a vocabulary subtest, and a similarities subtest. In the block design subtest, participants were asked to reproduce pictured designs using specifically designed blocks as quickly and accurately as possible. In the matrix reasoning subtest, participants were asked to complete a matrix or serial reasoning problem by selecting the missing section from five response items. In the vocabulary subtest, participants were asked to verbally define vocabulary words (i.e., What does lamp mean?) that became progressively more challenging. In the similarities subtest, participants were asked to relate pairs of concepts (i.e., How are a cow and bear alike?) that became progressively more challenging. Per scoring guidelines, subjects’ raw scores were converted to standardized scores and combined into an estimated intelligence quotient score, which provided a measure of general intelligence.
Demographics, anthropometrics, and fitness
Demographics, including sex, education, and income, were collected via questionnaire responses provided by the participants. Anthropometric measures of weight, height, hip, and waist circumference were assessed by the study coordinator at the first study visit. Several measures of physical fitness were also collected or determined. Body Mass Index (BMI) was calculated from measured height and weight. Resting Heart Rate (RHR) was measured by the study coordinator during the participant’s first visit to the lab. Physical activity and the metabolic equivalent of VO 2 were assessed via a published questionnaire and required BMI and RHR as inputs 96 .
Analysis overview
First, individual differences in brain health were determined from the multimodal neuroimaging features using hierarchical clustering. Individuals with similar brain health were grouped together. Second, brain aging trajectories were computed for everyone and for each brain health group. Third, we examined cognitive aging differences within each brain health group. Fourth, a nutrient profile for the healthy brain and cognitive aging group was determined. Finally, lifestyle factors other than diet were examined to determine their role in brain and cognitive aging.
Statistical analyses
All statistical analyses were conducted in R Studio Version 2022.2.3.492 97 using the R statistical computing software environment Version 4.0.3 98 . Covariates with the weakest inter-correlations associated with age-related cognitive decline (age, gender, education, income, and Body Mass Index) were included as predictors in a separate regression model for each outcome measure of nutrition, brain, and cognition. Residualization was performed using the Frisch-Waugh-Lowell theorem. The net result of residualization is to remove the potential effects of covariates on the outcome. The residuals from each model were normally transformed using Tukey’s Ladder of Powers 99 and then [0,1] scaled. This process also had the effect of transforming outlier values to a normal range and resulting in a range of 0 to 1 for all variables. Hierarchical clustering, using the complete linkage method, was used to cluster individuals according to similarity of their brain features and it is not sensitive to multicollinearity. T tests of the mean were used to assess the magnitude and significance of differences between phenotypes.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The individual de-identified participant data can be made available upon request.
Code availability
Codes used for this study are available upon reasonable request from the authors.
Zamroziewicz, M. & Barbey, A. Nutritional cognitive neuroscience: innovations for healthy brain aging. Front. Neurosci. 10 , 240 (2016).
Article PubMed PubMed Central Google Scholar
Jensen, D., Leoni, V., Klein-Flügge, M., Ebmeier, K. & Suri, S. Associations of dietary markers with brain volume and connectivity: a systematic review of MRI studies. Ageing Res. Rev. 70 , 101360 (2021).
Article CAS PubMed Google Scholar
Tracey, T., Steyn, F., Wolvetang, E. & Ngo, S. Neuronal lipid metabolism: multiple pathways driving functional outcomes in health and disease. Front. Mol. Neurosci. 11 , 10 (2018).
Köbe, T., Witte, A., Schnelle, A., Lesemann, A. & Fabian, S. Combined omega-3 fatty acids, aerobic exercise and cognitive stimulation prevents decline in gray matter volume of the frontal, parietal and cingulate cortex in patients with mild cognitive impairment. NeuroImage 131 , 226–238 (2016).
Article PubMed Google Scholar
Witte, A., Kerti, L., Hermannstädter, H., Fiebach, J. & Schreiber, S. Long-chain omega-3 fatty acids improve brain function and structure in older adults. Cereb. Cortex 24 , 3059–3068 (2014).
