Select "Patients / Caregivers / Public" or "Researchers / Professionals" to filter your results. To further refine your search, toggle appropriate sections on or off.

What Is Cancer Research?

Home > Patients, Caregivers, and Advocates > About Cancer > What Is Cancer Research?
Cancer research transforms and saves lives.
The purpose of studying cancer is to develop safe and effective methods to prevent, detect, diagnose, treat, and, ultimately, cure the collections of diseases we call cancer. The study of cancer is called oncology.
Why Cancer Research Is Important
Cancer research is important because the better we understand these diseases, the more progress we will make toward diminishing the tremendous human and economic tolls of cancer.
Research has helped us accumulate extensive knowledge about the biological processes involved in cancer onset, growth, and spread in the body. Those discoveries have led to more effective and targeted treatments and prevention strategies.
Breakthroughs in prevention, early detection, screening, diagnosis, and treatment are often the result of research and discoveries made by scientists in a wide array of disciplines over decades and even generations. Ultimately, cancer research requires partnerships and collaborations involving researchers, clinicians, patients, and others to translate yesterday’s discoveries into today’s advances and tomorrow’s cures.
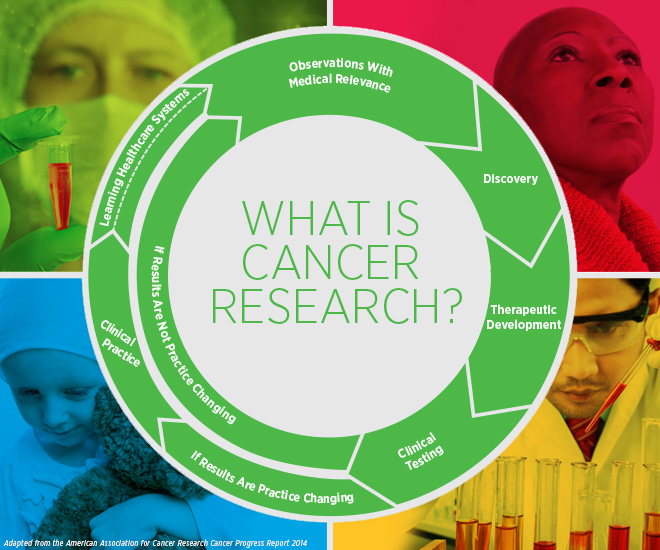
The Cancer Research Cycle
Research progress is often not linear, but cyclical and ongoing. Advances are the result of constantly building on earlier discoveries and observations.
The research cycle flows from observations with medical relevance to the patient’s bedside and back to the lab. Progress in cancer research depends on the participation of basic and population scientists, physician-scientists, and clinical cancer researchers, as well as patients, their caregivers, and health care providers. Insights from one discipline influence others, and discoveries made in one cancer can offer new ideas to better address others.
Categories of Cancer Research
Cancer research can be divided into several broad categories:
Basic Research
Basic research is the study of animals, cells, molecules, or genes to gain new knowledge about cellular and molecular changes that occur naturally or during the development of a disease. Basic research is also referred to as lab research or preclinical research.
Translational Research
Translational research seeks to accelerate the application of discoveries in the laboratory to clinical practice. This is often referred to as moving advances from bench to bedside.
Clinical Research
Clinical research involves the application of treatments and procedures in patients. Clinical cancer researchers conduct clinical trials, study a particular patient or group of patients, including their behaviors, or use materials from humans, such as blood or tissue samples, to learn about disease, how the healthy body works, or how it responds to treatment.
Population Research
Population research (also known as epidemiological research) is the study of causes and patterns of occurrence of cancer and evaluation of risk. Population scientists, also known as epidemiologists, study the patterns, causes, and effects of health and diseases in defined groups. Population research is highly collaborative and can span the spectrum from basic to clinical research.
We have made spectacular progress against cancer thanks to breakthroughs in cancer science. However, with more than 600,000 people in the United States projected to die from cancer this year, our work is not done. Get involved to ensure that the momentum continues:
- The Progression of Cancer
- Experts Forecast Cancer Research and Treatment...
- Open access
- Published: 11 October 2019
Depression and anxiety among people living with and beyond cancer: a growing clinical and research priority
- Claire L. Niedzwiedz ORCID: orcid.org/0000-0001-6133-4168 1 ,
- Lee Knifton 2 , 3 ,
- Kathryn A. Robb 1 ,
- Srinivasa Vittal Katikireddi 4 &
- Daniel J. Smith 1
BMC Cancer volume 19 , Article number: 943 ( 2019 ) Cite this article
90k Accesses
352 Citations
44 Altmetric
Metrics details
A cancer diagnosis can have a substantial impact on mental health and wellbeing. Depression and anxiety may hinder cancer treatment and recovery, as well as quality of life and survival. We argue that more research is needed to prevent and treat co-morbid depression and anxiety among people with cancer and that it requires greater clinical priority. For background and to support our argument, we synthesise existing systematic reviews relating to cancer and common mental disorders, focusing on depression and anxiety.
We searched several electronic databases for relevant reviews on cancer, depression and anxiety from 2012 to 2019. Several areas are covered: factors that may contribute to the development of common mental disorders among people with cancer; the prevalence of depression and anxiety; and potential care and treatment options. We also make several recommendations for future research. Numerous individual, psychological, social and contextual factors potentially contribute to the development of depression and anxiety among people with cancer, as well as characteristics related to the cancer and treatment received. Compared to the general population, the prevalence of depression and anxiety is often found to be higher among people with cancer, but estimates vary due to several factors, such as the treatment setting, type of cancer and time since diagnosis. Overall, there are a lack of high-quality studies into the mental health of people with cancer following treatment and among long-term survivors, particularly for the less prevalent cancer types and younger people. Studies that focus on prevention are minimal and research covering low- and middle-income populations is limited.
Research is urgently needed into the possible impacts of long-term and late effects of cancer treatment on mental health and how these may be prevented, as increasing numbers of people live with and beyond cancer.
Peer Review reports
A cancer diagnosis can have a wide-ranging impact on mental health and the prevalence of depression and anxiety among people with cancer is high [ 1 , 2 ]. Among those with no previous psychiatric history, a diagnosis of cancer is associated with heightened risk of common mental disorders, which may adversely affect cancer treatment and recovery, as well as quality of life and survival [ 3 ]. People who have previously used psychiatric services may be particularly vulnerable and at greater risk of mortality following a cancer diagnosis [ 4 ]. However, the mental health needs of people with cancer, with or without a prior psychiatric history, are often given little attention during and after cancer treatment, which is primarily focused on monitoring physical health symptoms and side effects. Advances in the earlier detection of cancer and improved cancer treatments means that people are now living longer with cancer, presenting a significant global challenge. The total number of people who are alive within 5 years of a cancer diagnosis was estimated to be 43.8 million in 2018 for 36 cancers across 185 countries [ 5 ], and in the United States alone, the number of cancer survivors is projected to rise exponentially from 15.5 million in 2016 to 26.1 million in 2040 [ 6 ].
The main objective of this article is to argue that more research is needed into the prevention, care and treatment of co-morbid depression and anxiety among people with cancer and highlight it as a growing clinical and policy priority. For background and to support our argument, we provide a current evidence review of systematic reviews relating to common mental disorders amongst people living with and beyond cancer. We cover the factors that may increase the risk of experiencing co-morbid depression and anxiety, epidemiology, and potential care and treatment options.
We searched three key electronic databases: Medline, PsycINFO and CINAHL (Cumulative Index to Nursing and Allied Health Literature) for relevant reviews (favouring those using systematic methods) using the following search terms: (neoplasm OR carcinoma OR tumo*r OR cancer) AND (depression OR anxiety) AND review. Only English language articles were considered and searches were limited to the years 2012 to 2017 and updated during February 2019. These years were considered adequate to capture the main themes relating to cancer and common mental disorders in the current literature. The references of highly relevant articles were scrutinised for additional papers and a Google search for important grey literature was also conducted. A minority of significant research articles known to the authors were also consulted.
Factors influencing the development of depression and anxiety among people with cancer
A variety of factors are likely to interact to influence the development of depression and anxiety among people with cancer (summarised in Fig. 1 ), but these are not well understood [ 1 ], and require further research. Individual risk factors that may increase the risk of depression, similar to the general population, include demographic factors, such as age and gender, and social and economic factors such as unemployment, fewer educational qualifications and a lack of social support [ 7 ]. The development of depression and anxiety among people with cancer is also likely to depend on factors at the structural level, including healthcare costs and access, as well as access to welfare support, such as disability benefits, as cancer can have a significant financial impact [ 8 , 9 ]. Several psychological factors are also important. A key factor is the presence of pre-existing mental health problems and their severity. Research has demonstrated that individuals who have previously accessed mental health services before a cancer diagnosis experience excess mortality due to certain cancers, which may reflect late diagnosis, inadequate treatment and a higher rate of adverse health behaviours [ 4 , 10 ]. Personality factors, such as neuroticism, and existing coping skills may also contribute [ 11 ]. The risk of suicide among people with cancer is higher than the general population for certain diagnoses that tend to have poorer prognoses, such as mesothelioma and lung cancer, especially in the first 6 months after diagnosis [ 12 , 13 ]. Individuals who have previously engaged in suicidal behaviour are likely to be particularly vulnerable.
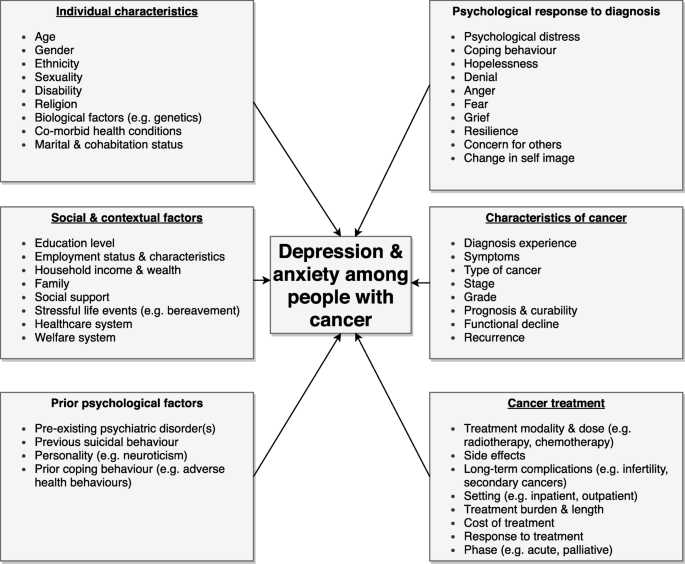
Factors that may contribute to depression and anxiety among people living with and beyond cancer
The individual psychological response to a cancer diagnosis is also likely to be an important component. The experience of being diagnosed, particularly if the diagnosis has been delayed, can be a significant source of distress and can impact on illness acceptance [ 14 ]. Feelings of hopelessness, loss of control and uncertainty around survival and death can also have a detrimental impact, particularly in patients with a poor prognosis. Anxiety around a cancer diagnosis can also lead to sleep disturbance, which may increase the risk of depression [ 15 ]. The stigma surrounding both mental illness and certain types of cancer, such as lung cancer, can lead to feelings of guilt and shame, which could contribute to the onset of depression. For example, the link between smoking and lung cancer can lead to some patients blaming themselves for their illness and experiencing stigma if they have engaged in smoking [ 14 ].
A variety of factors related to the cancer and its treatment are likely to impact on the development of depression and anxiety, including the type of cancer, stage and prognosis. Cancer treatments including immunotherapy and chemotherapy may induce depression through particular biological mechanisms, such as inflammatory pathways, and some medications used to treat chemotherapy-induced nausea can reduce dopaminergic transmission, which is implicated in the development of depressive symptoms [ 16 ]. The use of steroids in cancer treatment can induce depression [ 17 ], and androgen deprivation therapy in the treatment of prostate cancer is also associated with increased risk [ 18 ]. The physical symptoms of specific cancers can also contribute to depression (e.g. incontinence and sexual dysfunction associated with prostate cancer) [ 19 ]. Iatrogenic distress is also commonly reported amongst patients, which could increase the risk of experiencing later problems with depression and anxiety, including post-traumatic stress disorder [ 20 ]. This is often related to a combination of poor communication, a lack of consideration of psychological concerns and disjointed care [ 14 , 20 ].
Prevalence of depression and anxiety among people with cancer
The prevalence of common mental disorders among people with cancer varies widely in the published literature. The mean prevalence of depression using diagnostic interviews is around 13% and using all assessment methods it varies from approximately 4 to 49% [ 2 , 21 ]. This wide variation is due to several factors including the treatment setting, type of cancer included and method used to screen for symptoms (e.g. interview by trained psychiatrist or self-report instrument). The estimated prevalence of depression was found to be 3% in patients with lung cancer, compared to 31% in patients with cancer of the digestive tract, when diagnostic interviews were used [ 21 ]. A meta-analyses of 15 studies meeting a number of quality criteria, including the use of diagnostic interviews, found that the estimated prevalence of depression varied across treatment settings (5 to 16% in outpatients, 4 to 14% in inpatients, 4 to 11% in mixed outpatient and inpatient samples, and 7 to 49% in palliative care) [ 2 ]. There is no universal standardised tool which is recommended for depression screening in patients with cancer and the method used is likely to differ depending on the treatment setting. A meta-analysis of screening and case finding tools for depression in cancer settings identified 63 studies that used 19 different screening tools for depression [ 22 ]. Common screening methods for depression include semi-structured diagnostic interviews, the Hospital Anxiety and Depression Scale - depression subscale (HADS-D) and Center for Epidemiologic Studies Depression Scale (CESD), which are designed to measure the severity of depressive symptoms.
An important aspect that needs to be considered is the timing of increased psychiatric risk. Studies demonstrate that depression tends to be highest during the acute phase and decreases following treatment, but again this likely differs depending on the type of cancer and prognosis [ 21 ]. Using diagnostic interviews, the prevalence of depression during treatment was found to be 14%, 9% in the first year after diagnosis and 8% a year or more after treatment in a meta-analysis of 211 studies [ 21 ]. Of the 238 cohorts included, around 30% included only breast cancer patients and there is a need for research including rarer types of cancer.
As well as the type of cancer, the type of mental health outcome considered is also important and fewer studies have examined anxiety. A systematic review and meta-analysis study focusing on patients with ovarian cancer found that anxiety tended to be higher following treatment (27%) and during treatment (26%), and was lowest pre-treatment (19%) [ 23 ]. The heightened anxiety observed post-treatment may be due to reduced clinical consultations and support following treatment, potential transfer to a palliative setting, and fear of recurrence. Fear of recurrence is one of the most commonly reported issues and an important area of unmet need for cancer survivors [ 24 ]. A lack of outward physical symptoms in ovarian cancer also means that self-monitoring is difficult [ 23 ]. In the same study of ovarian cancer patients, depression was highest before treatment (25%) and during treatment (23%), and reduced following treatment (13%). This is in the context of a lifetime prevalence for clinical depression and anxiety of around 10 and 8%, respectively, amongst women in the UK [ 23 , 25 ].
A similar systematic review of depression and anxiety among patients with prostate cancer found that anxiety tended to be highest pre-treatment (27%) and lowered during treatment (15%) and post-treatment (18%) [ 26 ]. Rates of depression were relatively similar following treatment (18%), during treatment (15%) and pre-treatment (17%), with the 95% confidence intervals for these estimates largely overlapping. For reference, the prevalence of clinical depression and anxiety in men aged over 65 years is less than 9 and 6%, respectively [ 26 ]. A systematic review on the prevalence of psychological distress among testicular cancer survivors demonstrated that around one in five experienced clinically significant anxiety, compared to one in eight among general population controls, with fear of recurrence again being one of the key issues reported [ 27 ]. However, depression was no more prevalent amongst those surviving testicular cancer compared to the general population. In Scotland, the prevalence of depression was found to be highest in patients with lung cancer (13%), followed by gynaecological cancer (11%), breast cancer (9%), colorectal cancer (7%), and genitourinary cancer (6%) [ 28 ]. The authors found depression to be more likely among younger and more socially disadvantaged individuals. In addition, 73% of the patients with depression were not receiving treatment for their mental health. Further research is needed to ascertain the factors which contribute to the uptake and efficacy of treatment for depression. This study also only considered people with cancer who had attended specialist cancer clinics within a defined time period, which likely excluded people who were diagnosed many years ago.
The longer-term psychological impact of cancer has received comparatively little research. The few studies in this area have mainly focused on women with breast cancer and demonstrate that depressive symptoms can persist for over 5 years after diagnosis, though the prevalence of anxiety was not elevated compared to the general population [ 29 ]. A systematic review of the prevalence of depression and anxiety among long-term cancer survivors, including all types, found that anxiety was more prevalent among cancer survivors, compared to healthy controls [ 30 ]. Few studies have focused specifically on younger cancer survivors and more research is needed in this area. A representative study of young adult cancer survivors aged 15 to 39 years in the United States demonstrated that moderate (23% vs 17%) and severe (8% vs 3%) mental distress were significantly higher in those living with cancer for at least 5 years after diagnosis, compared to controls [ 31 ]. 75 and 52% of people with cancer with moderate and severe distress, respectively, had not talked to a mental health professional, with the cost of treatment a potential barrier. Limitations of this study included the focus on self-reported mental distress and not clinical depression or anxiety, as well as the relatively small sample size.
Many studies in this area have a poor response rate, lack representativeness, are based on a small sample of patients (often with the most common types of cancer), which often exclude those with cognitive impairment and patients who are too physically or mentally unwell to take part [ 32 ]. Future studies would benefit from using administrative health data [ 33 ], for example, linking together cancer registries, inpatient and outpatient records and prescribing data. There are also a lack of studies covering populations from low- and middle-income countries [ 34 ]. The estimated prevalence of comorbid common mental disorders is likely to vary depending on the country studied, due to factors such as the health and welfare system. These factors may influence mental health inequalities among people with cancer, which has received little research focus. In a Scottish study, depression was found to be higher in the least advantaged groups (19%), compared to the most advantaged (10%) [ 35 ]. Cancer and comorbid anxiety was also unequally distributed; in the least advantaged groups around 12% had both conditions, compared to 7% among the most advantaged [ 35 ]. Further research is needed in this area to quantify, monitor and prevent inequalities among people with cancer.
It should also be highlighted that the psychological impact of cancer may not always be negative and many people will not experience problems with depression and anxiety. Experiencing temporary distress related to a cancer diagnosis may lead to positive psychological changes in the long-term whereby individuals feel a greater appreciation of life and are able to re-evaluate their priorities [ 36 ]. The factors that protect against the development of common mental disorders and contribute to positive mental health among people living with and beyond cancer merits further research.
Treatment and management of depression and anxiety among people with cancer
To effectively manage and treat depression and anxiety among people with cancer, symptoms must first be identified. However, several social and clinical barriers have been reported. A key issue is the lack of physician time for assessing symptoms. There can also be a normalisation of distress and attribution of the somatic symptoms of depression and anxiety to the cancer. Patients may not disclose psychiatric symptoms because of the stigma surrounding mental health conditions [ 37 ]. Screening for depression and anxiety among patients with cancer is also only of value if it leads to effective treatment and support that is able to improve patient outcomes. Patients may be more reluctant to discuss their mental health needs if they perceive a lack of effective treatment options.
The existing evidence for treating anxiety and depression among patients with cancer is limited and of varying quality [ 38 ]. Studies with small sample sizes are common; this mitigates against the detection of meaningful changes in patient outcomes and these studies often suffer from a high rate of attrition, which likely reflects the high symptom burden and reduced survival in this patient population [ 39 ]. Systematic reviews demonstrate there is a preponderance of studies from the United States, which include a high number of studies focusing on female patients with breast cancer [ 40 ]. However, these studies demonstrate that psychotherapy, psychoeducation and relaxation training may have small to medium short-term effects on relieving emotional distress and reducing symptoms of anxiety and depression, as well as improving health-related quality of life. The evidence for pharmacological treatment of depression with antidepressants is mixed - there are very few studies in this area and those that exist are of low quality [ 41 ]. There is also concern around potential side effects of antidepressants and drug interactions that may affect the efficacy of cancer treatments [ 42 ].
A systematic review and meta-analysis focusing on cognitive behavioural therapy (CBT) found that it may be effective in reducing depression and anxiety and improving quality of life in patients with cancer in the short-term, but potential long-term effects were only sustained for quality of life [ 43 ]. However, in this meta-analysis the included participants were primarily women with breast cancer and there are a lack of studies covering other cancer types. It is likely that collaborative care interventions which involve partnership between psychiatry, clinical psychology and primary care, overseen by a care manager are likely to be most effective in the management and treatment of depression amongst people with cancer [ 44 ]. Treatment should be based on patient preference and also take into account potential adverse side effects [ 44 ]. In a UK-based study it was found that only a third of patients with cancer and related psychological or emotional distress were willing to be referred for support [ 45 ]. Qualitative studies also demonstrate that patients often do not want to discuss their feelings with nurses during cancer treatment [ 46 ]. However, patients valued having the option to talk about their emotions, but they preferred to choose with whom and when. There is therefore a need for further research into some of the barriers to obtaining mental health support among those affected by cancer and experiencing distress to prevent future problems.