Jernerén, F., Elshorbagy, A., Oulhaj, A., Smith, S. & Refsum, H. Brain atrophy in cognitively impaired elderly: the importance of long-chain ω-3 fatty acids and B vitamin status in a randomized controlled trial. Am. J. Clin. Nutr. 102 , 215–221 (2015).
Sueyasu, T., Yasumoto, K., Tokuda, H., Kaneda, Y. & Obata, H. Effects of long-chain polyunsaturated fatty acids in combination with lutein and zeaxanthin on episodic memory in healthy older adults. Nutrients 15 , 2825 (2023).
Article CAS PubMed PubMed Central Google Scholar
Zwilling, C., Strang, A., Anderson, E., Jurcsisn, J. & Johnson, E. Enhanced physical and cognitive performance in active duty Airmen: evidence from a randomized multimodal physical fitness and nutritional intervention. Nat. Sci. Rep. 10 , 17826 (2020).
CAS Google Scholar
Mazereeuw, G., Lanctôt, K., Chau, S., Swardfager, W. & Herrmann, N. Effects of ω-3 fatty acids on cognitive performance: a meta-analysis. Neurobiol. Aging 33 , e17–e29 (2012).
Article Google Scholar
Franzoni, F. et al. Oxidative stress and cognitive decline: the neuroprotective role of natural antioxidants. Front. Neurosci. 15 , 729–757 (2021).
Terracina, S., Petrella, C., Francati, S., Lucarelli, M. & Barbato, C. Antioxidant intervention to improve cognition in the aging brain: the example of hydroxytyrosol and resveratrol. Int. J. Mol. Sci. 23 , 156–174 (2022).
Lindbergh, C., Lv, J., Zhao, Y., Mewborn, C. & Puente, A. The effects of lutein and zeaxanthin on resting state functional connectivity in older Caucasian adults: a randomized controlled trial. Brain Imaging Behav. 14 , 668–681 (2020).
Sloan, R., Wall, M. & Yeung, L. Insights into the role of diet and dietary flavanols in cognitive aging: results of a randomized controlled trial. Sci. Rep. 11 , 3837 (2021).
Yeh, T., Yuan, C., Ascherio, A., Rosner, B. & Willett, W. Long-term dietary flavonoid intake and subjective cognitive decline in US men and women. Neurology 97 , e1041–e1056 (2021).
CAS PubMed PubMed Central Google Scholar
Nakazaki, E., Mah, E., Sanoshy, K., Citrolo, D. & Watanabe, F. Citicoline and memory function in healthy older adults: a randomized, double-blind, placebo-controlled clinical trial. J. Nutr. 151 , 2153–2160 (2021).
López-Otín, C., Blasco, M., Partridge, L., Serrano, M. & Kroemer, G. The hallmarks of aging. Cell 153 , 1194–1217 (2013).
Kirkwood, T. Understanding the odd science of aging. Cell 120 , 437–447 (2005).
Kirkwood, T. B. A systematic look at an old problem. Nature 451 , 644–647 (2008).
Wrigglesworth, J., Ward, P., Harding, I., Nilaweera, D. & Wu, Z. Factors associated with brain ageing—a systematic review. BMC Neurolol. 21 , 312 (2021).
Bethlehem, R., Seidlitz, J., White, S. & Vogel, J. Brain charts for the human lifespan. Nature 604 , 525–533 (2022).
Harada, C., Natelson Love, M. & Triebel, K. Normal cognitive aging. Clin. Geriatr. Med. 29 , 737–752 (2013).
Raz, N. & Rodrigue, K. Differential aging of the brain: patterns, cognitive correlates and modifiers. Neurosci. Biobehav. Rev. 30 , 730–748 (2006).
Sexton, C., Walhovd, K., Storsve, A., Tamnes, C. & Westlye, L. Accelerated changes in white matter microstructure during aging: a longitudinal diffusion tensor imaging study. J. Neurosci. 34 , 15425–15436 (2014).
Lockhart, S. & DeCarli, C. Structural imaging measures of brain aging. Neuropsychol. Rev. 24 , 271–289 (2014).
Fjell, A., McEvoy, L., Holland, D., Dale, A. & Walhovd, K. Alzheimer’s Disease Neuroimaging Initiative Brain changes in older adults at very low risk for Alzheimer’s disease. J. Neurosci. 33 , 8237–8242 (2013).
Park, D. & Reuter-Lorenz, P. The adaptive brain: aging and neurocognitive scaffolding. Annu. Rev. Psychol. 60 , 173–196 (2009).
Salthouse, T. What and when of cognitive aging. Curr. Direc. Psychol. Sci. 13 , 140–144 (2004).
IJ, D., Corley, J., Gow, A., Harris, S. & Houlihan, L. Age-associated cognitive decline. Br. Med. Bull. 92 , 135–152 (2009).
Craik, F. I., Salthouse, T. A. The Handbook of Aging and Cogntion, 1st edn (Psychology Press, New York City, 2008).
Mattay, V., Goldberg, T., Sambataro, F. & Weinberger, D. Neurobiology of cognitive aging: insights from imaging genetics. Biol. Psychol. 79 , 9–22 (2008).
Nyberg, L. & Pudas, S. Successful memory aging. Annu. Rev. Psychol. 70 , 219–243 (2019).
Franke, K., Ziegler, G., Klöppel, S. & Gaser, C. Alzheimer’s Disease Neuroimaging Initiative Estimating the age of healthy subjects from T1-weighted MRI scans using kernel methods: exploring the influence of various parameters. Neuroimage 50 , 883–892 (2010).
Liem, F. Predicting brain-age from multimodal imaging data captures cognitive impairment. Neuroimage 148 , 179–188 (2017).
Franke, K. & Gaser, C. Ten years of brainAGE as a neuroimaging biomarker of brain aging: what insights have we gained? Front. Neurol 10 , 789 (2019).
Talukdar, T., Zwilling, C. & Barbey, A. Integrating nutrient biomarkers, cognitive function, and structural MRI data to build multivariate phenotypes of healthy aging. J. Nutr. 153 , 1338–1346 (2023).
Zamroziewicz, M., Paul, E. J., Zwilling, C. E. & Barbey, A. K. Determinants of fluid intelligence in healthy aging: omega-3 polyunsaturated fatty acid status and frontoparietal cortex structure. Nutr. Neurosci. 21 , 570–579 (2018).
Zamroziewicz, M., Paul, E., Zwilling, C. & Barbey, A. Predictors of memory in healthy aging: polyunsaturated fatty acid balance and fornix white matter integrity. Aging Dis. 8 , 372–383 (2017).
Galea, I. The blood-brain barrier in systemic infection and inflammation. Cell Mol. Immunol. 18 , 2489–2501 (2021).
Sankowski, R., Mader, S. & Valdés-Ferrer, S. Systemic inflammation and the brain: novel roles of genetic, molecular, and environmental cues as drivers of neurodegeneration. Front. Cell Neurosci. 9 , 29 (2015).
Sun, Y., Koyama, Y. & Shimada, S. Inflammation from peripheral organs to the brain: how does systemic inflammation cause neuroinflammation? Front. Aging Neurosci. 14 , 903455 (2022).
Sartori, A., Vance, D., Slater, L. & Crowe, M. The impact of inflammation on cognitive function in older adults: implications for healthcare practice and research. J. Neurosci. Nurs. 44 , 206–217 (2012).
Sæther, L., Ueland, T., Haatveit, B., Maglanoc, L. & Szabo, A. Inflammation and cognition in severe mental illness: patterns of covariation and subgroups. Mol. Psychiatry 28 , 1284–1292 (2023).
Kipinoinen, T., Toppala, S., Rinne, J., Viitanen, M. & Jula, A. Association of midlife inflammatory markers with cognitive performance at 10-year follow-up. Neurology 99 , e2294–e2302 (2022).