The self-management of psychological distress among people with cancer may be beneficial and could help prevent distress becoming clinical depression or anxiety. Self-management can be defined as: “The individual’s ability to manage the symptoms, treatment, physical and psychosocial consequences and lifestyle changes inherent in living with a chronic condition. Efficacious self-management encompasses the ability to monitor one’s condition and to affect the cognitive, behavioural and emotional responses necessary to maintain a satisfactory quality of life. Thus, a dynamic and continuous process of self-regulation is established.” [ 47 ] . Studies on self-management, cancer and psychological distress have focused on the treatment phase, with fewer investigating interventions following treatment or at the end of life [ 48 ]. There is evidence to suggest that self-management of psychological distress in cancer can help to empower patients and families to care for themselves in a way which is preferable for them. Self-management interventions that have shown promise include education, monitoring, teaching and counselling to help patients manage the short- and long-term physical and psychosocial effects of cancer [ 48 ]. However, a recent systematic review examining the impact of self-management interventions on outcomes including quality of life, self-efficacy and symptom management (such as psychological distress) amongst cancer survivors demonstrated a lack of evidence to support any specific intervention and found that the six included interventions lacked sustainability, bringing into question their long-term effectiveness and value for money [ 49 ]. Again, the included studies were dominated by women with breast cancer, with only two covering other cancers.
Effective treatment and management strategies may also differ according to the demographic group affected. In a report by CLIC (Cancer and Leukaemia in Childhood) Sargent which surveyed 146 young people with cancer, keeping in touch with friends and family, talking to others with similar experiences and access to the internet in hospital were reported to help maintain mental health during cancer treatment [ 50 ]. Of the young people who mentioned they would find it helpful to talk to other people with similar experiences, 60% said they would prefer to do this online. Young people also reported that the available services were not tailored to deal with those aged under 18 or the emotional impact of cancer. In addition, those who accessed services mentioned that there is a lack of suitable long-term emotional support. Just over 40% of the young people who took part did not access support for their mental health needs.
It is clear that a more personalised approach to supporting the psychological health of people with cancer is needed [ 51 ]. Some people may not want or require support or treatment, others will be able to self-manage, and some may have more complex needs that require more intensive follow-up and support. At diagnosis, the psychological health of patients should be considered alongside their physical health and sources of support offered. Needs and symptoms may also change over time. Evaluation of more recent personalised approaches to follow-up care that have been adopted in several areas including England and Northern Ireland [ 51 ] are needed to understand the role they may have in preventing longer term depression and anxiety amongst cancer survivors.
A key barrier affecting research progress in this area is funding [ 52 ]. In the UK, money spent on research into the biology of cancer was more than five times than that spent on ‘Cancer Control, Survivorship and Outcomes’ during 2017/18 [ 53 ]. Research into the mental health and wellbeing of people living with and beyond cancer is likely to only be a small part of this. Research is urgently needed in this area as more people survive cancer and for some cancers, such as multiple myeloma and colorectal cancer, risk is increasing in younger cohorts [ 54 ]. The long-term (those that begin during treatment and continue afterwards) and late effects of cancer treatment (those that begin after treatment is completed), such as secondary cancers, infertility, chronic pain and insomnia, are likely to affect the mental wellbeing of cancer survivors, potentially contributing to depression and anxiety [ 6 ]. The National Cancer Research Institute (NCRI) in the UK have also recently highlighted research into the short-term and long-term psychological impacts of cancer and its treatment as a key priority, following surveys of over 3500 patients, carers, and health and social care professionals [ 55 ].
The mental health of people living with and beyond cancer in its various types and stages is an important and growing research and clinical priority. Compared to the general population, the prevalence of anxiety and depression is often higher among people with cancer, but estimates vary due to a number of factors, such as the type and stage of cancer. Patients often do not obtain psychological support or treatment. This is likely due to several factors, including lack of awareness and identification of psychiatric symptoms, an absence of support available or offered, lack of evidence around effective treatments, stigma, and patient preference. In particular, we highlight the lack of high-quality research into the mental health of long-term cancer survivors, the potential impact of long-term and late effects of cancer treatment, and the few studies focused on prevention. Further research that includes the less common types of cancer is required, as well as the inclusion of younger people and populations from low- and middle-income countries. Given the increasing numbers of people living with and beyond cancer, this research is of timely importance.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
Cognitive behavioural therapy
Center for Epidemiologic Studies Depression Scale
Cumulative Index to Nursing and Allied Health Literature
Cancer and Leukaemia in Childhood
Hospital Anxiety and Depression Scale - depression subscale
National Cancer Research Institute
Pitman A, Suleman S, Hyde N, Hodgkiss A. Depression and anxiety in patients with cancer. BMJ. 2018;361:k1415.
Article PubMed Google Scholar
Walker J, Hansen CH, Martin P, Sawhney A, Thekkumpurath P, Beale C, Symeonides S, Wall L, Murray G, Sharpe M. Prevalence of depression in adults with cancer: a systematic review. Ann Oncol. 2013;24(4):895–900.
Article CAS PubMed Google Scholar
Zhu J, Fang F, Sjölander A, Fall K, Adami HO, Valdimarsdóttir U. First-onset mental disorders after cancer diagnosis and cancer-specific mortality: a nationwide cohort study. Ann Oncol. 2017;28(8):1964–9.
Klaassen Z, Wallis CJD, Goldberg H, Chandrasekar T, Sayyid RK, Williams SB, Moses KA, Terris MK, Nam RK, Urbach D, et al. The impact of psychiatric utilisation prior to cancer diagnosis on survival of solid organ malignancies. Br J Cancer. 2019;120:840–7.
Article PubMed PubMed Central Google Scholar
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Shapiro CL. Cancer survivorship. N Engl J Med. 2018;379(25):2438–50.
Wen S, Xiao H, Yang Y. The risk factors for depression in cancer patients undergoing chemotherapy: a systematic review. Support Care Cancer. 2019;27(1):57–67.
Gilligan AM, Alberts DS, Roe DJ, Skrepnek GH. Death or Debt? National Estimates of Financial Toxicity in Persons with Newly-Diagnosed Cancer. Am J Med. 2018;131(10):1187–99 e1185.
Lu L, O'Sullivan E, Sharp L. Cancer-related financial hardship among head and neck cancer survivors: Risk factors and associations with health-related quality of life. Psycho-Oncology. 2019;28(4):863–71.
Musuuza JS, Sherman ME, Knudsen KJ, Sweeney HA, Tyler CV, Koroukian SM. Analyzing excess mortality from cancer among individuals with mental illness. Cancer. 2013;119(13):2469–76.
Cook SA, Salmon P, Hayes G, Byrne A, Fisher PL. Predictors of emotional distress a year or more after diagnosis of cancer: a systematic review of the literature. Psycho-oncology. 2018;27(3):791–801.
Henson KE, Brock R, Charnock J, Wickramasinghe B, Will O, Pitman A. Risk of suicide after cancer diagnosis in England. JAMA Psychiatry. 2019;76(1):51–60.
Wang SM, Chang JC, Weng SC, Yeh MK, Lee CS. Risk of suicide within 1 year of cancer diagnosis. Int J Cancer. 2018;142(10):1986–93.
Ball H, Moore S, Leary A. A systematic literature review comparing the psychological care needs of patients with mesothelioma and advanced lung cancer. Eur J Oncol Nurs. 2016;25:62–7.
Howell D, Harris C, Aubin M, Olson K, Sussman J, MacFarlane J, Taylor C, Oliver TK, Keller-Olaman S, Davidson JR, et al. Sleep disturbance in adults with cancer: a systematic review of evidence for best practices in assessment and management for clinical practice. Ann Oncol. 2013;25(4):791–800.
Smith HR. Depression in cancer patients: pathogenesis, implications and treatment (review). Oncol Lett. 2015;9(4):1509–14.
Article CAS PubMed PubMed Central Google Scholar
Ismail MF, Lavelle C, Cassidy EM. Steroid-induced mental disorders in cancer patients: a systematic review. Future Oncol. 2017;13(29):2719–31.
Nead KT, Sinha S, Yang DD, Nguyen PL. Association of androgen deprivation therapy and depression in the treatment of prostate cancer: A systematic review and meta-analysis. Urologic Oncol. 2017;35(11):664 e661–664.e669.
CAS Google Scholar
De Sousa A, Sonavane S, Mehta J. Psychological aspects of prostate cancer: a clinical review. Prostate Cancer Prostatic Dis. 2012;15(2):120–7.
Cordova MJ, Riba MB, Spiegel D. Post-traumatic stress disorder and cancer. Lancet Psychiatry. 2017;4(4):330–8.
Krebber AMH, Buffart LM, Kleijn G, Riepma IC, de Bree R, Leemans CR, Becker A, Brug J, van Straten A, Cuijpers P, et al. Prevalence of depression in cancer patients: a meta-analysis of diagnostic interviews and self-report instruments. Psycho-Oncology. 2014;23(2):121–30.
Mitchell AJ, Meader N, Davies E, Clover K, Carter GL, Loscalzo MJ, Linden W, Grassi L, Johansen C, Carlson LE, et al. Meta-analysis of screening and case finding tools for depression in cancer: evidence based recommendations for clinical practice on behalf of the depression in Cancer care consensus group. J Affect Disord. 2012;140(2):149–60.
Watts S, Prescott P, Mason J, McLeod N, Lewith G. Depression and anxiety in ovarian cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open. 2015;5(11):e007618.
Simard S, Thewes B, Humphris G, Dixon M, Hayden C, Mireskandari S, Ozakinci G. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. 2013;7(3):300–22.
Halliwell E, Main L, Richardson C. The fundamental facts: the latest facts and figures on mental health: mental Health Foundation; 2007.
Google Scholar
Watts S, Leydon G, Birch B, Prescott P, Lai L, Eardley S, Lewith G. Depression and anxiety in prostate cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open. 2014;4(3):e003901.
Smith AB, Rutherford C, Butow P, Olver I, Luckett T, Grimison P, Toner G, Stockler M, King M. A systematic review of quantitative observational studies investigating psychological distress in testicular cancer survivors. Psycho-Oncology. 2018;27(4):1129–37.
Walker J, Hansen CH, Martin P, Symeonides S, Ramessur R, Murray G, Sharpe M. Prevalence, associations, and adequacy of treatment of major depression in patients with cancer: a cross-sectional analysis of routinely collected clinical data. Lancet Psychiatry. 2014;1(5):343–50.
Maass SW, Roorda C, Berendsen AJ, Verhaak PF, de Bock GH. The prevalence of long-term symptoms of depression and anxiety after breast cancer treatment: a systematic review. Maturitas. 2015;82(1):100–8.
Mitchell AJ, Ferguson DW, Gill J, Paul J, Symonds P. Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: a systematic review and meta-analysis. Lancet Oncol. 2013;14(8):721–32.
Kaul S, Avila JC, Mutambudzi M, Russell H, Kirchhoff AC, Schwartz CL. Mental distress and health care use among survivors of adolescent and young adult cancer: a cross-sectional analysis of the National Health Interview Survey. Cancer. 2017;123(5):869–78.
Ryan D, Gallagher P, Wright S, Cassidy E. Methodological challenges in researching psychological distress and psychiatric morbidity among patients with advanced cancer: what does the literature (not) tell us? Palliat Med. 2012;26(2):162–77.
Lu L, Deane J, Sharp L. Understanding survivors’ needs and outcomes: the role of routinely collected data. Curr Opinion Supportive Palliative Care. 2018;12(3):254–60.
Article Google Scholar
Walker ZJ, Jones MP, Ravindran AV. Psychiatric disorders among people with cancer in low- and lower-middle-income countries: study protocol for a systematic review and meta-analysis. BMJ Open. 2017;7(8):e017043.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43.
Casellas-Grau A, Ochoa C, Ruini C. Psychological and clinical correlates of posttraumatic growth in cancer: a systematic and critical review. Psycho-Oncology. 2017;26(12):2007–18.
Kissane DW. Unrecognised and untreated depression in cancer care. Lancet Psychiatry. 2014;1(5):320–1.
Rodin G, Lloyd N, Katz M, Green E, Mackay JA, Wong RK. Supportive care guidelines Group of Cancer Care Ontario Program in evidence-based care: the treatment of depression in cancer patients: a systematic review. Support Care Cancer. 2007;15(2):123–36.
Hui D, Glitza I, Chisholm G, Yennu S, Bruera E. Attrition rates, reasons, and predictive factors in supportive care and palliative oncology clinical trials. Cancer. 2013;119(5):1098–105.
Faller H, Schuler M, Richard M, Heckl U, Weis J, Küffner R. Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: systematic review and meta-analysis. J Clin Oncol. 2013;31(6):782–93.
Ostuzzi G, Matcham F, Dauchy S, Barbui C, Hotopf M. Antidepressants for the treatment of depression in people with cancer. Cochrane Database Syst Rev. 2018;4(4):CD011006.
Ostuzzi G, Benda L, Costa E, Barbui C. Efficacy and acceptability of antidepressants on the continuum of depressive experiences in patients with cancer: systematic review and meta-analysis. Cancer Treat Rev. 2015;41(8):714–24.
Osborn RL, Demoncada AC, Feuerstein M. Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: meta-analyses. Int J Psychiatry Med. 2006;36(1):13–34.
Li M, Kennedy EB, Byrne N, Gérin-Lajoie C, Katz MR, Keshavarz H, Sellick S, Green E. Systematic review and meta-analysis of collaborative care interventions for depression in patients with cancer. Psycho-Oncol. 2017;26(5):573–87.
Baker-Glenn EA, Park B, Granger L, Symonds P, Mitchell AJ. Desire for psychological support in cancer patients with depression or distress: validation of a simple help question. Psycho-Oncol. 2011;20(5):525–31.
Kvåle K. Do cancer patients always want to talk about difficult emotions? A qualitative study of cancer inpatients communication needs. Eur J Oncol Nurs. 2007;11(4):320–7.
Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. 2002;48(2):177–87.
McCorkle R, Ercolano E, Lazenby M, Schulman-Green D, Schilling LS, Lorig K, Wagner EH. Self-management: enabling and empowering patients living with cancer as a chronic illness. CA Cancer J Clin. 2011;61(1):50–62.
Boland L, Bennett K, Connolly D. Self-management interventions for cancer survivors: a systematic review. Support Care Cancer. 2018;26(5):1585–95.
PubMed Google Scholar
Sargent CLIC. Hidden costs: the mental health impact of a cancer diagnosis on young people; 2017.
Alfano CM, Mayer DK, Bhatia S, Maher J, Scott JM, Nekhlyudov L, Merrill JK, Henderson TO. Implementing personalized pathways for cancer follow-up care in the United States: proceedings from an American Cancer Society–American Society of Clinical Oncology summit. CA Cancer J Clin. 2019;69(3):234–47.
Foster C, Calman L, Richardson A, Pimperton H, Nash R. Improving the lives of people living with and beyond cancer: generating the evidence needed to inform policy and practice. J Cancer Policy. 2018;15:92–5.
National Cancer Research Institute. Spend by Research Category and Disease Site. [ https://www.ncri.org.uk/ncri-cancer-research-database-old/spend-by-research-category-and-disease-site/ ]. Accessed 27 June 2019.
Sung H, Siegel RL, Rosenberg PS, Jemal A. Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Health. 2019;4(3):e137–47.
National Cancer Research Institute. The UK Top living with and beyond cancer research priorities. [ https://www.ncri.org.uk/lwbc/#lwbc_questions ]. Accessed 27 June 2019.
Download references
Acknowledgements
This article is built on a literature review conducted by CLN and LK for a project on ‘Supporting the mental and emotional health of people with cancer’ funded by the Big Lottery Fund when CLN was an employee of the Mental Health Foundation in Scotland during 2017.
CLN is currently supported by the Medical Research Council (grant number MR/R024774/1). SVK is funded by a NHS Research Scotland (NRS) Senior Clinical Fellowship (SCAF/15/02), the Medical Research Council (MC_UU_12017/13 & MC_UU_12017/15) and Scottish Government Chief Scientist Office (SPHSU13 & SPHSU15). The funders had no role in the study design; collection, analysis and interpretation of data; the writing of the article; and in the decision to submit it for publication.
Author information
Authors and affiliations.
Institute of Health & Wellbeing, University of Glasgow, Glasgow, Scotland, UK
Claire L. Niedzwiedz, Kathryn A. Robb & Daniel J. Smith
University of Strathclyde, Centre for Health Policy, Glasgow, Scotland, UK
Lee Knifton
Mental Health Foundation, Glasgow, Scotland, UK
MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, Glasgow, Scotland, UK
Srinivasa Vittal Katikireddi
You can also search for this author in PubMed Google Scholar
Contributions
CLN and LK conceived the article. CLN conducted the searches and drafted the manuscript. CLN, LK, SVK, KAR and DJS interpreted the findings. All authors critically revised the manuscript, read and approved the final version.
Corresponding author
Correspondence to Claire L. Niedzwiedz .
Ethics declarations
Ethics approval and consent to participate.
Not applicable
Consent for publication
Competing interests.
The authors declare that they have no competing interests except for the funding acknowledged.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Niedzwiedz, C.L., Knifton, L., Robb, K.A. et al. Depression and anxiety among people living with and beyond cancer: a growing clinical and research priority. BMC Cancer 19 , 943 (2019). https://doi.org/10.1186/s12885-019-6181-4
Download citation
Received : 19 March 2019
Accepted : 20 September 2019
Published : 11 October 2019
DOI : https://doi.org/10.1186/s12885-019-6181-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Multimorbidity
- Survivorship
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 19 April 2022
Focus Issue: The Future Of Cancer Research
Nature Medicine volume 28 , page 601 ( 2022 ) Cite this article
14k Accesses
6 Citations
8 Altmetric
Metrics details
New treatments and technologies offer exciting prospects for cancer research and care, but their global impact rests on widespread implementation and accessibility.
Cancer care has advanced at an impressive pace in recent years. New insights into tumor immunology and biology, combined with advances in artificial intelligence, nano tools, genetic engineering and sequencing — to name but a few — promise ever-more-powerful capabilities in the prevention, diagnosis and personalized treatment of cancer. How do we harness and build on these advances? How do we make them work in different global settings? In this issue, we present a Focus dedicated to the future of cancer research, in which we take stock of progress and explore ways to deliver research and care that is innovative, sustainable and patient focused.
This year brought news that two of the first patients with leukemia to receive chimeric antigen receptor (CAR) T cell treatment remain in remission more than a decade later . Writing in this issue, Carl June — who helped to treat these first patients — and colleagues reflect on how early transplant medicine laid a solid foundation for CAR T cell development in blood cancers, and how this is now paving the way for the use of engineered cell therapies in solid cancers. In a noteworthy step toward this goal, Haas and colleagues present results of a phase 1 trial of CAR T cells in metastatic, castration-resistant prostate cancer — a disease that has seen relatively few new treatment options in recent years.
Up to now, CAR T cells have been used only in the context of relapsed or refractory hematological malignancies, but in this issue, Neelapu et al . present phase 2 study data that suggest CAR T cell therapy could be beneficial when used earlier in certain high-risk patients. In addition, prospective data from van den Brink et al . support a role for the gut microbiome composition in CAR T cell therapy outcomes, highlighting new avenues of research to help maximize therapeutic benefit.
Although the idea that the gut microbiome influences CAR T cell therapy outcomes may be relatively new, it has been known for some time that it has a role in the response to checkpoint-inhibitor immunotherapy. A plethora of microbe-targeting therapies are now under investigation for cancer treatment; in this issue, Pal and colleagues describe one such strategy — whereby the combination of a defined microbial supplement with checkpoint blockade led to improved responses in patients with advanced kidney cancer. In their Review, Jennifer Wargo and colleagues take stock of the latest research in this field, and predict that microbial targeting could become a pillar of personalized cancer care over the next decade.
The theme for this year’s World Cancer Day was ‘Close the care gap’ — a message that is woven through several pieces in this issue. Early detection strategies have enormous potential to make a difference in this area; reviewing the latest advances, Rebecca Fitzgerald and colleagues ask who should be tested, and how — and outline their vision for personalized, risk-based screening, keeping in mind practicality and clinical implementation. Journalist Carrie Arnold reports on an emerging strategy known as ‘theranostics’ that aims to both diagnose and treat cancers in a unified approach, highlighting the growing commercial interest in this field. Of course, commercial interest does not equate to widespread availability or equal access to new therapies, and increasingly sophisticated technologies — although beneficial for some — can serve to widen existing inequalities.
Pediatric cancers lag far behind adult cancers in terms of drug development and approval. Nancy Goodman, a patient advocate whose son died from a childhood cancer, argues that market failures are largely to blame for the gap — but that legislative changes can correct this. Although in some cases there is a strong mechanistic rationale for testing promising adult cancer therapies or combinations in children, translational research is also needed to identify new therapeutic targets — such as the approach taken by Behjati and colleagues , which sheds new light on the molecular characteristics of an aggressive form of infant leukemia.
Meanwhile, for adult cancers, countless new therapeutic modalities are on the horizon , and drug approvals based on genomic biomarkers have accelerated in recent years. Unfortunately, their implementation into routine clinical care is progressing at a much slower pace. In their Perspective, Emile Voest and colleagues point out that bridging this gap will require investment in health infrastructure, as well as in education and decision-support tools, among other things.
Perhaps the most striking gap is that between high-income countries and low- and middle-income countries, not only in terms of cancer survival outcomes but also in terms of resources and infrastructure for impactful research. In their Perspective, CS Pramesh and colleagues outline their top priorities for cancer research in low- and middle-income countries, arguing that cancer research must be regionally relevant and geared toward reducing the number of patients diagnosed with advanced disease. Practicality is key — a sentiment echoed by Bishal Gyawali and Christopher Booth, who call for a “ common sense revolution ” in oncology, and regulatory policies and trial designs that serve patients better.
To realize this goal, clinical trial endpoints and outcome measures should be designed to minimize the burden on patients and maximize the potential for improving on the standard of care. This should go beyond survival outcomes; systemic effects, including cachexia and pain, have a major impact on quality of life and mental health during and after treatment. Two articles in this issue highlight the enormous psychological burden associated with a cancer diagnosis; increased risks of depression, self-harm and suicide emphasize the need for psychosocial interventions and a holistic approach to treatment.
As noted by members of the Bloomberg New Economy International Cancer Coalition in their Comment , the widespread adoption of telemedicine and remote monitoring in response to the COVID-19 pandemic could, if retained, help to make cancer trials more patient centered. Therefore, as health systems and research infrastructures adapt to the ongoing pandemic, there exists an unprecedented opportunity to reshape the landscape of cancer research.
We at Nature Medicine are committed to helping shape this transformation. We are issuing a call for research papers that utilize innovative approaches to address current challenges in cancer prevention, detection, diagnosis and treatment — both clinical trials and population-based studies with global implications. Readers can find more information about publishing clinical research in Nature Medicine at https://www.nature.com/nm/clinicalresearch .
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Focus Issue: The Future Of Cancer Research. Nat Med 28 , 601 (2022). https://doi.org/10.1038/s41591-022-01809-z
Download citation
Published : 19 April 2022
Issue Date : April 2022
DOI : https://doi.org/10.1038/s41591-022-01809-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Skip to main content
- Keyboard shortcuts for audio player
This experimental drug could change the field of cancer research