Soberman, R. & Christmas, P. The organization and consequences of eicosanoid signaling. J. Clin. Investig. 111 , 1107–1113 (2003).
Goyens, P., Spilker, M., Zock, P., Katan, M. & Mensink, R. Conversion of α-linolenic acid in humans is influenced by the absolute amounts of α-linolenic acid and linoleic acid in the diet and not by their ratio. Am. J. Clin. Nutr. 84 , 44–53 (2006).
Chen, Y., Qiu, X. & Yang, J. Comparing the in vitro antitumor, antioxidant and anti-inflammatory activities between two new very long-chain polyunsaturated fatty acids, docosadienoic acid (DDA) and docosatrienoic acid (DTA), and docosahexaenoic acid (DHA). Nutr. Cancer 73 , 1697–1707 (2021).
Henry, G., Momin, R., Nair, M. & Dewitt, D. Antioxidant and cyclooxygenase activities of fatty acids found in food. J. Agric. Food Chem. 50 , 2231–2234 (2002).
Caballero, B. Ed., Encyclopedia of Human Nutrition in Health Effects of Saturated Fatty Acids , 215–219 (Academic Press, 2013).
Lemaitre, R. & King, I. Very long-chain saturated fatty acids and diabetes and cardiovascular disease. Curr. Opin. Lipidol. 33 , 76–82 (2022).
Li, D., Misialek, J., Jing, M., Tsai, M. & Eckfeldt, J. Plasma phospholipid very-long-chain SFAs in midlife and 20-year cognitive change in the Atherosclerosis Risk in Communities (ARIC): a cohort study. Am. J. Clin. Nutr. 111 , 1252–1258 (2020).
Zamroziewicz, M., Talukdar, M., Zwilling, C. & Barbey, A. Nutritional status, brain network organization, and general intelligence. NeuroImage 161 , 241–250 (2017).
Burdge, G., Tricon, S., Morgan, R., Kliem, K. & Childs, C. Incorporation of cis-9, trans-11 conjugated linoleic acid and vaccenic acid (trans-11 18:1) into plasma and leucocyte lipids in healthy men consuming dairy products naturally enriched in these fatty acids. Br. J. Nutr. 94 , 237–243 (2005).
Field, C., Blewett, H., Proctor, S. & Vine, D. Human health benefits of vaccenic acid. Appl. Physiol. Nutr. Metab. 34 , 979–991 (2009).
Murru, E., Carta, G., Manca, C., Sogos, V. & Pistis, M. Conjugated linoleic acid and brain metabolism: a possible anti-neuroinflammatory role mediated by PPARα activation. Front. Pharmacol. 11 , 587140 (2021).
Fan, Y., Meng, H., Hu, G. & Li, F. Iosynthesis of nervonic acid and perspectives for its production by microalgae and other microorganisms. Appl. Microbiol. Biotechnol. 102 , 3027–3035 (2018).
Zwilling, C., Talukdar, T., Zamroziewicz, M. & Barbey, A. Nutrient biomarker patterns, cognitive function, and fMRI measures of network efficiency in the aging brain. NeuroImage 188 , 239–251 (2019).
Power, R., Nolan, J., Prado-Cabrero, A., Roche, W. & Coen, R. Omega-3 fatty acid, carotenoid and vitamin E supplementation improves working memory in older adults: A randomised clinical trial. Clin Nutr 41 , 405–414 (2022).
Ceravolo, S., Hammond, B., Oliver, W., Clementz, B. & Miller, L. Dietary carotenoids lutein and zeaxanthin change brain activation in older adult participants: a randomized, double-masked, placebo-controlled trial. Mol. Nutr. Food Res. 63 , 15 (2019).
Tanprasertsuk, J., Scott, T., Barbey, A., Barger, K. & Wang, X. Carotenoid-rich brain nutrient pattern is positively correlated with higher cognition and lower depression in the oldest old with no dementia. Front. Nutr. 8 , 704691 (2021).
Lee, K., Cha, M. & Lee, B. Neuroprotective effect of antioxidants in the brain. Int. J. Mol. Sci. 21 , 7152 (2020).