Sacha Pfeiffer

Jonaki Mehta

The new treatment is categorized as immunotherapy. skaman306/Getty Images hide caption
The new treatment is categorized as immunotherapy.
A tiny group of people with rectal cancer just experienced something of a scientific miracle: their cancer simply vanished after an experimental treatment.
In a very small trial done by doctors at New York's Memorial Sloan Kettering Cancer Center, patients took a drug called dostarlimab for six months. The trial resulted in every single one of their tumors disappearing. The trial group included just 18 people, and there's still more to be learned about how the treatment worked. But some scientists say these kinds of results have never been seen in the history of cancer research.
Dr. Hanna Sanoff of the University of North Carolina's Lineberger Comprehensive Cancer Center joined NPR's All Things Considered to outline how this drug works and what it could mean for the future of cancer research. Although she was not involved with the study, Dr. Sanoff has written about the results.
This interview has been lightly edited
On her first reaction to the results: I mean, I am incredibly optimistic. Like you said in the introduction, we have never seen anything work in 100 percent of people in cancer medicine.
On how the drug works to treat cancer: This drug is one of a class of drugs called immune checkpoint inhibitors. These are immunotherapy medicines that work not by directly attacking the cancer itself, but actually getting a person's immune system to essentially do the work. These are drugs that have been around in melanoma and other cancers for quite a while, but really have not been part of the routine care of colorectal cancers until fairly recently.
On the kinds of side effects patients experienced: Very, very few in this study - in fact, surprisingly few. Most people had no severe adverse effects at all.
On how this study could be seen as 'practice-changing': Our hope would be that for this subgroup of people - which is only about five percent to 10 percent of people who have rectal cancer - if they can go on and just get six months of immunotherapy and not have any of the rest of this - I don't even know the word to use. Paradigm shift is often used, but this really absolutely is paradigm-shifting.
On why the idea of being able to skip surgery for cancer treatment is so revolutionary: In rectal cancer, this is part of the conversation we have with someone when they're diagnosed. We are very hopeful for being able to cure you, but unfortunately, we know our treatments are going to leave you with consequences that may, in fact, be life-changing. I have had patients who, after their rectal cancer, have barely left the house for years - and in a couple of cases, even decades - because of the consequences of incontinence and the shame that's associated with this.
On next steps for the drug: What I'd really like us to do is get a bigger trial where this drug is used in a much more diverse setting to understand what the real, true response rate is going to be. It's not going to end up being 100 percent. I hope I bite my tongue on that in the future, but I can't imagine it will be 100 percent. And so when we see what the true response rate is, that's when I think we can really do this all the time.
This piece was reported by Sacha Pfeiffer, produced by Jonaki Mehta and edited by Kathryn Fox. It was adapted for the web by Manuela Lopez Restrepo.
- cancer treatment
Cancer patients often do better with less intensive treatment, research shows