La Fata, G., Weber, P. & Mohajeri, M. Effects of vitamin E on cognitive performance during ageing and in Alzheimer’s disease. Nutrients 6 , 5453–5472 (2014).
Lee, P. & Ulatowski, L. Vitamin E: mechanism of transport and regulation in the CNS. IUBMB Life 71 , 424–429 (2019).
Colom, R., Karama, S., Jung, R. & Haier, R. Human intelligence and brain networks. Front. Psychol. 12 , 489–501 (2010).
Google Scholar
Zamroziewicz, M., Zwilling, C. & Barbey, A. Inferior prefrontal cortex mediates the relationship between phosphatidylcholine and executive functions in healthy, older adults. Front. Aging Neurosci. 8 , 226 (2016).
PubMed PubMed Central Google Scholar
Gómez-Pinilla, F. Brain foods: the effects of nutrients on brain function. Nat. Rev. Neurosci. 9 , 568–578 (2008).
Bowman, G., Shannon, J., Ho, E., Traber, M. & Frei, B. Reliability and validity of food frequency questionnaire and nutrient biomarkers in elders with and without mild cognitive impairment. Alzheimer Dis. Assoc. Disord. 25 , 49–57 (2011).
Fraser, G., Jaceldo-Siegl, K., Henning, S., Fan, J. & Knutsen, S. Biomarkers of dietary intake are correlated with corresponding measures from repeated dietary recalls and food-frequency questionnaires in the adventist health study-2. J. Nutr. 146 , 586–594 (2016).
Folstein, M., Folstein, S. & McHugh, P. Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12 , 189–198 (1975).
Zhimin, X. & Howard, L. R. Analysis of Antioxidant‐Rich Phytochemicals (John Wiley & Sons Ltd, 2012).
Folch, J., Lees, M. & Stanley, G. A simple method for the isolation and purification of total lipids from animal tissues. J. Biol. Chem. 226 , 497–509 (1957).
Babson, A. The Cirrus Immulite automated immunoassay system. J. Clin. Immunoassay 14 , 83–88 (1991).
Hart, G., Furniss, J., Laurie, D. & Durham, S. Measurement of vitamin D status: Background, clinical use, and methodologies. Clin Lab 52 , 335–343 (2006).
CAS PubMed Google Scholar
Van Dijk, K., Hedden, T., Venkataraman, A., Evans, K. & Lazar, S. Intrinsic functional connectivity as a tool for human connectomics: theory, properties, and optimization. J. Neurophysiol. 103 , 297–321 (2010).
Smith, S. Fast robust automated brain extraction. Hum. Brain Mapp. 17 , 143–155 (2002).
Zhang, Y., Brady, M. & Smith, S. Segmentation of brain MR images through a hidden Markov random field model and the expectation-maximization algorithm. IEEE Trans. Med. Imaging 20 , 45–57 (2001).
Jenkinson, M., Beckmann, C., Behrens, T., Woolrich, M. & Smith, S. Fsl. Neuroimage 62 , 782–790 (2012).
Satterthwaite, T., Wolf, D. & Loughead, J. Impact of in-scanner head motion on multiple measures of functional connectivity: relevance for studies of neurodevelopment in youth. Neuroimage 60 , 623–632 (2012).
Reuter, M., Rosas, H. D. & Fischl, B. Highly accurate inverse consistent registration: a robust approach. Neuroimage 53 , 1181–1196 (2010).
Smith, S., Jenkinson, M., Woolrich, M., Beckmann, C. & Behrens, T. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage 23 , S208–S219 (2004).
Behrens, T. E. et al. Characterization and propagation of uncertainty in diffusion-weighted MR imaging. Magn. Reson. Med. 50 , 1077–1088 (2003).
Behrens, T., Berg, H., Jbabdi, S., Rushworth, M. & Woolrich, M. Probabilistic diffusion tractography with multiple fibre orientations: what can we gain? Neuroimage 34 , 144–155 (2007).