Scaling back treatment for three kinds of cancer can make life easier for patients without compromising outcomes, doctors reported at the world’s largest cancer conference .
It’s part of a long-term trend toward studying whether doing less — less surgery, less chemotherapy or less radiation — can help patients live longer and feel better. The latest studies involved ovarian and esophageal cancer and Hodgkin lymphoma.
Thirty years ago, cancer research was about doing more, not less. In one sobering example, women with advanced breast cancer were pushed to the brink of death with massive doses of chemotherapy and bone marrow transplants. The approach didn’t work any better than chemotherapy and patients suffered.
Now, in a quest to optimize cancer care, researchers are asking: “Do we need all that treatment that we have used in the past?”
It’s a question, “that should be asked over and over again,” said Dr. Tatjana Kolevska, medical director for the Kaiser Permanente National Cancer Excellence Program, who was not involved in the new research.
Often, doing less works because of improved drugs.
“The good news is that cancer treatment is not only becoming more effective, it’s becoming easier to tolerate and associated with less short-term and long-term complications,” said Dr. William G. Nelson of Johns Hopkins School of Medicine, who was also not involved in the new research.
Latest news on cancer treatment
- Cancer-fighting antibodies inject chemo directly into tumor cells, upping effectiveness.
- Long-term study shows 'remarkable' treatment helps patients with deadly nonsmoking-related lung cancer.
- FDA approves groundbreaking treatment for advanced melanoma.
Studies demonstrating the trend were discussed over the weekend at an American Society of Clinical Oncology conference in Chicago. Here are the highlights:
Ovarian cancer
French researchers found that it’s safe to avoid removing lymph nodes that appear healthy during surgery for advanced ovarian cancer. The study compared the results for 379 patients — half had their lymph nodes removed and half did not. After nine years, there was no difference in how long the patients lived and those with less-extreme surgery had fewer complications, such as the need for blood transfusions. The research was funded by the National Institute of Cancer in France.
Esophageal cancer
This German study looked at 438 people with a type of cancer of the esophagus that can be treated with surgery. Half received a common treatment plan that included chemotherapy and surgery on the esophagus, the tube that carries food from the throat to the stomach. Half got another approach that includes radiation too. Both techniques are considered standard. Which one patients get can depend on where they get treatment.
After three years, 57% of those who got chemo and surgery were alive, compared to 51% of those who got chemo, surgery and radiation. The German Research Foundation funded the study.
Hodgkin lymphoma
A comparison of two chemotherapy regimens for advanced Hodgkin lymphoma found the less intensive treatment was more effective for the blood cancer and caused fewer side effects.
After four years, the less harsh chemo kept the disease in check in 94% of people, compared to 91% of those who had the more intense treatment. The trial included 1,482 people in nine countries — Germany, Austria, Switzerland, the Netherlands, Denmark, Sweden, Norway, Australia and New Zealand — and was funded by Takeda Oncology, the maker of one of the drugs used in the gentler chemo that was studied.
The Associated Press

- Adolescent and Young Adult Cancer
- Bile Duct Cancer
- Bladder Cancer
- Brain Cancer
- Breast Cancer
- Cervical Cancer
- Childhood Cancer
- Colorectal Cancer
- Endometrial Cancer
- Esophageal Cancer
- Head and Neck Cancer
- Kidney Cancer
- Liver Cancer
- Lung Cancer
- Mouth Cancer
- Mesothelioma
- Multiple Myeloma
- Neuroendocrine Tumors
- Ovarian Cancer
- Pancreatic Cancer
- Prostate Cancer
- Skin Cancer/Melanoma
- Stomach Cancer
- Testicular Cancer
- Throat Cancer
- Thyroid Cancer
- Prevention and Screening
- Diagnosis and Treatment
- Research and Clinical Trials
- Survivorship

Request an appointment at Mayo Clinic

New research discovers a new combination of therapy for people with a type of leukemia, leading them to live longer
Share this:.
By Kelley Luckstein
In a new multicenter international study led by the Mayo Clinic Comprehensive Cancer Center , researchers found that people with the B-cell precursor subtype of acute lymphoblastic leukemia (BCP-ALL), who also lacked a genetic abnormality known as the Philadelphia chromosome and were in remission with no trace of cancer, showed significantly higher survival rates when blinatumomab was added to their chemotherapy treatment. The randomized study results are published this month in the New England Journal of Medicine.
"These results are encouraging and establish a new standard of treatment for people with BCP-ALL," says Mark Litzow, M.D. , lead study author and hematologist at the Mayo Clinic Comprehensive Cancer Center. "The addition of blinatumomab to chemotherapy reduced the risk of leukemia recurrence and death by nearly 60%."
Blinatumomab is a type of immunotherapy administered intravenously and brings a normal immune cell called a T cell close to a leukemia cell so it can destroy it. The Food and Drug Administration approved blinatumomab for patients in remission who have traces of cancer, also known as measurable residual disease (MRD)-positive. In this study, blinatumomab was added to see if it could lessen the risk of the ALL coming back and relapsing in a person who had no detection of cancer, also known as MRD-negative, following initial chemotherapy.
The study enrolled 488 participants aged 30 to 70 years with BCP-ALL, and 224 of them were in remission and MRD-negative following the initial course of treatment with chemotherapy. The 224 participants were equally randomized into two arms; the first arm would receive blinatumomab with chemotherapy, and the second arm would receive the standard treatment of chemotherapy alone.
The results showed that 85% of participants treated with blinatumomab and chemotherapy were alive at three years, compared to 68% of those who received chemotherapy alone, which is the standard treatment.
"We plan to build on this study to reduce the amount of chemotherapy people need to receive, ultimately leading to fewer side effects from the treatment and improving overall survival rates," Dr. Litzow says.
This study was conducted by the ECOG-ACRIN Cancer Research Group and funded in part by the National Cancer Institute of the National Institutes of Health . See the full paper for the complete list of funding and authors.
Dr. Litzow has received research funding from Amgen and served on a speaker's bureau for Amgen related to this study.
A version of this article was originally published on the Mayo Clinic News Network .
Related Posts

Diagnosed with chronic lymphocytic leukemia at 38, Alli Benezra found support to navigate treatment through two pregnancies at Mayo Clinic.

With the help of specialized genetic testing at Mayo Clinic, Shannon Camlek was finally able to achieve remission of acute myeloid leukemia.

Learn about CAR-T cell therapy and research at Mayo Clinic to reduce its side effects and expand its use beyond blood cancers.
Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
- Cancer is a leading cause of death worldwide, accounting for nearly 10 million deaths in 2020, or nearly one in six deaths.
- The most common cancers are breast, lung, colon and rectum and prostate cancers.
- Around one-third of deaths from cancer are due to tobacco use, high body mass index, alcohol consumption, low fruit and vegetable intake, and lack of physical activity. In addition, air pollution is an important risk factor for lung cancer.
- Cancer-causing infections, such as human papillomavirus (HPV) and hepatitis, are responsible for approximately 30% of cancer cases in low- and lower-middle-income countries.
- Many cancers can be cured if detected early and treated effectively.
Cancer is a generic term for a large group of diseases that can affect any part of the body. Other terms used are malignant tumours and neoplasms. One defining feature of cancer is the rapid creation of abnormal cells that grow beyond their usual boundaries, and which can then invade adjoining parts of the body and spread to other organs; the latter process is referred to as metastasis. Widespread metastases are the primary cause of death from cancer.
The problem
Cancer is a leading cause of death worldwide, accounting for nearly 10 million deaths in 2020 (1). The most common in 2020 (in terms of new cases of cancer) were:
- breast (2.26 million cases);
- lung (2.21 million cases);
- colon and rectum (1.93 million cases);
- prostate (1.41 million cases);
- skin (non-melanoma) (1.20 million cases); and
- stomach (1.09 million cases).
The most common causes of cancer death in 2020 were:
- lung (1.80 million deaths);
- colon and rectum (916 000 deaths);
- liver (830 000 deaths);
- stomach (769 000 deaths); and
- breast (685 000 deaths).
Each year, approximately 400 000 children develop cancer. The most common cancers vary between countries. Cervical cancer is the most common in 23 countries.
Cancer arises from the transformation of normal cells into tumour cells in a multi-stage process that generally progresses from a pre-cancerous lesion to a malignant tumour. These changes are the result of the interaction between a person's genetic factors and three categories of external agents, including:
- physical carcinogens, such as ultraviolet and ionizing radiation;
- chemical carcinogens, such as asbestos, components of tobacco smoke, alcohol, aflatoxin (a food contaminant), and arsenic (a drinking water contaminant); and
- biological carcinogens, such as infections from certain viruses, bacteria, or parasites.
WHO, through its cancer research agency, the International Agency for Research on Cancer (IARC), maintains a classification of cancer-causing agents.
The incidence of cancer rises dramatically with age, most likely due to a build-up of risks for specific cancers that increase with age. The overall risk accumulation is combined with the tendency for cellular repair mechanisms to be less effective as a person grows older.
Risk factors
Tobacco use, alcohol consumption, unhealthy diet, physical inactivity and air pollution are risk factors for cancer and other noncommunicable diseases.
Some chronic infections are risk factors for cancer; this is a particular issue in low- and middle-income countries. Approximately 13% of cancers diagnosed in 2018 globally were attributed to carcinogenic infections, including Helicobacter pylori, human papillomavirus (HPV), hepatitis B virus, hepatitis C virus, and Epstein-Barr virus (2).
Hepatitis B and C viruses and some types of HPV increase the risk for liver and cervical cancer, respectively. Infection with HIV increases the risk of developing cervical cancer six-fold and substantially increases the risk of developing select other cancers such as Kaposi sarcoma.
Reducing the burden
Between 30 and 50% of cancers can currently be prevented by avoiding risk factors and implementing existing evidence-based prevention strategies. The cancer burden can also be reduced through early detection of cancer and appropriate treatment and care of patients who develop cancer. Many cancers have a high chance of cure if diagnosed early and treated appropriately.
Cancer risk can be reduced by:
- not using tobacco;
- maintaining a healthy body weight;
- eating a healthy diet, including fruit and vegetables;
- doing physical activity on a regular basis;
- avoiding or reducing consumption of alcohol;
- getting vaccinated against HPV and hepatitis B if you belong to a group for which vaccination is recommended;
- avoiding ultraviolet radiation exposure (which primarily results from exposure to the sun and artificial tanning devices) and/or using sun protection measures;
- ensuring safe and appropriate use of radiation in health care (for diagnostic and therapeutic purposes);
- minimizing occupational exposure to ionizing radiation; and
- reducing exposure to outdoor air pollution and indoor air pollution, including radon (a radioactive gas produced from the natural decay of uranium, which can accumulate in buildings — homes, schools and workplaces).
Early detection
Cancer mortality is reduced when cases are detected and treated early. There are two components of early detection: early diagnosis and screening.
Early diagnosis
When identified early, cancer is more likely to respond to treatment and can result in a greater probability of survival with less morbidity, as well as less expensive treatment. Significant improvements can be made in the lives of cancer patients by detecting cancer early and avoiding delays in care.
Early diagnosis consists of three components:
- being aware of the symptoms of different forms of cancer and of the importance of seeking medical advice when abnormal findings are observed;
- access to clinical evaluation and diagnostic services; and
- timely referral to treatment services.
Early diagnosis of symptomatic cancers is relevant in all settings and the majority of cancers. Cancer programmes should be designed to reduce delays in, and barriers to, diagnosis, treatment and supportive care.
Screening aims to identify individuals with findings suggestive of a specific cancer or pre-cancer before they have developed symptoms. When abnormalities are identified during screening, further tests to establish a definitive diagnosis should follow, as should referral for treatment if cancer is proven to be present.
Screening programmes are effective for some but not all cancer types and in general are far more complex and resource-intensive than early diagnosis as they require special equipment and dedicated personnel. Even when screening programmes are established, early diagnosis programmes are still necessary to identify those cancer cases occurring in people who do not meet the age or risk factor criteria for screening.
Patient selection for screening programmes is based on age and risk factors to avoid excessive false positive studies. Examples of screening methods are:
- HPV test (including HPV DNA and mRNA test), as preferred modality for cervical cancer screening; and
- mammography screening for breast cancer for women aged 50–69 residing in settings with strong or relatively strong health systems.
Quality assurance is required for both screening and early diagnosis programmes.
A correct cancer diagnosis is essential for appropriate and effective treatment because every cancer type requires a specific treatment regimen. Treatment usually includes surgery, radiotherapy, and/or systemic therapy (chemotherapy, hormonal treatments, targeted biological therapies). Proper selection of a treatment regimen takes into consideration both the cancer and the individual being treated. Completion of the treatment protocol in a defined period of time is important to achieve the predicted therapeutic result.
Determining the goals of treatment is an important first step. The primary goal is generally to cure cancer or to considerably prolong life. Improving the patient's quality of life is also an important goal. This can be achieved by support for the patient’s physical, psychosocial and spiritual well-being and palliative care in terminal stages of cancer.
Some of the most common cancer types, such as breast cancer, cervical cancer, oral cancer, and colorectal cancer, have high cure probabilities when detected early and treated according to best practices.
Some cancer types, such as testicular seminoma and different types of leukaemia and lymphoma in children, also have high cure rates if appropriate treatment is provided, even when cancerous cells are present in other areas of the body.
There is, however, a significant variation in treatment availability between countries of different income levels; comprehensive treatment is reportedly available in more than 90% of high-income countries but less than 15% of low-income countries (3).
Palliative care
Palliative care is treatment to relieve, rather than cure, symptoms and suffering caused by cancer and to improve the quality of life of patients and their families. Palliative care can help people live more comfortably. It is particularly needed in places with a high proportion of patients in advanced stages of cancer where there is little chance of cure.
Relief from physical, psychosocial, and spiritual problems through palliative care is possible for more than 90% of patients with advanced stages of cancer.
Effective public health strategies, comprising community- and home-based care, are essential to provide pain relief and palliative care for patients and their families.
WHO response
In 2017, the World Health Assembly passed the Resolution Cancer prevention and control in the context of an integrated approach (WHA70.12) that urges governments and WHO to accelerate action to achieve the targets specified in the Global Action Plan for the prevention and control of NCDs 2013-2020 and the 2030 UN Agenda for Sustainable Development to reduce premature mortality from cancer.
WHO and IARC collaborate with other UN organizations, inlcuing the International Atomic Energy Agency, and partners to:
- increase political commitment for cancer prevention and control;
- coordinate and conduct research on the causes of human cancer and the mechanisms of carcinogenesis;
- monitor the cancer burden (as part of the work of the Global Initiative on Cancer Registries);
- identify “best buys” and other cost-effective, priority strategies for cancer prevention and control;
- develop standards and tools to guide the planning and implementation of interventions for prevention, early diagnosis, screening, treatment and palliative and survivorship care for both adult and child cancers;
- strengthen health systems at national and local levels to help them improve access to cancer treatments;
- set the agenda for cancer prevention and control in the 2020 WHO Report on Cancer;
- provide global leadership as well as technical assistance to support governments and their partners build and sustain high-quality cervical cancer control programmes as part of the Global Strategy to Accelerate the Elimination of Cervical Cancer;
- improve breast cancer control and reduce avoidable deaths from breast cancer, focusing on health promotion, timely diagnosis and access to care in order to accelerate coordinated implementation through the WHO Global Breast Cancer Initiative;
- support governments to improve survival for childhood cancer through directed country support, regional networks and global action as part of the WHO Global Initiative for Childhood Cancer using the Cure All approach;
- increase access to essential cancer medicines, particularly through the Global Platform for Access to Childhood Cancer Medicines; and
- provide technical assistance for rapid, effective transfer of best practice interventions to countries.
(1) Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, et al. Global Cancer Observatory: Cancer Today. Lyon: International Agency for Research on Cancer; 2020 ( https://gco.iarc.fr/today , accessed February 2021).
(2) de Martel C, Georges D, Bray F, Ferlay J, Clifford GM. Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis. Lancet Glob Health. 2020;8(2):e180-e190.
(3) Assessing national capacity for the prevention and control of noncommunicable diseases: report of the 2019 global survey. Geneva: World Health Organization; 2020.
Cervical cancer
Cervical cancer country profiles
Cervical Cancer Knowledge Repository

Online Help
Our 24/7 cancer helpline provides information and answers for people dealing with cancer. We can connect you with trained cancer information specialists who will answer questions about a cancer diagnosis and provide guidance and a compassionate ear.
Chat live online
Select the Live Chat button at the bottom of the page
Call us at 1-800-227-2345
Available any time of day or night
Our highly trained specialists are available 24/7 via phone and on weekdays can assist through online chat. We connect patients, caregivers, and family members with essential services and resources at every step of their cancer journey. Ask us how you can get involved and support the fight against cancer. Some of the topics we can assist with include:
- Referrals to patient-related programs or resources
- Donations, website, or event-related assistance
- Tobacco-related topics
- Volunteer opportunities
- Cancer Information
For medical questions, we encourage you to review our information with your doctor.
You are not your cancer. Not even close. You are just you.
You deserve to feel like yourself during and after cancer treatment. At EverYou, you’ll find quality wigs, headwear, and recovery care products.

Every cancer. Every life.
We are a leading cancer-fighting organization with a vision to end cancer as we know it, for everyone. We are improving the lives of people with cancer and their families as the only organization combating cancer through advocacy, research, and patient support, to ensure that everyone has an opportunity to prevent, detect, treat, and survive cancer.

Be Safe in the Sun
Get tips to help you protect yourself and your family.

Cancer and Asian Americans, Native Hawaiians & Other Pacific Islanders
Get the facts.

Protect Your Child From 6 Types of Cancer
Call to schedule your child’s HPV vaccine today.

Give in Honor or Memory
Your loved one's legacy can be a cancer-free world.
Get Cancer Information Now
Cancer information and resources.
1 in 2 men and 1 in 3 women will be diagnosed with cancer in their lifetime. If you’ve been recently diagnosed, or know someone who has, we’re here with answers, guidance, and support.
Understanding Cancer
Managing cancer care, survivorship, caregivers & family, find support & resources, services for you.
The American Cancer Society offers all kinds of support for patients, families, and caregivers.

When cancer treatment is far from home, our Hope Lodge facilities offer a free place to stay and a supportive space to rest. We also provide lodging grants to local healthcare systems partners so they can provide lodging assistance to their patients.

Rides and Transportation
Road to Recovery connects cancer patients in need of transportation to treatment with volunteers to get them there. We also provide transportation grants to local healthcare systems partners to provide transportation assistance to their patients.

All Patient Programs and Services
Connect with American Cancer Society staff or others who are facing cancer for information and support.
Overall Impact of the American Cancer Society
Help us end cancer as we know it, for everyone. Donate now to improve the lives of people with cancer and their families through advocacy, research, and patient support.
lives touched in 2023
invested in research since 1946
cancer survivors alive today
cancer screenings in underserved communities
rides to treatment
free lodging nights provided
Help us continue our work
Risk, prevention, and screening.
You can help reduce your risk of cancer by making healthy choices like eating right, staying active, and not smoking. It's also important to follow recommended screening guidelines, which can help detect certain cancers early.
Eat Healthy and Get Active
Learn about the benefits of good nutrition, regular physical activity, and staying at a healthy weight.

Stay Away From Tobacco
Let the Great American Smokeout event be your day to start your journey toward a smoke-free life.
HPV Prevention
Human Papillomavirus can cause 6 types of cancer. But preventing it — and the cancers it causes — is simple.
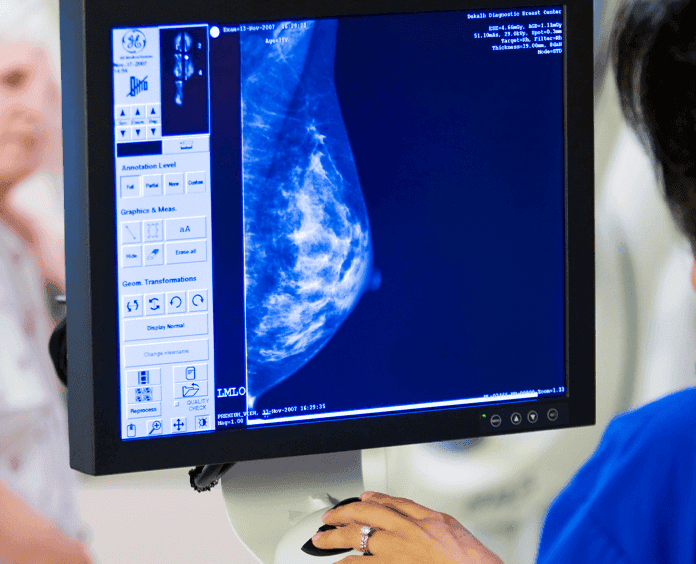
Get Screened
Learn about recommended cancer screening tests and find resources to help you get on a screening schedule that's right for you.
Supporting Families and Caregivers
A cancer diagnosis affects close family and friends too. Find out what to expect if you become a caregiver for a person with cancer, and get tips for making sure that you take care of yourself as well.

Volunteer and Fundraise
We couldn’t do what we do without our volunteers, fundraisers, and donors. Together, we’re making a difference – and you can, too. Become a volunteer, make a tax-deductible donation, or participate in a fundraising event to help us save lives.

Volunteer Opportunities
Be part of the movement to save lives and celebrate life. Every single day.

Relay For Life
Join the world’s largest volunteer-based fundraising event.

Making Strides Against Breast Cancer
Support the walk that unites more than 150 communities every year.
Fundraise Your Way
Learn about the endless new and creative opportunities to raise funds or get involved with the American Cancer Society.

American Cancer Society Cancer Action Network
Fight together to influence public policy and make cancer a national priority.

Volunteer and Fundraising Impact
Our fundraising events are key to fighting for our mission and building a supportive cancer community. Our community events and patient services are funded entirely by donations.
Relay For Life participants globally
raised through RFL and MSABC since 1985
CEOs of U.S. companies engaged in our mission
Participate in a Volunteer or Fundraising Activity
Research that saves lives.
What does it take to outsmart cancer? Research. We’ve invested more than $5 billion in cancer research since 1946 , all to find more – and better – treatments, uncover factors that may cause cancer, and improve cancer patients’ quality of life.

Surveillance & Health Equity Science
We CONDUCT and publish research on cancer prevention, surveillance, health services, and disparities. Publications include Cancer Facts & Figure reports.

Population Science
We CONDUCT and publish research about cancer risk factors, the quality of life, and cancer survivors through Cancer Prevention Studies (CPS), including CPS-II and CPS-3.

Extramural Discovery Science
We FUND high impact and innovative research for any type of cancer and from bench to bedside by supporting scientists across the United States with research grants.
Survivor Journeys
Numbers only tell part of the story. Meet the people who are living proof of our mission.

Survivor, Breast Cancer
Survivor, Colon & Kidney Cancer

Survivor, Colon Cancer
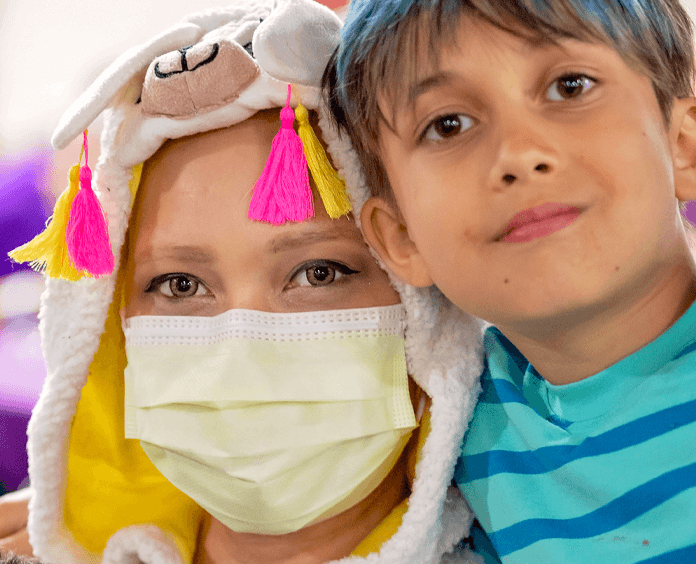
Survivor, Ovarian Cancer
Sign Up for American Cancer Society Emails
Stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.
Thank you, Firstname
Thank you for signing up for American Cancer Society emails.
Help us end cancer as we know it, for everyone.

Explore CRI’s 2023 Cancer Research Impact
Cancer Patient Resource Websites
Finding the answer to your cancer requires many different resources. If you are dealing with or diagnosed with cancer, it is important to have information to make informed choices about your treatment options. The websites listed below are valuable sources of cancer information for patients and their families, including support and advocacy groups and financial assistance programs.
Information on the novel coronavirus (COVID-19)
Cancer.net Recommendations for cancer patients
Centers for Disease Control and Prevention (CDC) Latest public health recommendations and guidelines
National Cancer Institute (NCI) Emergency and preparedness. For up-to-date information and recommendations for people with cancer during the rapidly evolving COVID-19 situation
World Health Organization (WHO) Latest global health news and basic protective measures
Helpful links for cancer information
American Cancer Society Organization providing cancer information, educational programs, and community outreach, both nationally and internationally
American Medical Association “DoctorFinder” Professional information on over 690,000 licensed physicians in the U.S. Search for doctors by name, medical specialty, and zip code
Association of American Cancer Institutes Site includes directory of member cancer research centers, an annual report, and information on current initiatives
CancerCommons 1-on-1 support, free of charge, to find the best options for your advanced cancer with a team of nurse navigators, PhD scientists, physicians, and national experts
Cancer.net Patient information from the American Society of Clinical Oncology that includes cancer types, treatments, survivorship, advocacy, and resources
Centers for Disease Control and Prevention Comprehensive information on cancer and many other health and safety topics, including a resource library and links to publications and reports. Site also offers recommendations on preventive cancer screening
Drugs.com Search for information on both over-the-counter and prescription drugs, including new drug approvals.
MedlinePlus U.S. National Library of Medicine and National Institutes of Health site with comprehensive health education, drug information, and medical news
National Cancer Institute Part of the U.S. National Institutes of Health. Comprehensive site with information on cancer types, topics, and statistics as well as clinical trial enrollment and results. Also includes Physician Data Query (PDQ) database of summaries on cancer treatments and related issues.
The National Health Information Center (NHIC) U.S. Department of Health and Human Services site with health information and searchable resource database to link people to health organizations and government offices with the information they need
OncoLink Associated with the Abramson Cancer Center of the University of Pennsylvania. Offers information on types of cancers and treatments, coping resources, “Ask the cancer expert” feature, and an online library.
PDRHealth Provides disease education, treatment options, and clinical trial information for cancer and many other topics. Also supplies comprehensive information on prescription and over-the-counter drugs as well as herbal medicines and nutritional supplements.
Financial and legal assistance programs
CancerCare A national nonprofit organization that provides free, professional support services for anyone affected by cancer
Cancer and Careers A national nonprofit that empowers and educates people with cancer to thrive in their workplace, by providing expert advice, interactive tools, and educational events
Hill-Burton Free and Reduced-Cost Health Care Facilities that offer services at no or reduced cost upon eligibility, application, and acceptance according to U.S. Department of Health and Human Services guidelines
Social Security Disability (SSDI) A federal insurance program managed by the Social Security Administration and designed to provide income supplements to people who are physically restricted in their ability to be employed
Lazarex Patient navigators that can help you with the costs associated with participating in a clinical trial, including transportation, lodging, and certain medical expenses not covered by insurance and necessary for clinical trial treatment
Ronald McDonald House A “home-away-from-home” for families so they can stay close by their hospitalized child at little or no cost with home-cooked meals, private bedrooms, and playrooms for children
Triage Cancer A national, nonprofit organization that provides education on the practical and legal issues that may impact individuals diagnosed with cancer and their caregivers
Emotional support services
Cancer Support Community Free comprehensive integrative care—including counseling, support groups, nutrition, exercise, and patient education programs—for people with cancer and their families or caregivers
Gilda’s Club New York City Programming of free emotional and social support for everyone living with cancer, including yoga workshops, educational programs, and knitting and crochet circle workshops
Imerman Angels A cancer support community that provides personalized one-on-one connections among cancer patients, survivors, and caregivers
National Coalition for Cancer Survivorship A nonprofit advocate for quality cancer care for all people touched by cancer
Nursing at Georgetown: Managing Mental Health After a Cancer Diagnosis Georgetown University discusses the emotional heaviness that a patient might experience following a cancer diagnosis. The three main topics covered are distress, depression and anxiety, but this article encourages an open dialogue for any mental illness that may come from such a heavy life experience.
Cancer-specific resources
Colorectal Cancer Alliance Organization that empowers allies to provide genuine supportfor patients and families, caregivers, and survivors; to raise awareness of preventive measures; and inspire efforts to fund critical research
Facing Our Risk of Cancer Empowered (FORCE) Organization to improve the lives of individuals and families affected by hereditary breast, ovarian, and related cancers
LUNGevity Organization that offers peer-to-peer support through our mentor program and online message board, opportunities to connect with other patients, survivors, and caregivers in private Facebook groups and weekly Virtual Meetups, and a HELPLine staffed by oncology social workers
The Lung Cancer Research Foundation (LCRF) Organization that provides print and digital materials for patient/caregiver education as well as tools for healthcare professionals
Melanoma Research Foundation (MRF) Find educational resources and support services for melanoma, including the Melanoma Patient Guide, Patient and Caregiver Meetings, and Financial Assistance
National Ovarian Cancer Coalition (NOCC) Organization educating communities and increasing awareness about ovarian cancer
Patient Empowerment Network (PEN) Actionable advice and downloadable resources to help you communicate clearly and effectively with your healthcare team
SHARE Organization that supports, educates, and empowers women affected by breast, ovarian, uterine, or metastatic breast cancer, with a special focus on medically underserved communities
Stupid Cancer Leading national advocacy organization serving the adolescent and young adult (AYA) cancer community
Us TOO Organization with more 200 support groups throughout the U.S. and abroad that help men and their families make informed decisions about prostate cancer
Medical literature and scientific organizations
Cancer Immunology Research An academic journal published monthly by the American Association of Cancer Research (AACR), in collaboration with the Cancer Research Institute, reporting major advances in cancer immunology that span basic investigations in host-tumor interactions to developmental therapeutics in model systems, early translational studies in patients, and clinical trials.
National Academy of Sciences Society of distinguished scholars in scientific and engineering research, including members of the CRI Scientific Advisory Council
PubMed U.S. National Library of Medicine Searchable catalog of medical articles. Covers medical literature from the 1950s to the present.
U.S. National Library of Medicine Part of the National Institutes of Health. Site provides health news bulletins on different medical conditions including cancer and the history of medicine.
Related Links
Additional Resource
If you would like to tell us about other helpful sites that we could consider for this page, please contact us.
This website uses tracking technologies, such as cookies, to provide a better user experience. If you continue to use this site, then you acknowledge our use of tracking technologies. For additional information, review our Privacy Policy .
Every print subscription comes with full digital access
Science News
A long-awaited cancer treatment reaches patients.