Smith, S., Jenkinson, M., Johansen-Berg, H., Rueckert, D. & Nichols, T. Tract-based spatial statistics: Voxelwise analysis of multi-subject diffusion data. Neuroimage 31 , 1487–1505 (2006).
Oishi, K., Zilles, K., Amunts, K., Faria, A. & Jiang, H. Human brain white matter atlas: identification and assignment of common anatomical structures in superficial white matter. Neuroimage 43 , 447–457 (2008).
Muldoon, S., Bridgeford, E. & Bassett, D. Small-world propensity and weighted brain networks. Sci. Rep. 6 , 22057 (2016).
Yeo, B., Krienen, F. & Sepulcre, J. The organization of the human cerebral cortex is estimated by intrinsic functional connectivity. J. Neurophysiol. 106 , 1125–1165 (2011).
Craddock, R., James, G., Holtzheimer, P., Hu, X. & Mayberg, H. A whole brain fMRI atlas generated via spatially constrained spectral clustering. Hum. Brain Mapp. 33 , 1914–1928 (2012).
Ree, M. Correlation and regression: applications for industrial organizational psychology and management. Organ. Res. Methods 5 , 200–201 (2002).
Fox, M., Zhang, D., Snyder, A. & Raichle, M. The global signal and observed anticorrelated resting state brain networks. J. Neurophysiol. 101 , 3270–3283 (2009).
Murphy, K., Birn, R., Handwerker, D., Jones, T. & Bandettini, P. The impact of global signal regression on resting state correlations: are anti-correlated networks introduced?. Neuroimage 44 , 893–905 (2009).
Paul, E., Larsen, R. & Barbey, A. Dissociable brain biomarkers of fluid intelligence. NeuroImage 137 , 201–211 (2016).
Fischl, B. FreeSurfer. NeuroImage 62 , 774–781 (2012).
Wechsler, D. Wechsler Abbreviated Scale of Intelligence (Psychological Corporation, 1999).
Delis, D. C., Kaplan, E. & Kramer, J. H. Delis-Kaplan Executive Function System (D–KEFS) (The Psychological Corporation, San Antonio, 2001).
Wechsler, D. WMS-IV: Wechsler Memory Scale-fourth Edition (Pearson, San Antonio, 2009).
Siedlecki, K., Honig, L. & Stern, Y. Exploring the structure of a neuropsychological battery across healthy elders and those with questionable dementia and Alzheimer’s disease. Neuropsychology 22 , 400–411 (2009).
Jurca, R., Jackson, A., LaMonte, M., Morrow, J. J. & Blair, S. Assessing cardiorespiratory fitness without performing exercise testing. Am. J. Prev. Med. 29 , 185–193 (2005).
CoreTeam, R Studio: Integrated Development Environment for R (RStudio, PBC, Boston, 2022).
Team, R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, Vienna, 2020).
Salvatore, M. rcompanion: Functions to Support Extension Education Program Evaluation , R package version 2.3.25, (2020).
Download references
Acknowledgements
This work was supported by a grant from Abbott Nutrition through the Center for Nutrition, Learning, and Memory at the University of Illinois (ANGC1205; PI: Barbey). The interdisciplinary community and supportive environment within the Decision Neuroscience Laboratory ( https://www.decisionneurosciencelab.org ) proved invaluable in completing this research.
Author information
Authors and affiliations.
Department of Psychology, University of Illinois, Urbana, IL, USA
Christopher E. Zwilling & Aron K. Barbey
Beckman Institute for Advanced Science and Technology, University of Illinois, Urbana, IL, USA
Decision Neuroscience Laboratory, University of Nebraska-Lincoln, Lincoln, NE, USA
Jisheng Wu & Aron K. Barbey
Center for Brain, Biology, and Behavior, University of Nebraska-Lincoln, Lincoln, NE, USA
Department of Psychology, University of Nebraska-Lincoln, Lincoln, NE, USA
Department of Bioengineering, University of Illinois, Urbana, IL, USA
Aron K. Barbey
You can also search for this author in PubMed Google Scholar
Contributions
Project Conception (C.E.Z., J.W., and A.K.B.), Study Design (C.E.Z., J.W., and A.K.B.), Data Analysis (C.E.Z. and J.W.), Manuscript drafting (C.E.Z., J.W., and A.K.B.), Manuscript editing and final review (C.E.Z. and A.K.B.).