By Erin Wayman
Managing Editor, Print and Longform
10 hours ago
Share this:
Thanks to the pandemic, the immune system has gotten a lot of attention. When I think about all the viruses, bacteria and other invaders that the body’s defenses fend off, I’m in awe, even if the nudge of a vaccine is sometimes needed to help mount the counterattack.
This issue’s cover story reminds me of another reason to be in awe: The immune system not only protects against foreign threats but homegrown ones as well. On Page 22, senior writer Meghan Rosen describes a recent breakthrough in wielding the immune system against cancer. Earlier this year, the U.S. Food and Drug Administration approved the first T cell therapy for a solid tumor , sold under the name Amtagvi. To treat advanced melanoma, doctors remove tumor-infiltrating lymphocytes, a type of T cell known as TILs, from a patient’s own tumor and grow these natural cancer killers by the billions in the lab. Then the battalion of T cells is injected into the patient to improve the body’s odds of beating the cancer.
Oncologist Steven Rosenberg of the U.S. National Cancer Institute became intrigued by the body’s potential for fighting cancer in 1968 after encountering a patient whose tumors spontaneously disappeared, presumably due to the immune system. It took decades to go from that kernel of an idea to the new TIL therapy.
Rosenberg’s TIL therapy was an idea ahead of its time. In fact, it’s an idea whose foundation stretches all the way back to antiquity.
Early reports of cancer suddenly going into remission after an infection date back to ancient Egypt. By the 19th century, scientists began to piece together that an awakened immune system might be at play. In 1891, New York City bone surgeon William Bradley Coley put that idea to the test by infecting patients’ tumors with Streptococcus and Serratia bacteria. It appeared to work: Reportedly more than 1,000 patients saw their tumors shrink or even disappear. Many doctors, however, were wary of infecting people with potentially dangerous bacteria. Another concern was that no one really knew how or why Coley’s treatment worked. And so, cancer immunotherapy stalled.
But throughout the 20th century, scientists demystified the immune system (or at least began to; it’s still quite mysterious!). In 1967, for example, the year before Rosenberg’s realization, immunologists discovered the existence of T cells and their role in immunity. In the last decade or so, advances have translated into wins for cancer patients. In 2011, a class of drugs known as checkpoint inhibitors, which keep cancer-fighting immune cells in attack mode, first became available. In 2017, the FDA approved the first cancer treatment that uses genetically engineered T cells from patients, called CAR T-cell therapy. This form of treatment has successfully treated blood cancers, such as leukemia. Now with TIL therapy, solid tumors are a target.
So far, it’s approved only for advanced melanoma, but studies suggest TIL therapy may work against other kinds of solid tumors too. We’re far from the end of the story, with many lingering questions about how the immune system fights cancer. One big question: Why do therapies often work for some patients but not others? As answers come in, we’ll keep you updated.
Subscribers, enter your e-mail address for full access to the Science News archives and digital editions.
Not a subscriber? Become one now .
- Share full article
Advertisement
Supported by
How to Find the Right Oncologist for You
After a cancer diagnosis, it’s one of the most important decisions you’ll make.

By Ted Alcorn
After a career as a golf professional in southeastern New Mexico, Doug Lyle, 76, decided he had somewhere better to be than on the course: spending time with his new grandchild. Then this summer, just as he was settling into retirement, he learned he had prostate cancer.
“When you’re first diagnosed, you immediately go to the internet, and you can be overwhelmed in short order,” he said. “The more you read about it, the more complicated it gets.”
One of the first and most important choices he had to make was who his oncologist would be. Many of the two million patients diagnosed with cancer in the United States each year get the news from a primary care doctor. Those patients might accept a referral to an oncologist without question. But research suggests that it’s worth considering the choice closely: It can shape the care you receive , your satisfaction with the treatment and your chances of survival .
Scour the information available.
Not everyone has a choice of oncologists. There are fewer providers in rural areas, and patients must travel farther to reach them. Insurers may only cover certain clinicians and hospitals. And patients from certain populations have less access to oncologists for a range of reasons, which may affect the care they receive. For example, research suggests that Black and Hispanic women with breast cancer are more likely than white women to experience delays in starting radiotherapy. And Black men with prostate cancer are less likely than white men to receive treatment that’s intended to cure their condition, even when they’re at similar stages of disease.
No matter your circumstances, you should feel empowered to have a say in who treats your cancer.
Ideally, experts said, you’d be able to easily compare doctors’ levels of experience and the outcomes of patients they’ve treated with your same diagnosis. But such apples-to-apples comparisons are not always easy to make. But “right now, there are no publicly available data to help a patient with cancer say, ‘Oh, this is where I want to go,’” said Dr. Nancy Keating, a physician and professor of health care policy and medicine at Harvard Medical School. (And even if there were, apples-to-apples comparisons are not always easy to make, since patient populations vary from one doctor to the next).
Still, there are some accreditations to look for. The National Cancer Institute has given a special designation to 72 cancer centers , which must show they treat patients in accordance with the latest evidence and also conduct research into new therapies. The American College of Surgeons Commission on Cancer has accredited over 1,500 programs that meet certain standards. And the American Society of Clinical Oncology has several certification programs, including a list of 300 practices recognized for their quality and safety.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
August 23, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Using RNA splicing events to identify colon cancer subtypes is a more reliable and cost-effective method
by Leslie Orr, University of Rochester Medical Center
Researchers discovered an alternative way to classify distinct types of colon cancer, making the information more valuable to patients and their doctors as they consider treatment.
Currently, colon cancers can be classified into four subtypes based on gene expression patterns , yet this method can be unreliable and is very costly, scientists said.
In the new proof-of-concept study, a team at Wilmot Cancer Institute, collaborating with a German company, Indivumed Therapeutics, found that using RNA splicing events rather than gene-expression analysis offers more precise and lower cost tumor-type identification.
When a patient is diagnosed, this step—identifying the unique characteristics and molecular properties of tumors—is crucial to determining prognosis and what medications may work best to attack the disease.
Hucky Land, Ph.D., deputy director at Wilmot and chair of the University of Rochester Medical Center Department of Biomedical Genetics, is corresponding author of the article published in Gastroenterology .
He credits Aslihan Ambeskovic, Ph.D., lead bioinformatics analyst in the Land lab, for conducting most of the work using RNA sequencing data from hundreds of human colon cancer tissue samples. Matthew N. McCall, Ph.D., associate professor of Biostatistics, is also a co-author.
Calling the discovery "a significant advance based on biological principles that is highly translational," Land noted that the next step is to develop a diagnostic test suitable for the clinic.
Colorectal cancers have a complex landscape of genetic and epigenetic alterations. Some subtypes, for example, may respond better to immunotherapy while certain chemotherapy regimens may be the correct approach for other subtypes.
Researchers believe their newly discovered subtype identifier is accurate and reliable because variation in RNA splicing holds more relevant information in each cancer specimen.
Explore further
Feedback to editors

Study identifies metabolic switch essential for generation of memory T cells and anti-tumor immunity
15 hours ago

Multiple sclerosis appears to protect against Alzheimer's disease
Aug 23, 2024

Good sleep habits important for overweight adults, study suggests

Mediterranean diet supplement can affect epigenetics associated with healthy aging

New method for quantifying boredom in the body during temporary stress

Cancer researchers develop new method that uses internal clock inside tumor cells to optimize therapies

Strength training activates cellular waste disposal, interdisciplinary research reveals

Being a 'weekend warrior' could be as good for brain health as exercising throughout the week

Simple blood test for Alzheimer's disease could change how the disease is detected and diagnosed

Chlamydia can settle in the intestine, organoid experiments reveal
Related stories.

Genetic signatures provide prognostic information in colorectal cancer
Aug 7, 2024

Transcription factors found to contribute to subtypes of colorectal cancers
Jul 27, 2023

When tumors collide: Analysis of mixed-type breast cancer reveals complexity
Jul 24, 2024

Homing in on shared network of cancer genes
Dec 21, 2021

Researchers identify novel gene networks associated with aggressive type of breast cancer
Apr 24, 2024

Identifying cancer genes' multiple personalities
Apr 10, 2023
Recommended for you

AI platform enhances lung cancer diagnosis accuracy

Researchers identify piRNAs as a highly relevant genetic cause of male infertility

Faulty gene makes the brain too big—or too small

A new culprit in Huntington's: Brain organoid model implicates gene in disease progression
Aug 22, 2024

Reading your biological age in your blood or saliva? It's not as simple as that, study shows
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cancers (Basel)

Physical Activity and Cancer Care—A Review
Weronika misiąg.
1 Student Research Club No. 180, Faculty of Medicine, Wroclaw Medical University, 50-367 Wroclaw, Poland
Anna Piszczyk
Anna szymańska-chabowska.
2 Department of Internal Medicine, Occupational Diseases, Hypertension and Clinical Oncology, Wroclaw Medical University, 50-556 Wroclaw, Poland
Mariusz Chabowski
3 Department of Nursing and Obstetrics, Faculty of Health Science, Wroclaw Medical University, 51-618 Wroclaw, Poland
4 Department of Surgery, 4th Military Teaching Hospital, 50-981 Wroclaw, Poland
Associated Data
All the data analysed during the current study are available from the corresponding author upon reasonable request.
Simple Summary
The aim of this paper is to outline the role and potential benefits of physical activity for cancer patients. We present a review of publications on the subject in order to compare the findings reported in the literature and draw general conclusions that could help clinicians who provide cancer care to develop a more comprehensive treatment approach. This review may also help patients overcome barriers and become more motivated to take up physical activity, which would improve their quality of life. We wish to demonstrate to patients that physical activity should not be regarded as a burdensome medical recommendation but rather as a factor that can reduce the risk of cancer mortality and recurrence.
In 2020, 19.3 million new cancer cases were diagnosed, and almost 10 million deaths from cancer were recorded. Cancer patients may experience fatigue, depression, anxiety, reduced quality of life and sleep problems. Cancer treatments cause numerous side effects and have a negative impact on all body systems. Physical activity is important for cancer patients. The aim of this review is to analyse recent studies on the role of physical activity in cancer patients and emphasize its importance. The review included 36 papers published in English between 2017 and 2021. The findings from these studies show that physical activity decreases the severity of side effects of cancer treatment, reduces fatigue, improves quality of life, has a positive impact on mental health and improves aerobic fitness in cancer patients. Moreover, it reduces the risk of cancer recurrence and death. Physical activity is recommended for patients with any type of cancer and at all stages of treatment. The type of physical activity should depend on the condition of the individual patient. It is extremely difficult to determine what type, intensity and duration of physical activity is likely to have the greatest effect.
1. Introduction
In 2020, 19.3 million new cancer cases were diagnosed, and almost 10 million deaths from cancer were recorded [ 1 ]. Cancer patients may experience fatigue, depression, anxiety, reduced quality of life (QoL) and sleep problems [ 2 , 3 , 4 ].
Cancer treatments have many side effects. They exert a negative impact on: the cardiovascular system, the endocrine system, the digestive system, the immune system, the nervous system, the respiratory system, systemic symptoms such as fatigue, which can persist for many years after treatment, and lymphedema [ 5 ].
Physical activity (PA) is important for cancer patients. The World Health Organization distinguishes between two types of physical activity: aerobic physical activity and anaerobic physical activity. Physical activity can be classified according to intensity as: light-intensity physical activity, 1.5–3 metabolic equivalents of task (METs), which does not result in a significant increase in heart rate or respiratory rate (one example of light-intensity physical activity is slow walking); moderate-intensity physical activity, 3–6 METs; and vigorous-intensity physical activity, more than 6 METs [ 6 ].
PA improves QoL, increases aerobic fitness, has a positive influence on mental health and reduces the side effects of cancer treatment, fatigue and mortality in cancer patients [ 2 , 3 , 7 , 8 , 9 ]. The type of physical activity should depend on the condition of the individual patient. A patient’s response to a given physical activity stimulus may vary due to the side effects of treatment, demographic factors (age), mobility restrictions or comorbidities [ 10 ]. However, patients should undertake physical activity unless the disturbances are severe enough to prevent them from exercising [ 11 ]. Moreover, a patient’s ability to tolerate exercise may vary during a disease. This is caused by the variability in the intensity of the symptoms [ 5 ].
With patients facing a life-threatening illness, recommending additional physical activity may seem to be unnecessarily burdensome or too simplistic, as it would require an investment of time and energy from the patient [ 10 ].
Although there are many research papers about the benefits of physical activity in cancer patients, in practice combining PA with treatment is rare. In 2020, as many as 35.5% of the cancer survivors aged 18 years and older reported physical inactivity [ 12 ]. Only 7% of cancer patients perform adequate exercises [ 13 ]. This manuscript analyses the recent studies from the last five years on the role of physical activity in cancer patients under active treatment and cancer survivors and emphasize its importance. The review summarizes the results gathered from 36 articles and presents the influence of PA in cancer care for different types of tumour and patient groups.
The aim of the study is to present the impact of physical activity on cancer patients and cancer survivors in order to reach the largest possible group of readers, both among healthcare professionals and oncological patients.
2. Material and Methods
We conducted a search of articles in the PubMed, Web of Science and EBSCO Information Services using the following keywords: cancer care, physical activity, survivors, quality of life, QoL. The inclusion criteria were as follows: articles in English, publication between 2017 and 2022. A total of 971 records were initially identified. We removed 381 duplicates and excluded articles to which we had no access, articles in a language other than English and articles not directly related to the subject of the review ( n = 326). During the eligibility assessment, we also excluded articles concerning cancer prevention, since the aim of this review was to evaluate the role of physical activity in patients already diagnosed with cancer, as well as articles with insufficient data ( n = 228). Thirty-six articles were ultimately identified as eligible for inclusion. These publications were meta-analyses, systematic reviews and randomised controlled trials. The identification process of eligible studies is shown in Figure 1 . Patient-reported outcomes were assessed using Functional Assessment of Cancer Therapy Scale (FACT) with a subscale for fatigue (FACT-F) [ 8 ]. The FACT Measurement System consists of over 250 questions, and it measures health-related QoL in patients with cancer and other chronic diseases. Patients are asked to answer about 60 questions, based on the general version FACT-G, then new questions could be added to focus specifically on the problems of a given disease [ 14 , 15 , 16 ].