Corresponding author
Correspondence to Aron K. Barbey .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplemental information, reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Zwilling, C.E., Wu, J. & Barbey, A.K. Investigating nutrient biomarkers of healthy brain aging: a multimodal brain imaging study. npj Aging 10 , 27 (2024). https://doi.org/10.1038/s41514-024-00150-8
Download citation
Received : 18 October 2023
Accepted : 15 April 2024
Published : 21 May 2024
DOI : https://doi.org/10.1038/s41514-024-00150-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.

IMAGES
VIDEO
COMMENTS
PART THREE: THE COGNITIVE CONCEPTUALIZATION DIAGRAM (CCD) Include a completed CCD with the case write -up. PART FOUR: THE CASE CONCEPTUALIZATION SUMMARY HISTORY OF CURRENT ILLNESS, PRECIPITANTS AND LIFE STRESSORS: The first occurrence of Abe's psychiatric symptoms began 2 ½ years ago when Abe began to display mild
The following samples can be taken as basic templates for case conceptualization, in the context of Cognitive-Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and family therapy. Sample #1: Conceptualization for CBT case. This is a 35-year-old Caucasian man referred by his physician for treatment of generalized anxiety.
Beck Institute for Cognitive Behavior Therapy • One Belmont Ave, Suite 700 • Bala Cynwyd, PA 19004 • beckinstitute.org Created Date 8/26/2020 12:13:03 PM
Monson, C. M. & Shnaider, P. (2014). Treating PTSD with cognitive-behavioral therapies: Interventions that work. Washington, DC: American Psychological Association. Updated July 31, 2017. Date created: 2017. This case example explains how Jill's therapist used a cognitive intervention with a written worksheet as a starting point for engaging in ...
The CB case formulation, depicted in Figure 2, is a hypothesis that ties together, in a brief narrative or diagram, the mechanismsthat cause and maintain the client's problems,the. originsof the mechanisms, and the precipitantsthat are currently activating the mechanismsto. 4 cause the problems.
Strengths and Assets: bright, attractive, personable, cooperative, collaborative, many good social skills Treatment Plan Goals (measures): Reduce symptoms of depression and anxiety (BDI, BAI). To feel more comfortable and less pressured in relationships, less guilty. To be less dependent in relationships.
The Alternative Action Formulation is a CBT case conceptualization (formulation) worksheet. ... Case Formulation Template Download Archived Link. Recommended Reading. ... The Case of" Sonia" Through the Lens of Dialectical Behavior Therapy.Pragmatic Case Studies in Psychotherapy,10(1), 30-39. Download Primary Link Archived Link.
Psychologists in private practice (N=742) were randomly assigned to receive a research review of data from randomized controlled trials of cognitive-behavioral treatment (CBT) and medication for ...
A case formulation is a hypothesis about the psychological mechanisms that cause and maintain an individual's symptoms and problems (Kuyken et al., 2009; Persons, 2008). It's a principle-driven approach that targets mechanisms grounded in basic psychological theories—such as cognitive theory, classical and operant conditioning.
The (Traditional) Cognitive Conceptualization Diagram allows you to extract a great deal of information about clients' most central beliefs and key behavioral patterns; it helps you understand the connections
The case formulation bridges the assessment and treatment plan, and informs a clinician's treatment choices. In the Case Formulation worksheet, a client's vulnerabilities (e.g. risk factors), problems, and triggers are used to generate a single hypothesis that makes sense of their unique case. Many therapies, such as CBT, recommend ...
Case formulation is a framework used by practitioners of cognitive behavioural therapy (CBT) to identify and understand the client's problems. While the standard generic (sometimes referred to as 'nomothetic') case formulations offered by CBT manuals provide a useful starting point for working with a particular client presentation (e.g ...