Identification of studies via databases.
We carried out a review of 36 systematic reviews, meta-analyses and randomised controlled trials concerning physical activity and cancer care. The studies included in the review investigated the effects of physical activity, as measured by a number of questionnaires assessing the type, frequency and duration of particular activities. We presented the results in Table 1 . This table compares the influence of physical activity on cancer patients: both survivors and patients under active oncology treatment. It shows results depending on: the type of cancer, type of intervention and its intensity and the frequency and duration of PA. The main findings in Table 1 describes if the cancer care with PA is superior to the usual care of these patients. This paper presents the findings from studies investigating the impact of physical activity on particular areas of life in cancer patients, such as: QoL, mental health, physical fitness, muscle strength and impact on body weight. The survey describes the impact of PA on side effects, fatigue, mortality, survival and recurrence of cancer. A summary of the key points is presented in Figure 2 .
Comparison of the influence of physical activity on cancer survivors.
| Author (Ref.) | Type of Cancer, Number of Patients | Intervention Type, Intensity | Frequency, Duration | Main Findings |
|---|---|---|---|---|
| Singh B. et al. [ ] | colorectal cancer ( = 670) | supervised and unsupervised aerobic and combined exercise | pre-treatment supervised: 1 session per week, unsupervised: 3–7 times per week for 4 weeks; during chemotherapy and post-treatment: from 1 to 7 sessions per week for 7 days to 6 months. | Superior to UC for: QoL, aerobic fitness, sleep, fatigue, reduced body fat, depression, upper-body strength ( < 0.05) |
| An K-Y. et al. [ ] | breast cancer ( = 301) | CARE | 25–30 min of aerobic exercise ( = 96), 50–60 min ( = 101), a combined dose of 50–60 min of aerobic and resistance exercise ( = 104), median of 17 weeks | The “combined” group was superior for: fatigue, upper and lower body endurance, body fat percentage—12-month follow up, CARE after chemotherapy may be optimal for longer-term health outcomes |
| Cannioto R.A. et al. [ ] | breast cancer ( = 1340) | DELCaP [ ] | from minimum PAGAs (the MET [ ] hour equivalent of 150 min to moderate intensity RPA per week) to exceeding the minimum recommended range | 1 year after diagnosis: reduction in recurrence and mortality |
| Parker N.H. et al. [ ] | pancreatic cancer ( = 50) | aerobic exercise, full-body strengthening exercises | 60 min/week—moderate intensity aerobic PA; 60 min/week of strengthening exercises, 7–25 weeks | Exercise recommendations for cancer survivors are important, but in order to reduce barriers to participation, further efforts are needed. |
| Dieli- Conwright C.M. et al. [ ] | breast cancer ( = 100), overweight and obese survivors | combined aerobic and resistance exercise | 16 weeks, 150 min of aerobic exercise with 2–3 days of resistance exercise training/week | Superior to usual care for QoL, fatigue, depression, muscular strength ( < 0.001). Three-month follow-up: outcomes remained improved. |
| Li W et al. [ ] | childhood cancer ( = 222) | adventure-based training program: ice-breaking and teambuilding games, shuttle runs, rock climbing, high- and low-level rope courses and descending | 4 training days: 2 weeks, 2, 4, and 6 months after randomisation | Significantly lower levels of CRF ( < 0.001), higher levels of physical activity ( < 0.001), QoL ( < 0.01) |
| Jones T.L. et al. [ ] | ovarian cancer (20 articles with sample sizes from 10 to 7022) | aerobic | 3 to 26-week intervention, from 75 min/week to 225 min/week | Higher health-related QoL, decreased levels of anxiety and depression, improvement in fatigue, physical and psychological health |
| Galvao D. et al. [ ] | prostate cancer with bone metastases ( = 103) | resistance, aerobic, flexibility exercise | 3 times per week, 60 min session, for 3 months | After 3 months—improved self-reported physical function, muscle strength. No changes for total body fat mass, fatigue ( = 0.964). |
| Cataldi et al. [ ] | breast cancer ( = 3) | each session: cardiorespiratory, resistance, flexibility, postural education exercises | 8-week programme, 60 min of exercise, 2 days per week | Measures of fatigue have decreased ( < 0.001), exercises improved physical fitness, functional capacity, capability to manage emotional life ( = 0.003), helped with dealing with the physiological and psychological side effects. |
| Di Maso et al. [ ] | prostate cancer ( = 777) | occupational and recreational physical activity and Mediterranean diet | 15-year follow-up | Intervention reduces mortality in PCa patients (due to lowering serum insulin levels, IGF and inflammation). |
| Wang et al. [ ] | non-metastatic prostate cancer ( = 10,864) | recreational physical activity, e.g., walking, bicycling, aerobics, dancing, jogging, tennis | MET-h/week < 3.5, 3.5–8.75, 8.75, ≤17.5, >17.5 | 37% lower risk of PCSM among men with lower-risk tumours (Gleason score 2–7, T1–T2, = 0.02), 31% lower risk of PCSM (>17.5 vs. 3.5 ≤ 8.75 MET-h/week)—no difference observed by tumour risk category |
| Dieli-Conwright C.M. et al. [ ] | overweight and obese survivors of breast cancer ( = 100) | aerobic, resistance exercise | 3 times per week for 16 weeks | Improved levels of insulin, IGF-1, leptin, adiponectin, BMI, skeletal mass index. At 3-month follow-up, all variables remained improved. |
| Tubiana-Mathieu N. et al. [ ] | breast cancer ( = 138) | CPET, 6MWT- 6-min walk test | 6 min | 6MWT allows for the calculation of the required exercise intensity |
| Watson G.A. et al. [ ] | Colorectal cancer ( = 832, = 573) breast, colon cancer (multiple systematic reviews) | aerobic and resistance training | 150 min of moderate intensity aerobic exercise in 3–5 sessions per week; resistance training—at least 2 days per week for 6–12 weeks | PA: reduces mortality and risk of recurrence in cancer survivors; improves QoL, allows maintaining a healthy weight, decreases fatigue. |
| Rogers L.Q. et al. [ ] | breast cancer ( = 222) | BEAT Cancer—physical activity behaviour change intervention | PA recommendations from American Cancer Society, 12 supervised exercise sessions for the first 6 weeks, then unsupervised home-based exercises, >150 min/week of moderate to vigorous PA, 3- and 6-month follow-up | BEAT Cancer was superior to usual care for improvement in sleep quality ( < 0.01) |
PA—physical activity; CARE—Combined Aerobic and Resistance Exercise; DELCaP—Diet, Exercise, Lifestyle and Cancer Prognosis Study; PAGA—Physical Activity Guidelines for Americans; RPA—recreational physical activity; MET—metabolic equivalent of task (minutes/hours); PCa—prostate cancer; PCSM—prostate-cancer-specific mortality; CRF—cancer-related fatigue.

A graphical abstract summarizing the presented results.
3.1. Side Effects of Cancer Treatment
Chemotherapy and radiotherapy inhibit physical activity due to their side effects, such as severe fatigue, lack of energy as well as hair loss and mental health problems [ 17 ]. Chemotherapy is more likely than chemoradiotherapy to cause fatigue and reduce motivation to exercise. While chemoradiotherapy involves a more intensive treatment schedule, it is better tolerated by patients [ 18 ]. Physical activity has been shown to reduce the side effects of treatment and fatigue in cancer patients. The reduction was seen in those patients who, despite the side effects of treatment, underwent physical activity [ 7 ]. Studies report that regular PA reduces disease-specific side effects in patients with MM [ 19 , 20 ]. However, there is no evidence that physical activity mitigates the cardiotoxicity induced by cytostatic drugs [ 21 ].
3.2. Fatigue
One study included in the review found that regular physical activity combined with an appropriate diet (the patients completed 71% of the aerobic exercise sessions of 41 ± 25 min and 58% of the resistance exercise sessions planned as part of the intervention) reduced the fatigue resulting from intensive cancer treatment. The QoL was improved as well as lower limb muscle mass and endurance in breast cancer patients undergoing chemotherapy or radiotherapy. An important finding from the study was that the beneficial effect on QoL and fatigue persisted one year after the intervention [ 2 ]. Combined aerobic and resistance exercise has been found to reduce fatigue in patients with breast cancer [ 8 ]. In a study by Singh et al. [ 3 ], analysing the findings from 19 clinical trials, physical activity was observed to have a significant effect on fatigue in patients with colorectal cancer as compared with usual cancer care. Physical activity reduces the level of fatigue in cancer patients. The association between exercise and reduced fatigue has been demonstrated in patients with breast, prostate, colon and lung cancers [ 4 ]. Moreover, moderate-intensity physical activity has been found to reduce cancer-related fatigue in patients with colorectal cancer [ 22 ].
3.3. Quality of Life
Physical activity improves physical and social QoL and reduces anxiety and depression in cancer patients [ 2 , 3 ]. Unlike moderate to vigorous intensity physical activity, sedentary time negatively affects QoL and wellbeing of cancer patients [ 4 ]. Findings from one randomised controlled trial showed that aerobic and resistance exercise improves QoL by reducing depression, fatigue and physical deconditioning, which are the most common symptoms reported by breast cancer survivors [ 23 ]. Combined aerobic and resistance exercise performed during chemotherapy results in better longer-term QoL outcomes in breast and colorectal cancer patients, improving sleep quality, reducing anxiety and depression and having a positive impact on happiness [ 3 , 8 ]. Our review also included studies investigating the effects of physical activity on QoL in paediatric cancer patients with the use of the Paediatric Quality of Life Inventory. The studies showed that exercise interventions significantly improved QoL in the patients [ 24 , 25 , 26 , 27 ], even patients with haematological malignancies such as multiple myeloma [ 28 , 29 , 30 ]. Physical activity has also been shown to improve QoL and reduce anxiety and depression in ovarian cancer patients [ 27 ]. The findings from one study indicated that physical activity improves QoL in cancer patients despite the bothersome side effects of cancer treatment [ 7 ].
3.4. Mental Health
Physical activity has a positive impact on the mental health of cancer patients and adds positivity to their daily life [ 7 ]. One study showed that aerobic, resistance and flexibility exercises undertaken by prostate cancer patients with bone metastases for 3 months resulted in self-reported improvements in physical functioning, which had a positive influence on the mental health of the patients studied [ 31 ]. Another study found that an 8-week exercise intervention programme consisting of twice-per-week sessions of 60 min of resistance, flexibility and cardiorespiratory exercises performed by patients with different types of cancer improved the capability of the patients to express positive emotions, improved their functional capacity and had a positive influence on their mental health [ 32 ].
3.5. Physical Fitness, Muscle Strength, Impact on Body Weight
Studies have shown that exercise improves aerobic fitness and upper-body strength and reduces BMI and body fat in colorectal cancer patients. The results of a meta-analysis conducted by Singh et al. showed a greater effect for exercise interventions lasting over 12 weeks and interventions conducted during chemotherapy in patients with colorectal cancer [ 3 ]. Combined aerobic and resistance exercise has been found to be associated with superior upper and lower body muscle endurance in breast cancer patients [ 8 ].
3.6. Mortality and Longer Survival
There is an association between greater physical activity and reduced mortality in colorectal, breast and prostate cancer patients, with 40–50% risk reductions observed among individuals undertaking physical activity [ 33 ]. A study by Palesh et al. found that engaging in moderate physical activity was associated with longer survival and reduced hazard of cancer-related mortality in patients with advanced breast cancer [ 34 ]. In their study, Di Maso et al. noted that only vigorous physical activity had the advantage over inactivity in terms of reduced risks of cardiovascular and cancer mortality [ 35 ]. The cohort studies referred to by the authors reported approximately 40% reduction in mortality from prostate cancer in physically active men. Physical activity has also been found to reduce the risk of mortality in breast and colorectal cancer patients [ 36 ]. Barnard et al. [ 37 , 38 ] reported that intense physical activity reduces insulin resistance and insulin levels, with greater effects observed for a combination of intense physical activity and a low-fat, high-fibre diet. One study reported that breast cancer patients who met the minimum physical activity guidelines (PAGAs) had lower hazards of mortality compared with physically inactive patients (HR = 0.74, 95%, CI = 0.56 to 0.96; HR—hazard ratio; CI—confidence interval) [ 9 ]. A cohort study carried out by Wang et al. [ 39 ] that investigated the effects of recreational physical activity in patients with non-metastatic prostate cancer found that engaging in ≥17.5 MET-h/week of recreational physical activity, compared with 3.5 ≤ 8.75 MET-h/week of recreational physical activity, was associated with a 31% lower risk of prostate cancer-specific mortality (HR 0.69, CI 95%, p = 0.006), with no differences between the TNM stage of a tumour.
3.7. Recurrence
Combined aerobic and resistance exercise reduces the incidence of metabolic syndrome in cancer survivors, particularly breast cancer survivors. Metabolic syndrome is a risk factor for breast cancer recurrence [ 23 , 40 ]. A randomised controlled trial conducted among 100 breast cancer survivors, assigned either to exercise or usual care, showed an improvement in BMI and levels of circulating biomarkers, i.e., insulin, IGF-1, adiponectin and leptin, in the exercise group after the exercise intervention. An improvement in all metabolic syndrome variables persisted at the 3-month follow-up in the exercise group. Another study found that breast cancer patients meeting the minimum PAGAs both before and after their diagnosis had >50% reduced hazards of recurrence in comparison with patients not meeting this minimum at either time point. The study also found reduced hazards of recurrence for patients not meeting the minimum physical activity guidelines prior to diagnosis but who reported meeting the guidelines after their treatment (2-year follow-up) [ 9 ].
4. Discussion
A diagnosis of cancer has a profound impact on the life of the patient. The fear of cancer progression, metastases and side effects of systemic treatment affects the quality of life as well as the mental and physical health of cancer patients. The anxiety, depression and bothersome somatic symptoms, such as fatigue, nausea, vomiting and hair loss, experienced by cancer patients significantly inhibit their physical activity. The barriers to undertaking physical activity faced by cancer patients are a very complex issue. They are associated with a number of factors. The nature, type and extent of cancer; the presence of metastases; cancer treatment and its side effects; the patient’s attitude to their illness and their coping strategy, as well as social and family support, have an enormous impact on the patient’s motivation and quality of life and thus their attempt to undertake regular physical activity. Moreover, cancer patients are often concerned that physical activity could have a negative impact on their illness, especially patients with diagnosed multiple myeloma, whom have the highest physical and mental impairments and a low QoL [ 20 , 45 ]. Furthermore, they are less willing to include exercise in their standard cancer treatment because of the fear that it will make them feel worse and due to a lack of knowledge of the benefits of physical activity. However, numerous studies have reported that standard cancer care combined with physical activity is superior to standard pharmacological care. Physical activity improves the daily functioning of cancer patients, reduces fatigue, side effects of intensive treatments, anxiety and depression and improves muscle endurance and mass, thereby allowing patients to perform their daily activities without difficulty. Moreover, the findings from the studies showed that physical activity is associated with a reduced risk of cancer of the breast, colon, stomach and endometrium (10–20% risk reduction). The studies manifest that PA reduces the risk of mortality by 40–50% for breast, colon and prostate cancers [ 33 ].
Cancer-related fatigue is a serious and complex problem that affects the quality of life and daily activities of cancer patients. Although, based on the results in the studies [ 2 , 3 , 4 ], it can be concluded that there is a correlation between fatigue and a tendency to have less PA, it cannot be considered as an unequivocal cause of decline in PA. Nevertheless, fatigue has a major impact on the functioning of cancer patients, and clinicians should aim to reduce fatigue levels. Numerous studies have shown that physical activity is associated with a significant reduction in fatigue in breast, colorectal, ovarian and prostate cancer patients and multiple myeloma patients [ 3 , 8 , 19 , 22 , 27 , 31 , 43 ]. A systematic review by Cataldi et al. found that aerobic exercise is more effective than other treatments in reducing cancer-related fatigue. Their review suggested that exercise should be performed at least 2 days per week for at least 8 weeks in order to achieve the best results and showed that the effects of low- to medium-intensity exercise did not differ between women and men [ 46 ].
According to the National Comprehensive Cancer Network (NCCN) and the American College of Sports Medicine (ACSM) (2018), physical activity improves QoL and physiological and psychological fitness in cancer patients [ 46 ].
Chemotherapy and radiotherapy have a negative impact on many aspects of the lives of cancer patients, reducing their interest in physical activity and decreasing the effectiveness of exercise. The side effects of treatment are bothersome, especially for patients with MM, and their intensity is much higher than people with other haematological cancers [ 20 , 47 ]. One study revealed that cancer patients found it very difficult to engage in physical activity in public places due to the side effects of their treatment, such as hair loss, as well as the fear of overheating and infection [ 17 ]. However, physical activity has been shown to reduce the side effects of cancer treatment. Importantly, the beneficial effect of an intervention involving physical activity in reducing such side effects of cancer treatment as fatigue persisted one year after the intervention [ 2 ]. Chemotherapy not only affects QoL and causes bothersome side effects, but it also has a direct impact on the patient’s physiology. It reduces mitochondrial function by impairing oxidative phosphorylation, resulting in sarcopenia. Moreover, it may reduce lung function [ 43 , 48 ]. It has been shown that aerobic exercise mitigates the impact of cancer treatment on physiological functions. Physical activity helps increase blood flow, activates the sympathetic nervous system, regulates the endocrine system and mobilises cytotoxic lymphocytes and NK cells, thus exerting antitumor effects. Moreover, it reduces the levels of lactate, which are a factor in promoting tumour growth [ 49 , 50 ].
The results from a study by Cannioto et al. [ 9 ] showed that breast cancer patients meeting the minimum guidelines for physical activity both before and after diagnosis had >50% reduced hazards of cancer recurrence and mortality. These findings are of great importance for the development of clinical oncology, as they suggest that clinicians should advise their patients to increase their physical activity immediately after a diagnosis, which would result in significant benefits. However, the benefits of regular engagement in physical activity are not only directly associated with cancer care but also translate into a reduced risk of comorbidities, improved cardiovascular function and physical fitness and thus improved wellbeing and better daily functioning.
Physical activity can improve immune system function by mobilizing leukocytes with increased functional capacities into the circulation. It helps with the elimination of dysfunctional T cells and improves the abundance of some T cell populations. PA may have an impact on CTLA-4 (inhibitory immune checkpoint) and provide to better response to immunotherapy in cancer patients [ 51 , 52 ].
As for incorporating exercise into cancer care and improving treatment outcomes, it is crucial to understand the role of the intensity, dose and mode of exercise in cancer patients. It is necessary to consider the individual needs of patients, the type of cancer they have as well as their treatment and health history. It has been found that the sooner physical activity is incorporated into a patient’s treatment plan after diagnosis, the more effective it is [ 53 ]. High-intensity exercise is not contraindicated for all cancer patients. Therefore, patients should not be restricted to exercise of low intensity. High-intensity exercise should be avoided by those who suffer from nausea and vomiting as well as those who have a blood clot related to a peripheral central catheter [ 54 ]. Positive effects of exercise are observed with sessions of at least 20 min on most days of the week (accounting for planned days of rest and unplanned days of inactivity [ 55 ] due to one of the following barriers: fatigue, pain, lack of motivation [ 54 ]). Recommendations from the ACSM, the NCCN and the Clinical Oncology Society of Australia (COSA) recommend participation in 150 min of moderate-intensity aerobic exercise, 3–5 sessions per week, as well as resistance training at least 2 days per week as part of a programme lasting 6–12 weeks [ 56 , 57 , 58 ]. It is also recommended that exercise interventions should, at least initially, be supervised by exercise trainers or physical therapists [ 59 ]. Cataldi et al. recommend increasing the quantity and quality of exercise in cancer patients by monitoring all parameters during exercise sessions. Persons responsible for cancer care should take into consideration the outcomes of studies on this subject, so as to best plan the intensity and volume of exercise for their patients [ 46 ]. Similarly, the World Cancer Research Fund (WCRF) and the American Institute for Cancer Research (AICR) recommend participation in at least 150 min of moderate-intensity exercise per week, including strength training exercises at least twice a week [ 60 ].
A major challenge for cancer patients is the very initiation of regular physical activity. This, in turn, is influenced by their strategy for coping with the illness. Strategies for coping with cancer can be constructive (e.g., fighting spirit, positive redefinition) or destructive (e.g., helplessness, hopelessness, anxious preoccupation). Choosing a constructive strategy will help initiate and maintain physical activity, whereas destructive strategies are a major barrier to the initiation of physical activity. The helplessness and anxiety associated with a diagnosis of cancer result in the patient giving in to the illness. This reduces the patient’s QoL, making it more difficult for them to maintain motivation for engaging in physical activity [ 61 ]. Other barriers to participation in physical activity reported by cancer patients include: fatigue, business and the associated lack of time [ 62 ], severe pain and social and environmental barriers—lack of an exercise partner, lack of exercise facilities, fear of injury, lack of willpower, lack of interest, lack of equipment and lack of experience [ 63 , 64 ]. A relatively large proportion of patients (approximately 17.9%) cite the lack of access to information about how to exercise and what type of exercise would be best for them as the reason for which they do not engage in physical activity [ 64 ]. Another reason why patients do not initiate physical activity is their concern that a given type of exercise is contraindicated for them due to their illness.
It is very difficult for patients to maintain the appropriate intensity of exercise, especially if they suffer from chronic comorbidities or experience bothersome side effects of cancer treatment. The occurrence of comorbidities such as hypertension, kidney disease, diabetes, liver disease or obesity is increasing in cancer survivors [ 65 ]. Obesity, which occurs particularly in colorectal and breast cancer survivors, increases the risk of heart diseases and hypercholesterolemia and has an influence on survival [ 66 ]. Attempts are being made to determine what training intensity would be most beneficial for such patients in terms of improving their QoL and maintaining their motivation for participating in physical activity. All members of the cancer care team should promote physical activity at all stages of cancer treatment. Exercise should be individualised, planned and tailored to the individual patient and adjusted to a specific type of cancer, as it offers major potential for reducing cancer morbidity and mortality [ 67 ]. Studies show that flexible time for PA sessions, low-cost and close location to home met with highest interest from patients and better compliance [ 20 ]. The literature discussed above suggests that physical activity has a significant multidimensional impact on the quality of life of cancer patients and plays a major role in improving cancer care, treatment outcomes, increasing survival time and reducing mortality in cancer patients. Therefore, it is important that clinical recommendations focus on educating patients and attempting to change their attitude to exercise [ 62 ]. It is extremely hard to find the best way to encourage patients to start and maintain physical activities. Nevertheless, the healthcare providers should aim to encourage patients to exercise. An adequate education and demonstration PA advantages may be the first step to motivate them. Healthcare professionals should devote their time to patients, list the barriers the cancer patients and cancer survivors are struggling with and should try to find a solution to reduce the barriers and recommend an appropriate intervention. Psychological help could be invaluable. The results presented in this study may be helpful to convince patients that PA can offer them many benefits for their QoL, everyday functioning and survival time.
5. Limitations
The study has potential limitations. The first limitation is the selection of articles only in English, which introduces a language bias. The reason for this limitation is the insufficient knowledge of other languages to discuss the results in the study with appropriate precision. The second limitation is exclusion of the papers which the authors had no access to, which may potentially have impact on the results. The third limitation is the lack of an unequivocal way to encourage patients to start and maintain PA. Our purpose is to motivate the authors of future studies to search for an effective method encouraging patients to exercise.
6. Conclusions
Physical activity improves quality of life, increases survival and reduces mortality, fatigue, side effects of treatment and the risk of recurrence.
Physical activity should be selected individually, depending on the type of cancer, treatment and comorbidities.
It is extremely difficult to determine what type, intensity and duration of physical activity is likely to have the greatest effect.
Funding Statement
This research received no external funding.
Author Contributions
W.M. wrote the manuscript; A.P. reviewed and drafted the manuscript; A.S.-C. analysed the data and supervised the manuscript; M.C. participated in supervision and project administration. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
You need to enable JavaScript to run this app.

IMAGES
COMMENTS
Treatment Research. A new cellular immunotherapy approach shrank tumors in 3 of 7 patients with metastatic colon cancer, in a small NCI clinical trial. Normal white blood cells from each patient were genetically engineered to produce receptors that recognize and attack their specific cancer cells.
The American Cancer Society (ACS) has helped make possible almost every major cancer breakthrough since 1946. Since then, we've invested more than $5 billion in cancer research, making us the largest nonprofit funder of cancer research in the United States, outside of the federal government. We remain committed to finding more - and better ...
Your donation to the American Association for Cancer Research helps our more than 58,000 members worldwide drive progress against cancer. The AACR is the first and largest cancer research organization. Our mission is to prevent and cure cancer through research, education, communication, collaboration, funding, and advocacy.
Clinical Research. Clinical research involves the study of cancer in people. These cancer research studies are further broken down into two types: clinical trials and observational studies. Clinical trials are research studies that involve an intervention, which is a treatment or change that may affect the results of cancer.These can lead to new treatments, care, and improved results for ...
Research Advances. The 2022 report includes data on new cancer cases and deaths plus a detailed examination of trends in pancreatic cancer and its subtypes. NCI joins the cancer community in advancing the goals of the National Cancer Plan as part of its research programs. Advances in technology and access to large volumes of data have led to ...
Population research (also known as epidemiological research) is the study of causes and patterns of occurrence of cancer and evaluation of risk. Population scientists, also known as epidemiologists, study the patterns, causes, and effects of health and diseases in defined groups. Population research is highly collaborative and can span the ...
Nature Cancer 2 , 245-246 ( 2021) Cite this article. Cancer therapies have evolved considerably in recent decades, substantially improving the quality of life and survival of patients with ...
Subsequently, cancer patients have a wide range of needs. This study aims to identify and synthesise cancer patients' views about areas where they need support throughout their care. A systematic search of the literature from PsycInfo, Embase and Medline databases was conducted, and a narrative.
The National Cancer Research Institute (NCRI) in the UK have also recently highlighted research into the short-term and long-term psychological impacts of cancer and its treatment as a key priority, following surveys of over 3500 patients, carers, and health and social care professionals .
Cancer care has advanced at an impressive pace in recent years. New insights into tumor immunology and biology, combined with advances in artificial intelligence, nano tools, genetic engineering ...
Patients' quality of life has become a major objective of care in oncology. At the same time, it has become the object of increasing interest by researchers, working with both quantitative and qualitative methods. Progress in oncology has enabled more patients to survive longer, so that cancer is increasingly often a chronic disease that ...
skaman306/Getty Images. A tiny group of people with rectal cancer just experienced something of a scientific miracle: their cancer simply vanished after an experimental treatment. In a very small ...
The research was funded by the National Institute of Cancer in France. Esophageal cancer This German study looked at 438 people with a type of cancer of the esophagus that can be treated with surgery.
Blinatumomab is a type of immunotherapy administered intravenously and brings a normal immune cell called a T cell close to a leukemia cell so it can destroy it. The Food and Drug Administration approved blinatumomab for patients in remission who have traces of cancer, also known as measurable residual disease (MRD)-positive.
The expanded approval of two HPV tests allows the patient to collect a vaginal sample themselves in a health care setting, rather than a health provider collecting a sample during a pelvic exam. The availability of a self-collection option in health care settings could help widen access to cervical cancer screening. Continue Reading >
This was a cross-sectional study conducted at the King Hussein Cancer Center (KHCC) in Amman, Jordan, between October 2019 and February 2020. According to the last available statistics in 2015, KHCC provides medical care to around 60.0% of all cancer patients in Jordan ( Abdel-Razeq et al., 2015 ).
Cancer is a leading cause of death worldwide, accounting for nearly 10 million deaths in 2020, or nearly one in six deaths. The most common cancers are breast, lung, colon and rectum and prostate cancers. Around one-third of deaths from cancer are due to tobacco use, high body mass index, alcohol consumption, low fruit and vegetable intake, and ...
Dedicated to helping people who face cancer. Learn about cancer research, patient services, early detection, treatment and education at cancer.org. ... We've invested more than $5 billion in cancer research since 1946, all to find more - and better - treatments, uncover factors that may cause cancer, ...
Association of American Cancer Institutes. Site includes directory of member cancer research centers, an annual report, and information on current initiatives. CancerCommons. 1-on-1 support, free of charge, to find the best options for your advanced cancer with a team of nurse navigators, PhD scientists, physicians, and national experts.
Thanks to NCI-funded research, patients with cancer have a greater number of therapeutic options than ever before, many of which are more effective and less toxic than earlier options. But more research is needed to ensure the most effective treatment possible, including better ways to use existing therapies in combination, while maintaining ...
In the last decade or so, advances have translated into wins for cancer patients. In 2011, a class of drugs known as checkpoint inhibitors, which keep cancer-fighting immune cells in attack mode ...
1. Introduction. Cancer and its treatments can affect every aspect of an individual's life, giving rise to a range of supportive care needs that can include informational, physical, practical, social, spiritual, psychological, and emotional requirements [].When left unaddressed, these needs can impact capacity to tolerate or adhere to treatment, capacity to engage in treatment decision ...
The National Cancer Institute has given a special designation to 72 cancer centers, which must show they treat patients in accordance with the latest evidence and also conduct research into new ...
And some is more clinical, seeking to translate basic information into improving patient outcomes. The programs listed below are a small sampling of NCI's research efforts in prostate cancer. The Cancer Biomarkers Research Group promotes research on cancer biomarkers and manages the Early Detection Research Network (EDRN). EDRN is a network ...
Researchers discovered an alternative way to classify distinct types of colon cancer, making the information more valuable to patients and their doctors as they consider treatment. Currently ...
Although there are many research papers about the benefits of physical activity in cancer patients, in practice combining PA with treatment is rare. In 2020, as many as 35.5% of the cancer survivors aged 18 years and older reported physical inactivity . Only 7% of cancer patients perform adequate exercises . This manuscript analyses the recent ...
We are pleased to offer this human-centered care to our patients undergoing treatments for cancer." — David Tom Cooke, Interim physician-in-chief, UC Davis Comprehensive Cancer Center DispatchHealth will assign two vehicles within a 25-mile radius of UC Davis Medical Center .Care will be furnished by a nurse practitioner or physician assistant, as well as a trained medical technician.
Resources for Patients. We offer authoritative information about your type of cancer as well as information on a wide range of cancer topics and the latest cancer research. Also find NCI-supported clinical trials. For your questions about cancer or help navigating the NCI website, please contact our information specialists.
This phase II trial tests how well pembrolizumab, carboplatin, paclitaxel and radiation works in treating patients with early stage anal cancer. Immunotherapy with monoclonal antibodies, such as pembrolizumab, may help the body's immune system attack the cancer, and may interfere with the ability of tumor cells to grow and spread.