Her more recent episodes related to her parents' marital problems and her academic/social difficulties at school. She was treated using cognitive-behavioral therapy (CBT). Chafey, M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response.
CASE WRITE-UP EXAMPLE PART ONE: INTAKE INFORMATION IDENTIFYING INFORMATION AT INTAKE: Age: 56 Gender Identity and Sexual Orientation: Male, heterosexual ... Beck Institute for Cognitive Behavior Therapy • One Belmont Ave, Suite 700 • Bala Cynwyd, PA 19004 • beckinstitute.org.
CBT Techniques and behavioural techniques used: The ABC Model. Identifying faulty thoughts and feelings. Identifying faulty thinking and looking at how it affects feelings and behaviour. Challenging facts and focusing on positive. Setting homework and goal and revisiting to look at progress. Relaxation techniques.
Case: History, Formulation, and Treatment Plan Your task in this assignment is to present a case study of the psychotherapy you have conducted with a patient. Your presentation should (1) place your view of the patient and the therapy in the context of key cognitive and behavioral theories (e.g., Beck's cognitive
An actual recording of a live CBT session with this client (without client's full name). Both parts of the Work Sample (Case Write -up and Recorded Therapy Session) are to be submitted at the same time according to the instructions provided. You may not use a client you submitted for supervision. Case Write-Up: Summary and Conceptualization
Offering a unique philosophical, theoretical and process-focused introduction to one of the cornerstones of CBT: assessment and case formulation. Updated and expanded to take account of the vast developments in the field of CBT since its first publication, this second edition follows a clear two part structure: - Part One introduces trainees to ...
For example, the ABC Level 4 Diploma in Therapeutic Counselling requires you to write two case studies as part of your external portfolio, to meet the following criteria: 4.2 Analyse the application of your own theoretical approach to your work with one client over a minimum of six sessions. 4.3 Evaluate the application of your own theoretical ...
Objective: In cognitive behavioural therapy (CBT), case formulation (CF) is an integral process in ensuring clinicians' work is grounded in evidence-based practice (EBP). The objective of this study was to evaluate psychologists' perceptions and self-reported applications of CBT-CF, and whether these differed according to clinician experience, training, and professional accreditation.
The criteria for BABCP CBT Practitioner Accreditation are set out in our Minimum Training Standards (MTS 2021) -. at least four of the eight training cases must be presented and formally assessed as case studies, a further three must have received close supervision. written case studies should be between 2000-4000 words (or 3-5000 if extended).
APA Template. Example Case Conceptualization and Treatment Plan for Kevin. J. Scott Branson, Ph.D., LPC, NCC. Wayne State University Example Case Conceptualization and Treatment Plan for Kevin. Kevin is a Caucasian male in his mid-30s who has been struggling with alcohol use since. he was 21 years old. Recently, Kevin lost his job, which ...
Thought Records in CBT: 7 Examples and Templates. 16 Dec 2020 by Jeremy Sutton, Ph.D. Scientifically reviewed by Gabriella Lancia, Ph.D. The idea that our thoughts determine how we feel and behave is the cornerstone of Cognitive-Behavioral Therapy (CBT). The good news is that by helping people view experiences differently and changing how they ...
This book takes you step-by-step through the Low-intensity CBT interventions, competencies and clinical procedures. ... Worksheet templates and short exercises for a patient to work through independently or a practitioner and patient to work through together are available at https: ... 14.3 Case study: Jane. 14.4 Case study: Mark 12.1 Unhelpful ...
The emerging field of Nutritional Cognitive Neuroscience aims to uncover specific foods and nutrients that promote healthy brain aging. Central to this effort is the discovery of nutrient profiles ...
With a template, all you need to do is customize the existing design and add your own content to create a stunning one-pager. You can get a head start with Visme's many pre-made, beautiful one-page designs. After selecting a template, take advantage of the graphs, diagrams, and figures available in the Visme editor. 4.